Advanced-Platelet Rich Fibrin Assisted Papilla Reconstruction by Modified Beagle’s Technique- A Novel Approach
Rajaram Vijayalakshmi1, Ravi Sathyapriya2, Prakash Prashanthi3, Chellathurai Burnice4
1 Associate Professor, Department of Periodontics, Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
2 Ex-PG, Department of Periodontics, Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
3 Assistant Professor, Department of Periodontics, Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
4 Assistant Professor, Department of Periodontics, Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Rajaram Vijayalakshmi, Meenakshi Ammal Dental College and Hospital, Maduravoyal, Chennai, Tamil Nadu, India.
E-mail: srvijayalakshmi@rediffmail.com
The loss of key papilla in an unaesthetic zone and the presence of a “black triangle” depicts the requirement for papillary reconstruction. The complete reconstruction of lost papilla is unpredictable; therefore, retention of papilla is very important for aesthetics. There are many causes for loss of papillae and the establishment of “black triangle” between teeth. However, the most common cause is loss of periodontal support due to plaque-associated lesions. However, abnormaility in tooth shape, improper contours of the prosthetic restorations and traumatic oral hygienic procedures may also impact the interdental papilla. The loss of interdental papilla soft tissue causes difficulties in phonetics, aesthetic appearance and lateral food impaction. This case report deals with a variant method of Beagle’s technique 37-year-old systemically healthy male patient with the chief complaint of black space between the upper front teeth region, causing displeasing smile and food entrapment. Intraoral examination done with periodontal probe revealed the loss of 2 mm of interdental papilla. Patient was treated surgically with Advanced Platelet Rich Fibrin (A-PRF) membrane for papilla reconstruction in the upper anterior aesthetic zone.
Aesthetics, Black triangle, Interdental papilla
Case Report
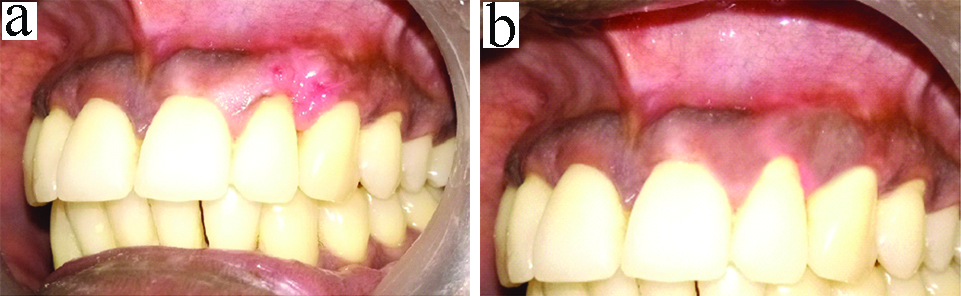
A 37-year-old systemically healthy male patient reported to Department of Periodontology, with the chief complaint of black space between the upper front teeth region, causing displeasing smile and food entrapment. Intraoral examination done with periodontal probe revealed the loss of 2 mm of interdental papilla- Nordland and Tarnow (1998) class I (The tip of interdental papilla lies between the interdental contact point and the coronal most extent of Cemento-enamel junction) between teeth 22 and 23 which was due to the periodontal support loss [Table/Fig-1a] [1]. Preoperatively the Papilla Presence Index (PPI) score was 2 (Cordropoli et al., 2004) and mesiodistal defect width was 2 mm [1]. Radiographic and haematological investigations were done prior to the surgery [Table/Fig-1b]. The treatment was planned as papilla reconstruction between teeth 22 and 23 by modified Beagle’s technique with A-PRF membrane. Informed consent was obtained from the patient [2]. Patient underwent scaling and root planing in phase I therapy, followed by surgical therapy.
a) Pre-operative view showing loss of interdental papilla; b) IOPA of 22, 23 region showing periodontal loss.

A-PRF Preparation
Before preparing the surgical site, 10 mL of intravenous blood was withdrawn by a venipuncture of the antecubital vein for A-PRF preparation. Collected blood was immediately centrifuged in a pre-programmed centrifuge (REMI) at 1500 rotations/minute for 14 minutes resulting in three layers wherein the top layer consisted of supernatant serum, the middle layer was of fibrin clot, the bottom layer contained Red Blood Corpuscles (RBCs). The fibrin clot was separated from the RBC base (keeping intact small RBC layers) by sterile tweezers and scissors. A-PRF membrane was procured by compressing the fibrin clot in the PRF box [Table/Fig-2a-d] [3].
a) Centrifuging Machine; b) PRF box; c) A-PRF gel in PRF box, d) A-PRF membrane.

Surgical Technique
The surgical procedure was performed using local infiltration anaesthesia (2% lignocaine with 1:80,000 concentration of adrenalin) in relation to 22, 23 interdental papillary region. Modified Beagle’s technique was used and incisions were given [Table/Fig-3a] at the adjacent line angles of the interdental papilla through an ophthalmic crescent knife, such that the length of the flap exceeded the length of the black triangle space to be reconstructed [4]. Full thickness mucoperiosteal flap was elevated with one horizontal and two vertical releasing incisions in 22, 23 interdental papillary region [Table/Fig-3b]. These vertical incisions were connected by a horizontal incision at the apical end. The papillary unit was displaced from the teeth and the interdental area, so that it can be mobilised freely. A-PRF membrane was prepared and placed on the recipient site and stabilised [Table/Fig-4a]; then papilla was coronally advanced to obliterate the open embrasure completely between 22 and 23. The free end of the flap was sutured with the adjacent gingiva with 4-0 mersilk (Ethiprime) sutures [Table/Fig-4b]. Coe-pak periodontal dressing was placed in the surgical site [Table/Fig-4c]. All patients were prescribed a course of antibiotics (Capsule Amoxicillin 500 mg, thrice a day for 5 days) and analgesic (Tablet Aceclofenac 100 mg+Paracetamol 325 mg, twice a day for 3 days). Post-surgical instructions were given to the patient. Patient was instructed not to brush over the pack and to avoid hot foods during the first 3 hours after surgery to permit the pack to harden. Patient was advised not to smoke.
a) Incision placed by modified Beagles technique; b) Mucoperiosteal Flap elevated.

a) A-PRF membrane stabilised; b) Sutures placed; c) Periodontal dressing placed.

Post-operative Follow-up
The periodontal dressing and the sutures were removed after 2 weeks. Healing was found to be uneventful. There was 100% papillary fill when the patient was reviewed after 2 weeks follow-up and the same was maintained after 3 months [Table/Fig-5a,b]. The patient did not turn up for further follow-up after 3 months. The distance from the contact point to the interproximal osseous crest was 4 mm as compared to the baseline value of 2 mm which was before the surgery. After 3 months follow-up the Papilla Presence Index score had become 1 from 2.
a) 2 weeks postoperative view b) 3 months postoperative view depicting complete papillary fill.
Discussion
The embrasure space in a healthy tooth is usually completely filled by the interdental papilla [5]. The loss of key papilla in an aesthetic zone leads to “black triangle” causing unaesthetic appearance, difficulties in speech and lateral food impaction. The factors that influence the presence or absence of papilla are the presence of underlying osseous support, periodontal biotype, tooth morphology, and contact point between adjacent teeth. The key reason for black triangle formation in the current case was loss of periodontal support. A-PRF which is a third-generation platelet concentrate acts as a scaffold which contains cells like lymphocytes, monocytes, neutrophils, etc., which are responsible for effective healing. Changes in the centrifugation time and speed, leads to a different distribution pattern for neutrophilic granulocytes [6].
The classic study by Tarnow DP et al., concluded that the distance from the base of the contact area to the crest of bone corresponds with the presence or absence of the interproximal papilla. According to the study, if the distance from the contact point to the interproximal osseous crest is 5 mm or less, total fill of the gingival embrasures with an interdental papilla takes place; with every 1 mm increase over 5 mm, the probability of complete fill of papilla decreases by 50% [2]. Similarly, in the present study, the distance from the contact point to the interproximal osseous crest was observed to be 4 mm after 3 months.
In the original Beagle’s technique, a partial thickness incision was made with help of an ophthalmic crescent knife along the line angles of adjacent teeth on the palatal side. In the interdental region, sulcular incisions were given to dislocate the papillary unit. The elongated papilla was folded. There was a risk of damage to the incisive nerves and vessels in order to approximate the connective tissue sides. Involvement of fat beneath the flap jeopardises the vascular supply and hence makes it difficult to obtain a palatal flap of uniform thickness and to retain the periodontal dressing [4].
To overcome the limitations of the original Beagle’s technique, in the present case report, modified Beagle’s technique with A-PRF was used for papilla reconstruction. This technique has the following merits: no second surgical site was needed since mucoperiosteal flap was reflected alone, no injury to palatine nerve and vessels because palatal flap which is used in original Beagle’s technique was not used; enhanced healing due to abundant growth factors present in the A-PRF membrane; reduced post-operative discomfort with good patient compliance due to reduced chair-side timing and minimally invasive surgical technique; prevention of dead space formation which retards the vascularisation and jeopardises the success of the graft by using A-PRF membrane.
Studies have been done for papilla reconstruction using platelet rich fibrin where PRF membrane has both mechanical adhesive properties and biological functions like fibrin glue which maintains the flap in stable position, increases the neo-angiogenesis, decreases the necrosis and shrinkage of the flap [7]. In the present study, we have used A-PRF also known as super PRF which plays a major role in the release of certain cytokines and sustained release of growth factors for tissue regeneration. Growth factor release is a key function of fibrin clots for tissue regeneration. A-PRF shows significantly higher growth factor release as well as gradual release upto a 10-day period. The distribution of neutrophilic granulocytes within the A-PRF clot is important for improved functionality of the transplanted and resident monocytes/macrophages and lymphocytes, they increase tissue regeneration. A-PRF contains more living progenitor cells and platelets, the subsequent significant increase in total protein release is an additional advantage for clinical use [8,9].
The procedure in the current case was atraumatic, (since second surgical site not needed) with primary closure contributing to the overall success. This procedure has an additional advantage of not requiring a second site for graft harvest, thus enhancing the patient compliance and lowering the post-operative morbidity. This case report is first of its kind wherein an A-PRF membrane has been used for papilla reconstruction.
During the course of the study, patient maintained good oral hygiene and elicited better compliance. There were no signs of inflammation in the study period.
Conclusion(s)
Papilla reconstruction techniques are an exciting area of interest in periodontal therapy. This case report with A-PRF could contribute to evidence in the subject of papilla reconstruction in future. Controlled clinical trials in the future could add up to the current evidence.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 26, 2019
Manual Googling: Feb 07, 2020
iThenticate Software: Mar 18, 2020 (14%)
[1]. Jamwal D, Kanade K, Tanwar VS, Waghmare P, Landge N, Treatment of interdental papilla: A review galoreInt J Health Sciences Research 2019 4(2):2456-9321. [Google Scholar]
[2]. Tarnow DP, Magner AW, Fletcher P, The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papillaJ Periodontol 1992 63(12):995-96.10.1902/jop.1992.63.12.9951474471 [Google Scholar] [CrossRef] [PubMed]
[3]. Ghanaati S, Booms P, Orlowska A, Kubesch A, Lorenz J, Rutkowski J, Advanced platelet-rich fibrin: A new concept for cell-based tissue engineering by means of inflammatory cellsJ Oral Implantol 2014 40(6):679-89.10.1563/aaid-joi-D-14-0013824945603 [Google Scholar] [CrossRef] [PubMed]
[4]. Beagle JR, Surgical reconstruction of the interdental papilla: Case reportInt J Periodontics Restorative Dent 1992 12(2):145-51. [Google Scholar]
[5]. Prato GP, Rotundo R, Cortellini P, Tinti C, Azzi R, Interdental papilla management: A review and classification of the therapeutic approachesInt J Periodontics Restorative Dent 2004 24(3):246-55.10.1016/j.prosdent.2004.07.00215227772 [Google Scholar] [CrossRef] [PubMed]
[6]. Kolaczkowska E, Kubes P, Neutrophil recruitment and function in health and inflammationNat Rev Immunol 2013 13(3):159-75.10.1038/nri339923435331 [Google Scholar] [CrossRef] [PubMed]
[7]. Arunachalam LT, Merugu S, Sudhakar U, A novel surgical procedure for papilla reconstruction using platelet rich fibrinContemp Clin Dent 2012 3(4):467-70.10.4103/0976-237X.10744323633811 [Google Scholar] [CrossRef] [PubMed]
[8]. Ley K, Laudanna C, Cybulsky MI, Nourshargh S, Getting to the site of inflammation: The leukocyte adhesion cascade updatedNat Rev Immunol 2007 7(9):678-89.10.1038/nri215617717539 [Google Scholar] [CrossRef] [PubMed]
[9]. Kobayashi E, Flückiger L, Fujioka-Kobayashi M, Sawada K, Sculean A, Schaller B, Comparative release of growth factors from PRP, PRF and advanced-PRFClin Oral Invest 2016 20(9):2353-60.10.1007/s00784-016-1719-126809431 [Google Scholar] [CrossRef] [PubMed]