Disturbances in skin health are serious and preventable problems in children’s care settings [1]. Diaper dermatitis as nappy rash and diaper rash, is a type of dermatitis that is present in the diaper area [2-5]. Diaper dermatitis is one of the most common skin problems that is prevalent in newborn infants [6,7]. Diaper dermatitis in infants can cause many complications such as pain and discomfort, irritability, restlessness, and an increased risk of infections especially infections caused by opportunistic germs and fungi [5,6]. This problem can also have negative consequences for the parents of infants. Parents of these infants often experience significant stress, anxiety and discomfort [8, 9].
Due to the complications of diaper dermatitis, researchers have conducted studies on the topic [10-12]. However, no Iranian study evaluated the prevalence and risk factors of diaper dermatitis in children admitted to hospitals and during their hospital stay. On the other hand, samples in a previous study [10-12] were healthy infants and children and less attention was paid to the prevalence of this disorder in ill children during hospital stay. So the aim of this study was to investigate the incidence of diaper dermatitis in Iranian hospitalised children.
Materials and Methods
Design: This descriptive epidemiologic study was conducted in Qazvin City from May 2018 to September 2018. Samples were newborns and infants admitted to the Qods Hospital aged 0-24 months. The study was conducted in paediatric wards 1 and 2, surgery ward, Neonatal Intensive Care Unit (NICU), Pediatric Intensive Care Unit (PICU) and neonatal ward.
Inclusion and exclusion criteria: Newborn to 24 months of age, weight over 2500 g, being admitted in the hospital for at least 72 hours based on researchers experiences, use of diaper. Exclusion criteria were severe skin diseases.
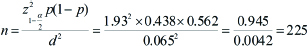
Sample size: According to the results of the study by Li CH et al., the prevalence of dermatitis in 1-24 months old children was reported as 43.8% [11]. Given α=0.05, p=0.438 and d=0.15×p, the sample size was to be 225, however, 228 were included to the study.
Data collection: Skin examination was performed by two researchers, once at the hospital admission and then every 48 hours. The examinations did not disturb the child’s therapeutic process or the care process. To collect data, a researcher-made checklist was designed based on the previous studies and researchers’ experiences [10-12]. It contained 18 items including demographic characteristics of the mother, child and possible risk factors for diaper dermatitis in the hospitalisation time. It included the history and frequency of previous symptoms and the severity of diaper dermatitis in the past 6 weeks, the type of nutrition, fecal consistency, manner of washing the genital area, changing diaper and the frequency of bathing the child before and after admission, type of diaper, use of protective creams etc. The checklist was provided to 10 faculty members and was approved for face and content validity.
The second tool measured the severity of diaper dermatitis. It was designed by Buckley BS et al., and included four domains of erythema and inflammation of the skin at the diaper area, extent of the affected area, presence of papules and pustules and damage to the skin. The scoring of this scale was from 0-6, and the higher score meant a greater severity of dermatitis [13].
The researchers examined the child diaper area in the ward every 48 hours using the scale. The correlation coefficient between the groups in the assessors groups was 0.949, p≤0.001, and the test-retest reliability within a two week interval was reported as r=0.603 and p≤0.001. The Cronbach’s alpha coefficient for the internal reliability was also reported as 0.702 [13]. This questionnaire was also used in other studies of Iran [14].
Ethical Considerations
This study was approved by Qazvin University of Medical Sciences, Iran (decree code: IR.QUMS.REC.1396.314). Before the study, explanations regarding the study type and related objectives were provided to parents of the children. They were asked to announce their consent to participate in this study. Data was kept confidential and used only for purposes specified in the study. For preserving anonymity, codes were assigned to the samples at all stages of the study.
Statistical Analysis
Data was analysed using the SPSS v.23 software. After collecting data, descriptive statistics (frequency and mean) and inferential statistics were used. The Chi-square test was used to examine the frequency distribution of dermatitis. A single-variable logistic regression model was used to determine the predictive variables of dermatitis. Statistically significant variables were entered into the logistic regression multiple regression model and the significance level was set as p<0.05.
Results
A total of 228 children aged between 0-24 months, admitted to Qazvin, were included in this study. The mean age of the children was 6.43 months with a standard deviation of 6.36 months and range of one month to 24 months. 127 (55.7%) babies were males out of total 228 participants. About 53% of participants were hospitalised at the infection, internal and paediatric surgery wards. Others were in neonatal or NICU. The mean age of mother was 28.88 years with a standard deviation of 5.9 years.
Total 116 (50.9%) had diaper dermatitis out of 228 subjects during the hospitalisation period. The severity of diaper dermatitis was reported as 58.6% with severity 1, 19.8% with severity 2, 15.5% with severity 3, and 6% with severity 4.
The incidence of diaper dermatitis was associated with eight variables including hospitalisation ward, gender, history of diaper dermatitis in the last 6 weeks, type of nutrition such as breastfeeding and combination nutrition, diarrhea stool consistency, the frequency of changing diapers over 5 times, and increasing the frequency of defecation and use of protective creams. The age which was also a variable was not found to be significant [Table/Fig-1].
Participants demographics characteristics. Frequency and predictors of diaper dermatitis in 0-24 months children using the Chi-square test and non-linear logistic regression model (univariate).
| Factor | Diaper dermatitis n (%) | χ2 | p | β | eβ (OR) | Sig | CI (OR) |
|---|
| No | Yes |
|---|
| Hospitalisation ward |
| Paediatric wards and surgery | 69 (57) | 52 (43) | 6.4 | 0.01 | | | | |
| Neonatal ward and NICU | 43(40.1) | 64 (59.8) | 0.681 | 1.975 | 0.012 | 1.165, 3.349 |
| Gender |
| Female | 42 (41.6) | 59 (58.4) | 4.1 | 0.046 | | | | |
| Male | 70 (55.1) | 57 (44.9) | -0.545 | 0.58 | 0.043 | 0.342, 0.983 |
| Age |
| 0-6 m | 58 (42.6) | 78 (57.3) | 7.23 | 0.06 | | | | |
| 7-12 m | 30 (56.6) | 23 (43.4) | -0.56 | 0.57 | 0.08 | 0.1, 3.08 |
| 13-18 m | 13 (54.2) | 11 (45.8) | -0.46 | 0.62 | 0.29 | 0.1, 3.08 |
| 19-24 m | 11 (73) | 4 (26) | -1.3 | 0.27 | 0.03 | 0.0, 0.9 |
| History of dermatitis in the last 6 weeks |
| Yes | 37 (31.3) | 81 (68.6) | 30.8 | ≥0.001 | | | | |
| No | 75 (68.2) | 35 (31.8) | -1.546 | 0.213 | 0.001 | 0.122, 0.273 |
| Type of infants’ nutrition |
| Breast feeding | 45 (41.3) | 64 (58.7) | 7.15 | 0.049 | | | | |
| Formula | 5 (83.3) | 1 (16.7) | -1.962 | 0.0141 | 0.078 | 0.16, 0.245 |
| Supplementary food | 2 (66.6) | 1 (33.3) | -1.045 | 0.352 | 0.399 | 0.031, 3.996 |
| Mixed | 60 (54.5) | 50 (45.5) | -0.535 | 0.586 | 0.050 | 0.343, 1.000 |
| Stool consistency in the last 48 hours |
| Normal | 83 (53.2) | 73(46.8) | 8.23 | 0.049 | | | | |
| Diarrhea | 25 (37.9) | 41 (62.1) | 0.623 | 1.865 | 0.038 | 0. 035, 3.359 |
| Constipation | 4 (66.6) | 2 (33.4) | -0.565 | 0.563 | 0.521 | 0.101, 3.195 |
| Frequency of defecation in the last 24 hours |
| ≤3 times/day | Mean±SD 3.3±3.3 | Mean±SD 4.2±3.6 | | | | t=2.5 | p=0.01 | |
| ≥4 times/day | | | 0.118 | 1.125 | 0.012 | 1.025, 1.235 |
| Frequency of diaper changing in the last 24 hours |
| ≤4 times/day | 51 (57.9) | 37 (42.1) | 3.82 | 0.046 | | | | |
| 5-9 times/day | 61 (43.5) | 79 (56.5) | 0.539 | 0.715 | 0.05 | 0.997, 2.949 |
| Use of protective creams |
| No | 37 (59) | 22 (37) | 7.36 | 0.05 | | | | |
| Sometimes | 50 (48) | 54 (52) | 0.597 | 1.816 | 0.073 | 0.945, 3.490 |
| Often | 9 (39) | 14 (61) | 0.962 | 2.616 | 0.057 | 0.972, 7.039 |
| Everyday | 16 (38) | 26 (62) | 1.005 | 2.733 | 0.016 | 1.208, 6.182 |
OR: Odd ratio; CI: Confidence interval; p<0.05- statistically significant.
The highest incidence was in the age range of 0-6 months, but was not statistically significant. In the univariate regression analysis, the age group of 19-24 months was the least likely to have diaper dermatitis in comparison with the group of 0-6 months, which was statistically significant.
A multivariate logistic regression model was used to investigate the synergistic and significant variables on the incidence of diaper dermatitis. The determination coefficient, or r2, was reported as 31%-42% indicating that these variables predicted the likelihood of developing diaper dermatitis. In the multivariate logistic regression analysis [Table/Fig-2], the chances of developing diaper dermatitis in neonatal and NICU wards were as 7.7 times more than paediatrics 1 and 2, and surgery wards. The history of diaper dermatitis in the past 6 weeks increased the odds. Also, formula compared with breastfeeding and girls compared to males have reduced incidence of diaper dermatitis. The likelihood of diaper dermatitis was also higher with the use of protective cream everyday. In the Chi-square test, no significant relationships was found between the child age, residence in the city or village level of mother’s education, manner of cleaning genital and diaper dernatitis in hospitalised children.
Summary of predictive factors that were significantly associated with the incidence of diaper dermatitis in 0- 24 months children.
| Factor | β | SE | eβ (OR) | Sig | CI (OR) |
|---|
| Paediatric and surgery wards |
| Neonatal and NICU | 2.050 | 0.646 | 7.77 | 0.001 | 2.192, 27.437 |
| Gender |
| Female | | | | | |
| Male | -0.733 | 0.336 | 0.480 | 0.029 | 0.249, 0.929 |
| History of diaper dermatitis in the last 6 weeks |
| Yes | | | | | |
| No | -2.635 | 0.484 | 0.072 | <0.001 | 0.028, 0.185 |
| Child nutrition breast milk |
| Formula | -3.558 | 1.406 | 0.029 | 0.011 | 0.002, 0.448 |
| Supplementary food | - | - | - | - | - |
| Mixed food | - | - | - | - | - |
| Use of protective cream |
| No | - | - | - | - | - |
| Sometimes | - | - | - | - | - |
| Often | - | - | - | - | - |
| Everyday | 1.120 | 0.527 | 3.065 | 0.033 | 1.092, 8.602 |
SE: Standard error; OR: Odds ratio; CI: Confidence interval; p<0.05- statistically significant.
Discussion
Having enough knowledge on the incidence and risk factors of diaper dermatitis in children can be a guide for the prevention and treatment of this disorder by the healthcare team [6]. This study showed that more than half of children between 0 and 24 months suffered from diaper dermatitis. In the majority of studies, the prevalence of diaper dermatitis in healthy children has been documented. This can be a reason for the difference in the incidence of diaper dermatitis between this study and other studies. The prevalence of diaper dermatitis in the United Kingdom, Cameroon, Kenya, China and Turkey has been reported as 16, 18, 27, 44 and 67%, respectively [3,9,11,15,16]. On the other hand, there is no precise information on the incidence and severity of diaper dermatitis in children admitted to hospitals because of lack of standard reporting method [7]. In a study on children admitted to a hospital in Boston, 16% of children with urinary incontinence had diaper contact dermatitis. This study was focused on one day screening of skin integrity among infants and children [17]. In the present study, the children were examined during hospitalisation to investigate the incidence of diaper dermatitis.
In addition, findings on risk factors in different studies also show different results, which are both consistent and inconsistent with the results of the present study. Adalat S et al., in England, LI CH et al., in China and Alonso C et al., in Spain mentioned that diarrhea and frequent defecation were risk factors [9,11,18], which were in line with the results of the present study. The results of this study showed that the incidence of diaper dermatitis in girls was higher than boys, but but LI CH et al., Emdadi M et al., and Chiabi A et al., did not show a significant relationship between gender and diaper dermatitis [11,12,15]. In the present study, the level of mother’s education was not associated with the incidence of diaper dermatitis, which was in line with the results of studies by LI CH et al., but in the study by Emdadi M and Bazmamon H, a significant relationship was found between maternal education and diaper dermatitis [11,12].
In this study, the occurrence of diaper dermatitis in the age range of 0-6 months was 57.3%, which decreased with the age of children, and lowest incidence was observed in the age group of 19-24 months, and this difference was statistically significant. These findings were converse to the results of Kayaoglu S et al., and Adalat S et al., studies [4,9]. In the study of LI CH et al., there was a significant relationship between age and prevalence of diaper dermatitis. In the age group of 1-6 months, the lowest prevalence was observed, which was converse to the results of the present study [11]. The cause of diaper dermatitis in the age range of 0-6 months was more sensitivity of their skin is especially in illness conditions.
In the present study, formula feeding compared to breast feeding decreased the likelihood of developing diaper dermatitis, but Alonso C et al., reported a different result [18]. On the other hand, no significant relationship between breast feeding and diaper dermatitis by LI CH et al., found [11]. One reason for this difference could be related to difference in participants of this study and previous study. Children in this study were ill. In the present study, residence in a city or village had no relationship with diaper dermatitis, but LI CH et al., stated that living in urban areas was associated with a reduction of diaper dermatitis [11].
In contrast to LI CH et al., there was no significant relationship between the use of protective creams and the incidence of diaper dermatitis [11]. In the present study similar to the study by Adalat S et al., the incidence of diaper dermatitis in hospitalised children and the use of protective creams had a significant relationship [9]. Children with diaper dermatitis had more use of protective creams, indicating that mothers use of creams increases for the affected children.
In contrast to the studies of LI CH et al., and Adalat S et al, in this study there was a significant positive correlation between frequency of diaper changing and the incidence of diaper dermatitis. [9,11]. Frequency of diaper changing may be due to the number of fecal and urinary excretion in children that increase the incidence of diaper dermatitis.
Differences in the findings of previous studies can be related to differences in samples, methods, assessing dermatitis, and duration of follow-ups.
In this study, the incidence of diaper dermatitis in neonatal and NICU wards was 64% and in pediatric and surgical wards were 52%, which was significant in single and multivariate analysis. This can be due to the high incidence of diaper dermatitis or effects of drugs, intravenous fluid therapy, or lack of adequate maternal care to preserve the child health. Therefore, it is necessary to pay more attention to newborns and take serious measures for prevention of diaper dermatitis. In a clinical trial study, diaper dermatitis was reported in 22.2% of neonates [18], which was less than the current study.
Since almost all children were receiving antibiotics and fluid therapy, it was not possible to investigate the effect of these treatments on the development of diaper dermatitis. In a study, the use of antibiotics and 50% oral glucose, and frequent defecation were associated with diaper dermatitis, while breastfeeding and phototherapy were protective factors [18].
Due to the complications of diaper dermatitis in neonates, healthcare team members should pay special attentions in preventing and managing such skin problem and the “ABCDE” approach can be a useful guide [19]. ‘A’ is derived from the word ‘Air’, which means that the diaper area must be kept open as possible to allow the baby’s skin to come in contact with air. ‘B’ in this approach is derived from the word “barrier”, which means that protective creams are used in the diaper area to prevent dermatitis. Previous studies have examined and introduced several creams, ointments and lotions including zinc oxide cream, Vaseline gel, and hydrocolloidal dressing [18,20,21]. ‘C’ is derived from the word ‘Cleansing’, which means that each time the diaper is replaced, skin of diaper area should be washed with water slowly and without causing harm to the skin. ‘D’ is derived from the word “diaper”, which means that the high-quality type diaper is used and is changed as much as possible during the daytime every three hours and one time at night. ‘E’ is based on the word ‘Education’, which means that parents receive sufficient education regarding skin care. The results of previous studies showed that parents do not have sufficient knowledge about the prevention and management of diaper dermatitis [22].
Limitation(s)
Study was conducted among hospitalised children. So results are limited to this groups of children.
Conclusion(s)
The present study showed that more than half of Iranian children admitted to the hospital experience some degree of diaper dermatitis. The most important risk factors included hospitalisation in neonate and NICU wards, diarrhea, female gender, and previous history of diaper dermatitis. Nurses and parents should pay particular attention to preventing this problem using the results of this study. Due to the lack of studies on the incidence of diaper dermatitis and its associated risk factors in hospitalised children, as well as the more incidence in neonates, further studies are suggested.
OR: Odd ratio; CI: Confidence interval; p<0.05- statistically significant.
SE: Standard error; OR: Odds ratio; CI: Confidence interval; p<0.05- statistically significant.