Ocular Adnexal Lymphoma Misdiagnosed as Myelodysplastic Syndrome
Sonali Vinay Kumar1
1 Classified Specialist, Department of Ophthalmology, Army Hospital R and R, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Sonali Vinay Kumar, AHRR, Delhi Cantt, Delhi, India.
E-mail: sonaliv91775@hotmail.com
Systemic lymphoma can have a varied presentation which can mislead physician resulting in wrong diagnosis. Lymphoma, when involves bone marrow, results in deranged blood picture as production of blood cells is affected. A 55-year-old patient presented with occipital headache since two and a half years and protrusion of both eyes, since two years. Patient was initially diagnosed of Myelodysplastic syndrome as he was found to have deranged blood picture and was advised observation. Ophthalmic consultation was sought and he was subjected to conjunctival incision biopsy. Histopathology showed features suggestive of extranodal marginal zone lymphoma. Tissue biopsy played a crucial role for definitive diagnosis and patient was started on treatment. Patient responded to treatment and has recovered. So, lymphoma should be considered as a differential diagnosis whenever patient presents with altered blood picture associated with a lesion in eye.
Deranged blood picture, Histopathology, Optical headache
Case Report
A 55-year-old male patient reported with complaints of occipital headache since two and a half years and protrusion of both eyes since two years. Occipital headache was intermittent and not associated with ocular complaints. There was no history of fever/weight loss/night sweats.
For this he consulted a physician at the time of presentation and he was evaluated. On evaluation he was found to have bicytopenia (leucopenia and thrombocytopenia) and normocytic anaemia. Bone marrow biopsy showed hypercellular erythroid hyperplasia with no blast cells. Based on peripheral blood smear and bone marrow biopsy report he was diagnosed to have Myelodysplastic syndrome. Since he had no other complaints other than occipital headache and his haemoglobin was 11 gm/dL, patient was advised close observation and monitoring. Meanwhile he developed painless, progressive and outward protrusion of both eyes since two years. He also noticed a mass in both eyes with redness over white part of eye since two years which was gradually increasing in size. There was no history of irritation, discharge, ocular injury or any ocular surgical intervention.
Thus, he presented to have an ocular examination done. It showed distant vision in both eyes 6/6 and near vision in both eyes was N6 with +2.50 sph. On gross examination, a fleshy salmon coloured swelling in superotemporal quadrant extending into inferior forniceal conjunctiva was found in both eyes [Table/Fig-1a]. Lacrimal gland was found enlarged in both eyes and enlarged caruncle in RE [Table/Fig-1b]. Slit lamp examination showed grade 1 nuclear sclerosis in both eyes. Rest of the anterior segment and fundus examination were normal. Systemic examination showed splenomegaly and enlarged bilateral cervical and abdominal lymph nodes. Hertel’s ophthalmometry (base-110 mm) measured 22 mm in RE and 24 mm in LE. CT orbit showed multiple heterogenous lesion in both intra and extraconal compartment of both orbits [Table/Fig-1c], (yellow arrow). Multiple similar lesions were also seen along both optic nerve and lacrimal gland. A few of these deposits were also seen abutting and infiltrating the extraocular muscle predominantly involving superior, inferior and lateral rectus. [Table/Fig-1c], (yellow arrow).
a) Clinical photograph showing pinkish lesion in superotemporal quadrant extending into inferior forniceal conjunctiva with enlarged lacrimal gland (black arrow); b) Clinical photograph showing enlarged caruncle (black arrow); c) CT orbit showing lesion multiple heterogenous lesions in both intra and extraconal compartment of both orbits. Multiple similar lesion were also seen along both optic nerve and lacrimal gland. A few of these deposits were also seen abutting and infiltrating the extraocular muscle predominantly involving superior, inferior and lateral rectus (yellow arrow).

As the diagnosis was not certain, patient was subjected to incision biopsy. A part of mass was removed from inferotemporal quadrant of conjunctiva. Histopathological examination showed whole stroma was infiltrated by sheets of atypical lymphoid cells [Table/Fig-2a], (black arrow). These cells were small to intermediate in size with hyperchromatic, inconscpicous nucleoli and scanty cytoplasm [Table/Fig-2b], (black arrow).
a): Histopathological features of lymphoma showing whole stroma is infiltrated by sheets of atypical lymphoid cells (black arrow) (10x); b): Histopathological features showing small to intermediate in size cells with hyperchromatic, inconscpicous nucleoli and scanty cytoplasm (black arrow) (40x).

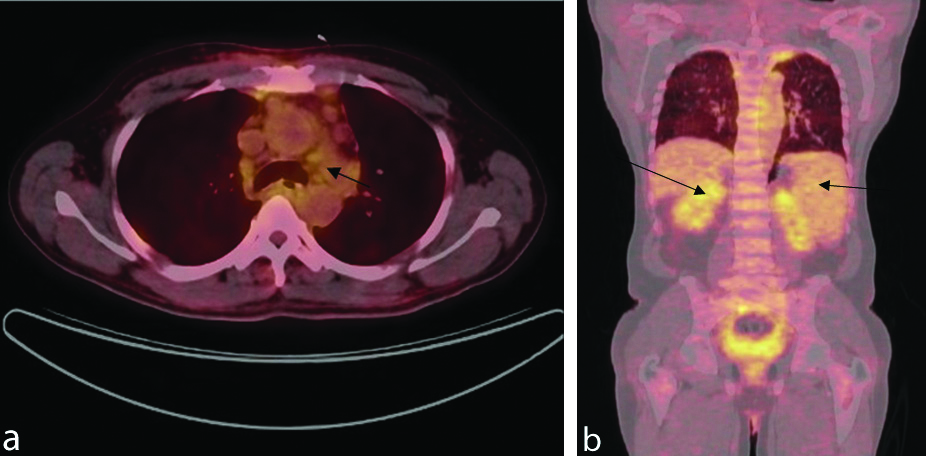
PET CT scan showed multiple enlarged cervical, mediastinal, hilar and abdominal nodes [Table/Fig-3a], (black arrow). It also showed spenomegaly and pleural thickening in apices of both lungs [Table/Fig-3b], (black arrow). So the final diagnosis was systemic and ocular adnexal lymphoma. Oncologist’s opinion was sought and patient was recommended 04 cycles of chemotherapy (Inj Rituximab, Inj Cyclophosphamide, Inj Vincristine, Tab Prednisolone). After 02 cycles of chemotherapy, there was complete disappearance of all lesions and proptosis also reduced [Table/Fig-4]. Patient is still on chemotherapy and doing well.
a) PET CT showing enlarged mediastinal lymph nodes (black arrow); b) PET CT showing spenomegaly and pleural thickening in apices of both lungs (black arrow).
Clinical photograph after one month of treatment showing reduction in proptosis and conjunctival lesion.

Discussion
Ocular Adnexal Lymphoma (OAL) are often misdiagnosed due to low prevalence in population and because of its vague presentation [1,2]. However, the incidence of ocular adnexal lymphoma has risen worldwide over the last few decades because of the growing no older individual, immunosuppression due to AIDS, immunosuppressive drugs or organ transplantation and improvements in diagnostic techniques [3].
Clinical features are also non-specific and depend on the location of lymphoma which makes the diagnosis of lymphoma difficult. Accurate diagnosis of lymphoma and staging is mandatory for appropriate treatment. Tissue biopsy plays a key role for correct diagnosis when there is a diagnostic dilemma [4].
Right diagnosis of a disease is critical to provide proper care but sometimes an error can happen when the disease is rare and symptoms are vague. In this case, patient was initially diagnosed as a case of Myelodysplastic syndrome on the basis of complete blood count report which showed pancytopenia and bone marrow report which showed hypercellular and erythroid hyperplasia. He also sought ophthalmic consultation twice but no intervention was done and he was managed conservatively. He reported to the present institute with same presentation and ocular adnexal lymphoma was provisionally diagnosed based on clinical features. Patient underwent conjunctival biopsy and histopathological examination confirmed the diagnosis of low grade lymphoma.
Diagnosis of ocular lymphoma is challenging because it can affect any part of eye and can mimic other pathologies [5]. Ocular adnexal lymphoma if associated with systemic lymphoma presents with deranged blood picture [6]. So, high index of clinical suspicion of lymphoma is required whenever patient presents with altered blood picture.
Ocular adnexal lymphoma presents as insidious onset, slowly progressive and painless mass involving conjunctival tissue, eyelid, orbital soft tissue, muscle, lacrimal gland and sometimes it involves optic nerve [5]. Eighty percent of ocular adnexal lymphomas are B cell Non Hodgkin lymphomas with extranodal marginal zone lymphoma being the most common histologic subtype followed by follicular lymphoma, diffuse B cell lymphoma and mantle cell lymphoma [7]. All cases of ocular adxexal lymphoma should be thoroughly investigated to rule out systemic lymphoma not only at initial presentation but also during follow-up visit.
Basic investigations include complete blood count, liver function test, ELISA for HIV and bone marrow biopsy. Whole body PET CT scan is better for detecting systemic involvement compared to traditional imaging like chest X-ray and ultrasound abdomen. Imaging like CT and MRI orbit not only helps in identifying the extent and location of the lesion but also to rule out deeper tissue involvement in conjunctival and ocular adnexal lymphoma [8]. Tissue biopsy plays a key role when symptoms may not be readily apparent for definitive diagnosis and in identification of histologic subtype of lymphoma [4].
The treatment of ocular adnexal lymphoma depends upon histologic subtype and presence of systemic involvement. The armamentarium for the treatment of ocular adnexal lymphoma includes radiotherapy and systemic chemotherapy in combination with steroids [9]. Radiotherapy is recommended in patients with low grade and localised lymphoma [10]. Radiotherapy in combination with chemotherapy and steroids is recommended in high grade lymphoma and in patients with systemic spread. Surgical excision is not preferred as it often ends with a relapse of the disease as complete excision is not possible due to location of tumour [9]. In all cases of ocular adnexal lymphoma long term follow-up is required to rule out recurrence.
Conclusion(s)
All patients who presents with deranged blood count should be evaluated for systemic and ocular lymphoma for timely diagnosis. Tissue biopsy plays an important role when diagnosis is not certain. Observation without treatment is not recommended in patients with Ocular Adnexal Lymphoma (OAL) due to high risk of progression.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 11, 2020
Manual Googling: Feb 27, 2020
iThenticate Software: Mar 16, 2020 (11%)
[1]. Dorey S, Clark B, Christopoulus V, Orbital lymphoma misdiagnosed as scleritisOphthalmology 2002 109:2347-50.10.1016/S0161-6420(02)01285-X [Google Scholar] [CrossRef]
[2]. Wolyniak B, Lewczuk A, Obolonczyk L, Majeswska H, Sworczak K, Orbital lymphoma mimicking Graves’s ophthalmopathy: A case reportCent, Eur J Med 2011 6(6):826-29.10.2478/s11536-011-0081-6 [Google Scholar] [CrossRef]
[3]. Moslehi R, Devesa SS, Schairer C, Fraumeni JF, Rapidly increasing incidence of ocular non-Hodgkin lymphomaJ Natl Cancer Inst 2006 98:936-39.10.1093/jnci/djj24816818858 [Google Scholar] [CrossRef] [PubMed]
[4]. Shields JA, Shields CL, Scartozzi R, Survey of 1264 patients with orbital tumours and simulating lesionsOphthalmology 2004 111:997-1008.10.1016/j.ophtha.2003.01.00215121380 [Google Scholar] [CrossRef] [PubMed]
[5]. Mulay K, Honaver S, An update on ocular adnexal lymphomaSeminars in Diagnostic pathology 2016 33:164-72.10.1053/j.semdp.2015.10.00426972223 [Google Scholar] [CrossRef] [PubMed]
[6]. Demirci H, Shield C, Karatza E, Shield J, Orbital lymphoproliferative tumours analysis of clinical features and systemic involvement in 160 casesOphthalmology 2008 115:1626-31.10.1016/j.ophtha.2008.02.00418440641 [Google Scholar] [CrossRef] [PubMed]
[7]. Fung CY, Tarbell NJ, Lucarelli MJ, Goldberg SI, Linggood RM, Harris NL, Ocular adnexal lymphoma: clinical behaviour of distinct World Health Organization classification subtypesInt J Radiat Oncol Biol Phys 2003 57(5):1382-91.10.1016/S0360-3016(03)00767-3 [Google Scholar] [CrossRef]
[8]. Kamal S, Kaliki S, Ocular adnexal lymphoma: clinical presentation, diagnosis, treatment and prognosisJ Mol Biomark Diagn 2017 8:31210.4172/2155-9929.1000312 [Google Scholar] [CrossRef]
[9]. Yen MT, Bilyk JR, Wladis EJ, Bradly EA, Mawn LA, Treatments for ocular adnexal lymphomaOphthalmology 2018 125:127-36.10.1016/j.ophtha.2017.05.03728712656 [Google Scholar] [CrossRef] [PubMed]
[10]. Liao SL, Kao SC, Hou PK, Chen MS, Results of radiotherapy for orbital and adnexal lymphomaOrbit 2002 21:117-23.10.1076/orbi.21.2.117.719212029566 [Google Scholar] [CrossRef] [PubMed]