Cylindromas are adnexal tumours of either eccrine or apocrine origin. Two common variants- Solitary and Multiple are seen, of which the malignant transformation of a solitary lesion is rare. Solitary tumours occur sporadically in the head and neck and are without a familial history whereas the multiple tumours are inherited in an autosomal dominant pattern occurring in scalp and rarely on trunk. Malignant transformation is observed commonly in multiple tumours, although transformation of solitary lesions has also been reported. We report a rare case of malignant transformation of a solitary cylindroma involving the fronto-nasal region in a 72-year-old diabetic and hypertensive male reported to the Department of Oral and Maxillofacial Surgery, with a chief complaint of rapidly growing, painful growth over fronto-nasal region for 3-years and difficulty in breathing since 3-months. on examination; a single, large, well circumscribed, tender, firm and fixed multinodular growth with focal areas of ulcerations and reddish brown crustations of approx. 9.0×3.5 cm measuring in its greatest dimension was seen in naso-frontal region. A CECT Head showed a well defined, heterogeneously enhancing lobulated soft tissue mass, occupying the left nasal cavity, ethmoid sinus and extending into medial extraconal space of left orbit. The incisional biopsy report suggested low grade skin adnexal tumor of malignant cylindroma. Based on the finding in the biopsy, the CECT surgical excision of the lesion was planned. The patient was kept on follow-up of 3 years and no local recurrence or distant metastases was noted.
Adnexal tumours, Canaliculi, Malignant cylindroma, Microcyst, Multinodular
Case Report
A 72-year-old diabetic and hypertensive male reported to the Department of Oral and Maxillofacial Surgery, with a chief complaint of rapidly growing, painful growth over fronto-nasal region for 3-years and difficulty in breathing since 3-months. He gave a history of noticing a small nodular growth which gradually increased to present size. There was history of difficulty in breathing and on examination; a single, large, well circumscribed, tender, firm and fixed multinodular growth with focal areas of ulcerations and reddish brown crustations of approx. 9.0×3.5 cm measuring in its greatest dimension was seen in naso-frontal region crossing the midline [Table/Fig-1]. Excision of a similar mass five years back was also reported. A differential diagnosis of Basal cell carcinoma, trichilemmoma, trichoepithelioma, basaloid follicular hamartoma, spiradenoma, cylindroma and neurofibromatosis was formulated and a biopsy for the lesion was planned following CECT Head.
Preoperative frontal view, showing soft tissue mass.

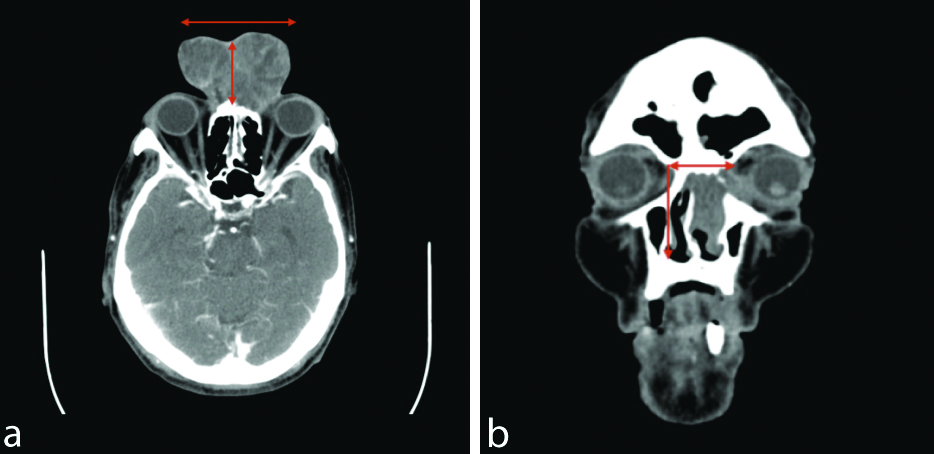
A CECT Head was done, which showed a well defined, heterogeneously enhancing lobulated soft tissue mass, occupying the left nasal cavity, ethmoid sinus and extending into medial extraconal space of left orbit. The lesion had caused destruction of adjacent nasal bone, medial wall of left orbit and was abutting the medial rectus muscle of the left orbit. The brain parenchyma appeared normal [Table/Fig-2a,b].
a) CECT head- axial view- showing the extension of the lesion; b) CECT head- sagittal view- destruction of the underlying bone.
The incisional biopsy showed myxoid flakes and spindle nuclear cells in small fragments, entrapped within these flakes were basaloid, polygonal epithelial cells which showed hyperchromasia, mild pleomorphism and granular chromatin. At places the hyaline myxoid nature appeared in small cylindrical group surrounded by epithelial cells. The report suggested of low-grade skin adenexal tumour of malignant cylindorma” [Table/Fig-3a].
a) Pictomicrograph (H&E, 10X) view showing myxoid flakes and spindle nuclear cells in small fragments, entrapped within these flakes were basaloid, polygonal epithelial cells which showed hyperchromasia, mild pleomorphism and granular chromatin; b) Pictomicrograph (H&E, 40X) view showing irregular dermal cords and nests of highly atypical and pleomorphic cells, which sometimes show ductal differentiation and cyst formation, pleomorphic nuclei, increased abnormal mitoses, loss of hyaline sheaths and loss of peripheral palisading at the tumour island periphery.

Based on the finding in the biopsy and the CECT surgical excision of the lesion was planned. Under general anaesthesia, wide local excision of lesion with a safety margin of 2cm was carried out and the defect was reconstructed using a scalp rotational flap based on the superficial temporal artery. The defect over the scalp was covered with split thickness skin graft. The excised specimen was submitted for histopathological examination.
The histological sections showed various sized cylindroid groups abutting each other made of small to intermediate size cells; Basaloid, cuboidal to polygonal in shape, attempting to form glands, canaliculi and microcyst. Nuclei of the cells were aggressive in appearance. The tumour mass in all sections was in close proximation to the dermis of the skin [Table/Fig-3b].
The patient was kept on follow-up of 3 years and no local recurrence or distant metastases was noted [Table/Fig-4].
Post-operative 3-year follow-up of patient.

Discussion
Cylindroma was first described by Ancell H in 1842 and its malignant nature was described by Weidman in 1929 [1-3]. Cutaneous cylindromas are rare adnexal skin tumours of the head and neck originating from the eccrine or apocrine glands of the skin appendages [2,4]. Two clinical variants are commonly encountered: 1) Solitary lesion without a familial history; and 2) Multiple cutaneous lesions, which is inherited in an autosomal dominant pattern [4]. Multiple cylindroma along with trichoepitheliomas are pathognomic features of Brook speigler syndrome. Solitary tumours occur sporadically in the head and neck and are without a familial history whereas the multiple tumours are inherited in an autosomal dominant pattern occurring in scalp and rarely on trunk. Malignant transformation is observed commonly in multiple tumours, although transformation of solitary lesions has also been reported. Malignant Cylindromas (MC) are locally aggressive, infiltrative, have a tendency for recurrence and exhibits potential for metastasis and therefore demands long term follow-up [3]. Diagnosis can be difficult due to its rarity and varied differential diagnosis such as Basal cell carcinoma, trichilemmoma, trichoepithelioma, basaloid follicular hamartoma, spiradenoma and neurofibromatosis. These can be ruled out by the histopathological examination of the resected specimens.
Cylindromas present as pink to purple-blue nodular lesions of varying sizes commonly present on the forehead and scalp and less frequently on the head and face regions and extremities [2,5]. The lesions are frequently presented in the 5-7th decade of life and have a higher female predilection (F:M::2:1). When the lesions occur over vital anatomic structures like the eye or the nose, the function may be compromised. Histopathologically, the tumour exhibits irregular dermal cords and nests of highly atypical and pleomorphic cells, which sometimes show ductal differentiation and cyst formation, pleomorphic nuclei, increased abnormal mitoses, loss of hyaline sheaths and loss of peripheral palisading at the tumour island periphery. These are characterised by an infiltrative growth pattern, without connection to the epidermis. Residual benign cylindromatous foci, characterised by a dual cell population, organised in to basaloid islands, surrounded by a thick, hyaline basal membrane with a typical ‘jigsaw’ pattern are scattered though the tumour [6,7]. Immunohistochemically, Malignant cylindromas express markers indicating their dual origins from eccrine and apocrine glands. CMA 5.2, EMA and CEA are expressed in tubular structures, while positivity to S100 and GCDFP-15 is variable [6,8]. performed Immunohistochemistry in the present case, Vimentin and S-100 protein was found to be positive in proliferating cell component of the tumour and EMA was negative except in some areas of skin epidermis. The solitary variant occurs more frequently than the multiple variant and has a lower malignant transformation potential. Malignant transformation is characterised by presence of ulceration, the potential for rapid growth, colour change, presence of pain and fixation of the lesion. However, once the transformation has taken place, the tumour in its aggressive forms, invades the underlying tissues, causing local destruction and potentiates distant metastases. Local, infiltrative growth shows distant metastases with a rate of approximately 67% compared to smaller lesions [9,10]. Metastases is most commonly found in cervical lymph nodes, liver and spine, however lung, rib, stomach and thyroid may also be affected. The prevalence of malignant cylindroma is not well documented as only a few are reported in the literature. Malignant transformation is usually seen in multiple cylindromas but may rarely be seen in solitary form [11]. Among 36 cases described in the literature only 9 solitary lesions transforming to the malignant variant were reported [2]. The present case demonstrated the transformation of a solitary lesion into a malignant variant.
Treatment for solitary lesions entails the surgical excision with wide safety margins of 2 cm laterally and 1 cm basal margin keeping in account for the recurrence and malignant transformation. Other reported treatment modalities are simple excision, scalping, Mohs’ microscopic surgery and laser ablation [2,5,12]. The defect can be reconstructed by local flaps or free grafts. Multiple lesions require a carefully planned, multi-step surgical approach. In the present case/patient case, we performed a wide local excision of the tumour with 2 cm safe margins and reconstruction by scalp rotational flaps. Recurrence following surgical excision is about 42% [4,11].
An electronic literature review was conducted on PubMed to identify case reports describing cylindroma using the search terms such as “malignant cylindroma,” “cylindrocarcinoma”, “head and neck cylindroma” and “transformation cylindroma”. A summary of these cases is shown in [Table/Fig-5] [3,9,11,13-28].
Previously published cases of cylindroma in literature [3,9,11,13-28].
| Author | Age/Sex | Size (cm) | Lesion characteristics | Treatment | Follow-up period (Months) |
|---|
| Lyon JB and Rouillard LM (1961) [13] | 59/M | 10×8 | Left posterior scalp:Reddish, penetrating the dura mater. Necrotic and hemorrhagic. | Excision+Adjuvant RTx | 12 |
| Urbanski SJ et al., (1985) [14] | - | 6.5 | Scalp:initial lesion invaded to calvaria | Excision | 30 |
| Galadari E et al., (1987) [15] | 66/M | 2.5×2.5 | Scalp:Nodular lesion with hemorrhagic crust growing over 6 yrs | | |
| Lin PY et al., (1987) [16] | | 3 | Scalp | | 24 |
| Iyer PV and Leong AS (1989) [17] | 60/M | a) 5×3×3b) 3×3×3 | Left side of the scalp:Fleshy and pedunculated | Excision and RND | |
| Hammond DC et al., (1990) [18] | 69/F | 3 | Right post-auricular:Ulcerating, bulbous, firm. | Excision and RND | 36 |
| Lo JS et al., (1991) [19] | 71/F | 8.8×7×4 | Left parieto-occipital scalp:Rapidly enlarging plaque on scalp, first noticed 5y ago | Mohs Surgery | 84 |
| Lotem M et al., (1992) [20] | 81/F | 1-1.5 | Scalp:Multiple nodules, that were ulcerated, hemorrhagic, necrotic | Excision + grafting | 12 |
| Donner LR et al., (1995) [21] | 81/F | 3×1.2×1.1 | Right mastoid:Growing over 2 yrs,increasingly painful; hard thickening of right mastoid skin | Excision, including mastoid and incus and stapes; neck dissection | 36 |
| Pizinger K and Michal M (2000) [22] | 68/F | 10 | Neck:Red, firm, tender, poorly circumscribed.CT scan revealed other tumours in spinal column, kidney | No intervention | 6 |
| Mashkevich G et al., (2006) [23] | 58/F | 13×9 | Left external auditory canal:Patient presented with aural fullness, otalgia, tinnitus | Excision with SSG | 24 |
| Akgul GG et al., (2013) [24] | 52/M | 20×10 | Scalp:Hyperemic, firm. Needle aspiration of submandibular LN revealed metastasis | Excision of entire scalp, bilateral modified radical neck dissection. Adjuvant CTx and RTx | 60 |
| Abedi SM et al., (2014) [25] | 63/M | 1.8 | Right neck:Painless nodule that increased in size over weeks.No ulceration, no necrosis, no hemorrhage | Excision | |
| Borik L et al., (2015) [3] | 83 | | Scalp:Rapidly growing;poorly circumscribed, with infiltrative growth pattern at the base | Excision | 12 |
| Tripathy SM et al., (2015) [9] | 60/F | 4.2×3.6 | Left post-aural:Painful, insidious onset and progressive over 3 m | Excision | |
| Pal S et al., (2016) [26] | 52/F | 3.5×3 | Left parietal region | Excision | 12 |
| Roncevic R and Roncevic D (2016) [27] | 65/M | 0.5-6 | Multiple over scalp | Excision | 108 |
| Portincasa A et al., (2018) [28] | 18/F | 8×5-20×10 | Multiple over scalp, Frontal area, occipito-temporal and retro-auricular | Excision | 72 |
| Kim SM et al., (2019) [11] | 60/M | | Right parietal region | Excision and Primary closure | 6 |
RTx: Radiotherapy; CTx: Chemotherapy; RND: Radical Neck Dissection; SSG: Split thickness skin graft
The reported case is on follow-up for 3-years and no recurrence or metastasis was recorded.
Conclusion(s)
Malignant cylindromas are rare tumours seen in head and neck region. They are locally invasive and may show distant metastasis. Early diagnosis and treatment gives best results. Regular follow-up to monitor recurrence and distant metastasis is required.
RTx: Radiotherapy; CTx: Chemotherapy; RND: Radical Neck Dissection; SSG: Split thickness skin graft
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 11, 2019
Manual Googling: Feb 19, 2020
iThenticate Software: Mar 16, 2020 (11%)
[1]. Ancell H, History of a remarkable case of tumours developed on the head and face; accompanied with a similar disease in the abdomenMedico-Chir Trans 1842 25:227-306.10.1177/09595287420250011620895749 [Google Scholar] [CrossRef] [PubMed]
[2]. Bansal C, Batra M, Lal N, Srivastava AN, Solitary cylindroma with malignant transformationIndian J Dermatol 2012 57(2):141-43.10.4103/0019-5154.9428922615516 [Google Scholar] [CrossRef] [PubMed]
[3]. Borik L, Heller P, Shrivastava M, Kazlouskaya V, Malignant cylindroma in a patient with Brooke-Spiegler syndromeDermatol Pract Concept 2015 5(2):61-65. [Google Scholar]
[4]. Gerretsen AL, van der Putte SC, Deenstra W, van Vloten WA, Cutaneous cylindroma with malignant transformationCancer 1993 72:1618-23.10.1002/1097-0142(19930901)72:5<1618::AID-CNCR2820720521>3.0.CO;2-5 [Google Scholar] [CrossRef]
[5]. Bernárdez C, Requena L, Treatment of malignant cutaneous adnexal neoplasmsActas Dermo-Sifiliográficas Engl Ed 2018 109(1):06-23.10.1016/j.adengl.2017.11.003 [Google Scholar] [CrossRef]
[6]. Caputo V, Rongioletti F, Malignant cylindromaIn: Rare Malignant Skin TumoursNew York, NYSpringer New York:85-87.10.1007/978-1-4939-2023-5_20 [Google Scholar] [CrossRef]
[7]. Deshpande P, Gupta V, Bhake A, Methylation pattern of retrotransposons: Biomarker for human cancerJ Datta Meghe Inst Med Sci Univ 2018 13(1):66-70.10.4103/jdmimsu.jdmimsu_3_18 [Google Scholar] [CrossRef]
[8]. Birare SD, Dantkale SS, Chavhan SV, Chandekar SD, Narkhede RR, Malignant change in a solitary cylindroma: A rare case reportJ Evol Med Dent Sci 2014 3(25):6909-12.10.14260/jemds/2014/2837 [Google Scholar] [CrossRef]
[9]. Tripathy SM, Somu TN, Sundaram M, Sadhiya S, Malignant cylindroma of post aural region involving the temporal boneJ Clin Diagn Res JCDR 2015 9(7):MD01-02.10.7860/JCDR/2015/13682.623226393151 [Google Scholar] [CrossRef] [PubMed]
[10]. Singh P, Bajaj JK, Gogia AR, Comparison of ropivacaine and lignocaine intravenous regional anaesthesia in upper limb surgeriesAstrocyte 2015 2(1):16-20.10.4103/2349-0977.168252 [Google Scholar] [CrossRef]
[11]. Kim SM, Truong JL, Wu K, Gabril MY, Grant A, Malignant cylindroma of the scalp treated with staged perimeter excision: A case report and literature reviewJPRAS Open 2019 21:01-05.10.1016/j.jpra.2019.04.00332158878 [Google Scholar] [CrossRef] [PubMed]
[12]. Antonescu CR, Terzakis JA, Multiple malignant cylindromas of skin in association with basel cell adenocarcinoma with adenoid cystic features of minor salivary glandJ Cutan Pathol 1997 24:449-53.10.1111/j.1600-0560.1997.tb00822.x9274965 [Google Scholar] [CrossRef] [PubMed]
[13]. Lyon JB, Rouillard LM, Malignant degeneration of turban tumour of scalpTrans St Johns Hosp Dermatol Soc 1961 46(7):74-77. [Google Scholar]
[14]. Urbanski SJ, From L, Abramowicz A, Joaquin A, Luk SC, Metamorphosis of dermal cylindroma: possible relation to malignant transformation. Case report of cutaneous cylindroma with direct intracranial invasionJ Am Acad Dermatol 1985 12:188-95.10.1016/S0190-9622(85)80015-3 [Google Scholar] [CrossRef]
[15]. Galadari E, Mehregan AH, Lee KC, Malignant transformation of eccrine tumoursJ Cutan Pathol 1987 14(1):15-22.10.1111/j.1600-0560.1987.tb00122.x3031140 [Google Scholar] [CrossRef] [PubMed]
[16]. Lin PY, Fatteh SM, Lloyd KM, Malignant transformation in a solitary dermal cylindromaArch Pathol Lab Med 1987 111(1):765-67. [Google Scholar]
[17]. Iyer PV, Leong AS, Malignant dermal cylindromas. Do they exist? A morphological and immunohistochemical study and review of the literaturePathology (Phila) 1989 21(8):269-74.10.3109/003130289090610722483749 [Google Scholar] [CrossRef] [PubMed]
[18]. Hammond DC, Grant KF, Simpson WD, Malignant degeneration of dermal cylindromaAnn Plast Surg 1990 24(2):176-78.10.1097/00000637-199002000-000132156478 [Google Scholar] [CrossRef] [PubMed]
[19]. Lo JS, Peschen M, Snow SN, Oriba HA, Mohs FE, Malignant cylindroma of the scalpJ Dermatol Surg Oncol 1991 17:897-901.10.1111/j.1524-4725.1991.tb03281.x1661755 [Google Scholar] [CrossRef] [PubMed]
[20]. Lotem M, Trattner A, Kahanovich S, Rotem A, Sandbank M, Multiple dermal cylindroma undergoing a malignant transformationInt J Dermatol 1992 31(9):642-44.10.1111/j.1365-4362.1992.tb03985.x1334057 [Google Scholar] [CrossRef] [PubMed]
[21]. Donner LR, Ruff T, Diaz JA, Well-differentiated malignant cylindroma with partially preserved hyaline sheaths a locally invasive neoplasm?Am J Dermatopathol 1995 17(2):169-73.10.1097/00000372-199504000-000098600783 [Google Scholar] [CrossRef] [PubMed]
[22]. Pizinger K, Michal M, Malignant cylindroma in Brooke-Spiegler syndromeDermatol Basel Switz 2000 201:255-57.10.1159/00001849911096200 [Google Scholar] [CrossRef] [PubMed]
[23]. Mashkevich G, Undavia S, Iacob C, Arigo J, Linstrom C, Malignant cylindroma of the external auditory canalOtol Neurotol Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol 2006 27:97-101.10.1097/01.mao.0000188352.97795.8c16371854 [Google Scholar] [CrossRef] [PubMed]
[24]. Akgul GG, Yenidogan E, Dinc S, Pak I, Colakoglu MK, Gulcelik MA, Malign cylindroma of the scalp with multiple cervical lymph node metastasis-A case reportInt J Surg Case Rep 2013 4(7):589-92.10.1016/j.ijscr.2013.02.02723702364 [Google Scholar] [CrossRef] [PubMed]
[25]. Abedi SM, El-Shinnawy I, Alowami S, Malignant cylindroma arising as a solitary neck lesionEur J Dermatol EJD 2014 24(3):403-05.10.1684/ejd.2014.234224751615 [Google Scholar] [CrossRef] [PubMed]
[26]. Pal S, Bose K, Sikder M, Chowdhury M, Fine needle aspiration cytology of cylindroma of scalp: A case reportDiagn Cytopathol 2016 44(12):1082-84.10.1002/dc.2354627456213 [Google Scholar] [CrossRef] [PubMed]
[27]. Roncevic R, Roncevic D, Treatment of multiple scalp cylindromaJ Surg Dermat 2016 1(2):100-02.10.18282/jsd.v1.i2.33 [Google Scholar] [CrossRef]
[28]. Portincasa A, Cecchino L, Trecca EMC, Lembo F, Annacontini L, Ciancio F, A rare case of Brooke-Spiegler syndrome: integrated surgical treatment of multiple giant eccrine spiradenomas of the head and neck in a young girlInt J Surg Case Rep 2018 51:277-81.10.1016/j.ijscr.2018.08.02130241087 [Google Scholar] [CrossRef] [PubMed]