Co-existence of Pulmonary Tuberculosis and Interstitial Lung Disease in a Patient of Connective Tissue Disorder: A Case Report
Huma Firdaus1, Nafees Ahmad Khan2, Ummul Baneen3, Mohammad Shameem4, Rakesh Bhargava5
1 Senior Resident, Department of TB and Respiratory Diseases, JN Medical College, Aligarh, Uttar Pradesh, India.
2 Assistant Professor, Department of TB and Respiratory Diseases, JN Medical College, Aligarh, Uttar Pradesh, India.
3 Assistant Professor, Department of TB and Respiratory Diseases, JN Medical College, Aligarh, Uttar Pradesh, India.
4 Professor, Department of TB and Respiratory Diseases, JN Medical College, Aligarh, Uttar Pradesh, India.
5 Professor, Department of TB and Respiratory Diseases, JN Medical College, Aligarh, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Nafees Ahmad Khan, Department of TB and Respiratory Diseases, Aligarh Muslim University, Aligarh, Uttar Pradesh, India.
E-mail: NAFEES.DOC@GMAIL.COM
Pulmonary involvement is common in patients with systemic sclerosis. The most common underlying histology is Non Specific Interstitial Pneumonia (NSIP). Disrupted immunity from the disease or associated medication may render such patients prone to develop tuberculosis infection. A 55-year-old female patient presented with chief complaints of shortness of breath from past five years which was gradually progressive, cough initially dry later with minimal expectoration, low grade fever from past two months. She also gave history of bluish discolouration of fingers tips on exposure to cold water. On examination there was restrictive mouth opening, thickened skin over hands, forearm, face, neck and trunk on pinching. Sclerodactyly was present with clubbing grade 2. On auscultation bilateral fine crepts were present. Serum ANA was highly raised and Scl 70 was positive. PFT was suggestive of restrictive ventilatory abnormality. Sputum smear for AFB was found to be positive. HRCT thorax was suggestive of NSIP. Patient was put on antituberculer treatment under DOTS category 1; nifedipine, pentoxyphylline and nitroglycerine gel was started for raynauds phenomenon. Chemotherapy for systemic sclerosis was given with cyclophosphamide infusion in six cycles every four weeks.
Raynaud’s pheomenon, Sputum positive pulmonary tuberculosis, Systemic sclerosis
Case Report
A 55-year-old female patient presented to Outpatient Department (OPD) for Tuberculosis (TB) and Respiratory diseases, with chief complaints of shortness of breath from last five years which was gradual in onset and progressive in nature. Initially, patient was dyspneic only on doing strenuous activity but with progression of dyspnea patient was now breathless even at rest, cough for last six months which was initially dry but later with minimal expectoration for last two months and low grade fever for last two months. She consulted some local practitioners but there was no satisfactory response.
She also complained of tightening of the skin over her hands, forearm, face, neck and trunk for the last six months and bluish discolouration of fingers tips on exposure to cold water. There was no history of chest pain, and haemoptysis. No history of diabetes mellitus, hypertension or any other chronic illness or previous hospitalisation. There was no significant family history nor any other family member had similar complaints.
On examination, her general condition was fair and patient was of average built. There was restrictive mouth opening, thickened skin over hands, forearm, face, neck and trunk. Sclerodactyly was present with clubbing grade 2 [Table/Fig-1]. On auscultation bilateral fine crepts were present. There was no pallor, cyanosis, lymphadenopathy or pedal oedema. PR was 94/min, BP: 118/74 mmHg, RR 14/min at the time of examination. Other systems were normal.

Haematological investigations showed total leucocytes were 13.3×103/microL (N-66%, L-31%, M-3%, E-0, B-0), Hb 13 g/dL, Random blood sugar 96 mg/dL, blood urea 32 mg/dL, serum creatinine 0.8 mg/dL. Liver function test was normal. Serum Antinuclear Antibody (ANA) was significantly raised (lab value-132) and Scl 70 was positive (lab value-56). Lung function tests (spirometry) were suggestive of restrictive ventilatory abnormality.
Sputum smear for acid fast bacilli was found to be positive (2+)(6-10 bacilli seen per high power field with fluorescent staining). Sputum LPA showed isoniazid and rifampicin sensitive.
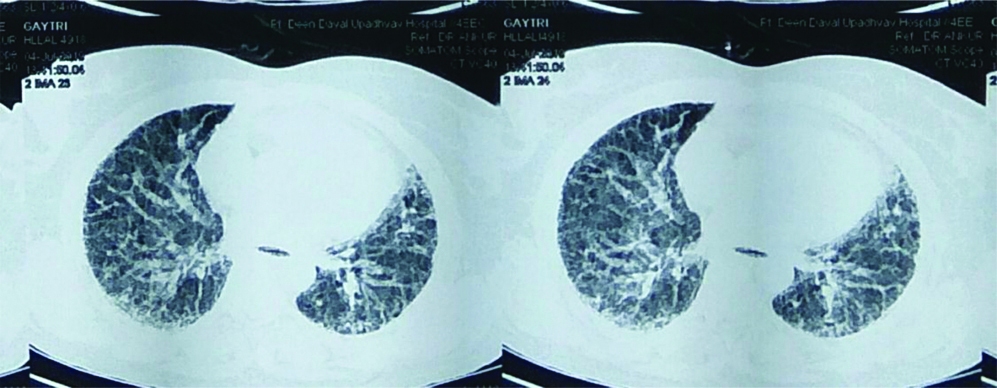
A 2D Echo, USG abdomen, Troponin I and Brain Natriuretic Peptide (BNP) were normal. Chest radiograph was done and showed reticulonodular opacities in mid and lower zones of both lungs with small cavities in right middle zone. [Table/Fig-2]. High Resolation Computed Tomography (HRCT) thorax was done and finding was suggestive of Non Specific Interstitial Pneumonia (NSIP) with diffuse ground glass opacities and inter and intralobular septal thickening with minimal honeycombing, Computed Tomography (CT) scan showed no specific features suggestive of tuberculosis [Table/Fig-3].
Chest radiograph at the starting of treatment.

HRCT thorax showing diffuse ground glass opacities and inter and intralobular septal thickening.
A dignoasis of pulmonary tuberculosis was confirmed microbiologically with interstitial lung disease, Raynaud’s phenomenon and systemic sclerosis. Patient was put on Antitubercular (ATT) drugs under Revised National Tuberculosis Control Program- Directly Observed Treatment Short Course (RNTCP DOTS) category I (isoniazid, rifampicin, pyrazinamide and ethambutol) for a period of 6 months, Nifedipine 5 mg OD; Pentoxyphylline 400 mg BD and Nitroglycerine gel was started after dermatology consultation for Raynaud’s phenomenon. Chemotherapy for systemic sclerosis was started with injectable cyclophosphamide 500 mg given as infusion.
Patient was discharged on ATT, oral low dose steroid (16 mg) on alternate day, Nifedipine 5 mg OD, Pentoxyphylline 400 mg BD, Nitroglycerine gel for local application for vasodilation. She was followed-up in OPD and total of 6 cycles of injectable cyclophosphamide were given every six weeks.
ATT was stopped after a six months course and patient became sputum negative and chest radiograph showed improvement [Table/Fig-4]. There was improvement in dyspnea and the patient was able to perform her daily activities. Skin tightness also improved, she could make a fist now, mouth opening improved (as told by the patient) and skin became loose over forearms, face, neck and trunk. No major side effect was reported during treatment. Few episodes of vomiting was complained by the patient after cyclophosphamide infusion which used to improve on antiemetics.
Chest radiograph after 6 months of ATT and 6 cycles of chemotherapy.

Discussion
Scleroderma or systemic sclerosis is an inflammatory fibrotic disease that results in deposition of excessive extracellular matrix in skin and several visceral organs involving the lungs, heart, kidneys, and Gastro Intestinal Tract (GIT). Incidence is three times more in women than in men with the peak incidence between ages 20-60 [1]. Two subtypes of systemic sclerosis exist: diffuse and limited. The diffuse variant causes extensive skin involvement of the extremities, face and torso and accompanying visceral involvement which is progressive in nature. The limited form or CREST variant (calcinosis, Raynaud’s phenomenon, oeosohageal dysmotility, sclerodactyly and telengiectasia) has a more protracted course in most patients and usually affects older patients. Lung are involved in 30% to 100% of cases. The most common underlying histology in systemic sclerosis is NSIP with honeycomb lung.
Patients with autoimmune diseases are known to develop infections like tuberculosis. There can be two possible mechanisms of which one could be possible immune dysfunction which predisposes to both immune-mediated disease and tuberculosis, however this requires further research. Another possible mechanism is immunosupprresion due to treatment with immunosuppressive drugs in patients of immune mediated disorders like long term corticosteroids and more recently TNF inhibitors have been shown to increase the risk of TB [2]. Tuberculosis itself can induce the development of autoantibodies leading to autoimmune diseases [3]. This was a case where patient was found to be sputum positive pulmonary tuberculosis prior to the initiation of chemotherapy for systemic sclerosis showing co-existence of both pulmonary tuberculosis and interstitial lung disease in systemic sclerosis.
A significant association of tuberculosis and autoimmune diseases like Addison’s disease, SLE, polymyositis and patients with scleroderma was found by Ramagopalan SV, et al., [4].
Study by Shachor Y et al., suggested that there is increased susceptibility of developing tuberculosis or reactivation of dormant tuberculosis in patients with damaged lungs [5]. Another study done by Subramanian S et al., highlights the association of tuberculosis and autoimmune diseases [6]. In a study done in Taiwan, in 838 patients with systemic sclerosis they found that the incidence of tuberculosis infection was 4.5 times higher than the controls [7].
Conclusion(s)
The present case is aimed to highlight the association between tuberculosis and other connective tissue related diseases. Physicians should be aware of such conditions to facilitate early diagnosis and treatment. However, further research is required to understand the mechanism behind association of increased risk of TB in patients of immune mediated disorders and vice versa.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 03, 2020
Manual Googling: Feb 08, 2020
iThenticate Software: Mar 16, 2020 (13%)
[1]. Steen VD, Oddis CV, Conte CG, Janoski J, Casterline GZ, Medsger TA Jr, Incidence of systemic sclerosis in allegheny county, Pennsylvania. A twenty-year study of hospital-diagnosed cases, 1963-1982Arthritis Rheum 1997 40(3):441-45.10.1002/art.17804003099082931 [Google Scholar] [CrossRef] [PubMed]
[2]. Lawn SD, Zumla AI, TuberculosisLancet 2011 378:57-72.10.1016/S0140-6736(10)62173-3 [Google Scholar] [CrossRef]
[3]. Pradhan V, Patwardhan M, Athavale A, Taushid S, Ghosh K, Mycobacterium tuberculosis triggers autoimmunityIndian J Tuberc 2012 59(1):49-51. [Google Scholar]
[4]. Ramagopalan SV, Goldacre R, Skingsley A, Conlon C, Goldacre MJ, Associations between selected immune mediated diseases and tuberculosis: Record linkage studiesBMC Medicine 2013 97(11):1741-7015.10.1186/1741-7015-11-9723557090 [Google Scholar] [CrossRef] [PubMed]
[5]. Shachor Y, Schindler D, Siegal A, Lieberman D, Mikulski Y, Bruderman I, Increased incidence of pulmonary tuberculosis in Chronic interstitial lung diseaseThorax 1989 44:151-53.10.1136/thx.44.2.1512929001 [Google Scholar] [CrossRef] [PubMed]
[6]. Subramanian S, Ragulan R, Natraj M, Meenakshi N, Viswambhar V, Co-existence of scleroderma and TuberculosisSch J Med Case Rep 2015 3(1):22-24. [Google Scholar]
[7]. Ou SM, Fan WC, Cho KT, Yeh CM, Su VYF, Hung MH, Systemic sclerosis & the risk of tuberculosisJ Rheumatol 2014 41(8):1662-69.10.3899/jrheum.13112525028380 [Google Scholar] [CrossRef] [PubMed]