Histochemical Analysis of Anterior Lens Capsule in Chalcosis Bulbi
Shweta Dhiman1, Paromita Dutta2, Vikas Kumar Jha3
1 Senior Resident, Department of Ophthalmology, Guru Nanak Eye Centre, Maulana Azad Medical College, Delhi, India.
2 Assistant Professor, Department of Ophthalmology, Guru Nanak Eye Centre, Maulana Azad Medical College, Delhi, India.
3 Postgraduate, Department of Ophthalmology, Guru Nanak Eye Centre, Maulana Azad Medical College, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shweta Dhiman, 3168-C/231, Chander Nagar, Tri Nagar, Delhi, India.
E-mail: dr.shwetadhiman@yahoo.com
Retained Intraocular Foreign Bodies (RIOFB) can cause significant visual morbidity due to the primary trauma or subsequent secondary complications. Copper Intraocular Foreign Body (IOFB)s can cause ocular changes involving cornea, lens, retina, and vitreous depending on its concentration. This report highlights the histochemical analysis of anterior lens capsule in a case of presumed chalcosis bulbi. A 27-year-old female presented with gradual decrease of vision in Left Eye (LE) since past four months. Best Corrected Visual Acuity (BCVA) in LE was Perception of Light (PL) with inaccurate Projection of Rays (PR). Slit lamp examination showed Kayser-Fleischer ring and sunflower cataract. Posterior segment evaluation revealed diffuse vitreous strands along with vitreous haze. Computerised Tomography (CT) scan orbit was obtained presuming ocular chalcosis which revealed IOFB. Removal of IOFB was not an option due to poor visual prognosis. However, the final diagnosis was cinched by using a copper detecting stain (Orcein) on the anterior lens capsule obtained during cataract surgery. Orcein staining may be used as a surrogate marker for confirmation of copper induced cataract in suspected cases of chalcosis bulbi and is a less expensive alternative to electron microscopy or spectroscopy.
Copper deposition, Intraocular foreign body, Orcein stain, Sunflower cataract
Case Report
A 27-year-old female presented with gradual painless decrease of vision in Left Eye (LE) since past four months. She had a history of minor trauma in LE with some unknown speeding object four months back while working on sewing machine. There was no history of acute inflammation in the affected eye neither had a medical opinion been taken.
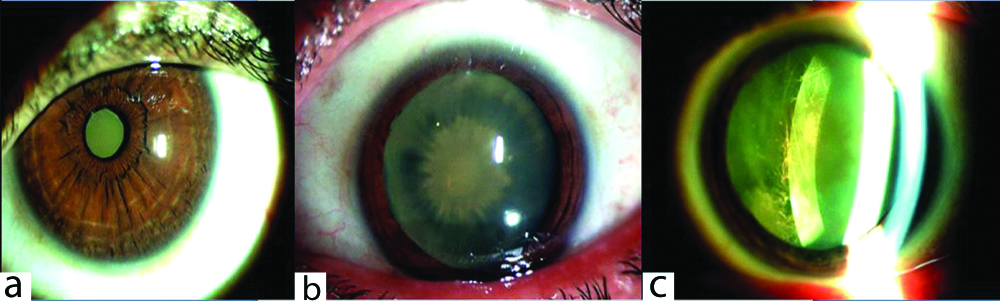
Best corrected visual acuity in Right Eye (RE) was 6/6 and LE was Perception of Light (PL) with inaccurate PR. Pupillary reactions were normal. The ocular adenexa and periorbital area was normal showing no signs of injury or any entry wound. On slit lamp examination yellow-brown granular deposition was seen in deeper layer of cornea (descemet’s membrane) all along the circumference of the corneoscleral junction suggestive of the Kayser-Fleischer ring. Anterior chamber did not show any signs of uveitis. Greenish brown central disc with radial spoke like opacities were seen in the anterior and posterior pole of lens. Posterior segment evaluation revealed diffuse vitreous strands along with vitreous haze, thus significantly obscuring disc and retinal vessels [Table/Fig-1a-c]. Examination of RE was unremarkable. There were no systemic complaints. Intra ocular pressure was 12 and 14 mm Hg.
Slit lamp photograph of left eye of patient: (a) Appearance of cataract in undilated pupil; (b) Characteristic sunflower cataract in dilated pupil; (c) Brownish deposition at posterior pole of lens with vitreous stands behind it.
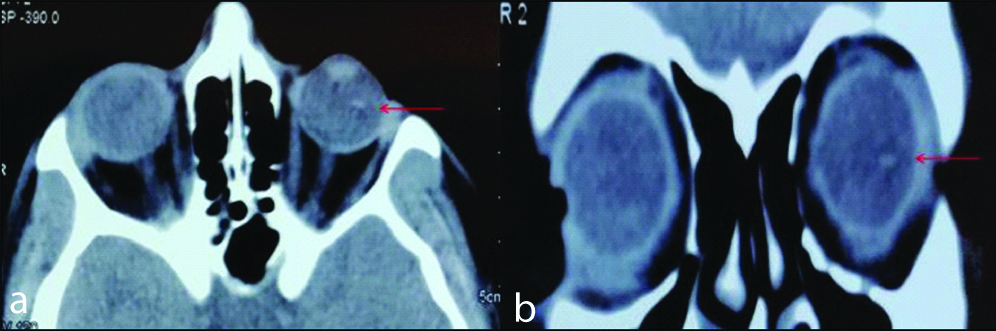
A CT scan orbit was obtained which revealed a metallic IOFB in vitreous cavity of LE and provisional diagnosis of ocular chalcosis was made [Table/Fig-2a,b]. Electroretinogram (ERG) LE showed extinguished response. Vitreo-retina consultation was sought and no intervention for IOFB removal was advised in view of poor visual prognosis. However, the patient desired for cataract removal for cosmetic reasons.
CT image of the patient showing intraocular foreign body in vitreous cavity of left eye (marked with red arrow): (a) axial section; (b) coronal section.
After counseling and obtaining consent, the patient underwent LE phacoemulsification with intraocular lens implantation (in the bag) under topical anaesthesia. The anterior lens capsule specimen (capsulorhexis tissue) was sent for histopathological analysis in 10% buffered formalin.
Post-operatively, BCVA was PL positive and PR inaccurate in LE. Funds evaluation was not possible due to dense vitreous haze. Examination of RE was normal on all with an unremarkable post-operative period.
Pathological Findings of Anterior Lens Capsule
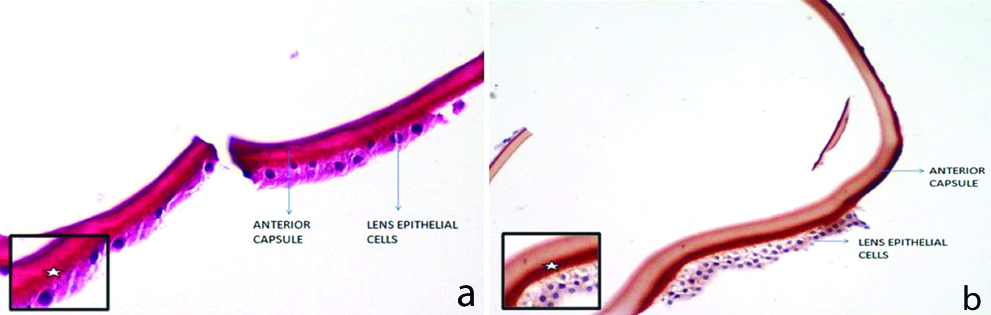
The thickness of anterior lens capsule was between 9-14 μm and contained a band of granular deposit which was densest in the posterior part of the capsule adjacent to lens epithelial cells. On Haematoxylin and Eosin (H&E) stain, the deposits were yellow-gold in colour. On Orcein staining, the deposits appeared dark brown in colour and showed a positive reaction for copper [Table/Fig-3a,b] suggestive of copper composition of IOFB.
Showing histopathology of anterior lens capsule: (a) Haematoxylin and eosin (H&E) staining- showing golden brown granular deposit in posterior layer of anterior capsule adjacent to lens epithelial cells (marked with asterisk in inset); (b) Orcein staining showing brown deposition suggestive of positive reaction for copper (marked with aterisk in inset).
Discussion
Intraocular foreign bodies represent 18-41% of all open globe injuries while endophthalmitis takes up 2-30% of open-globe injuries with retained IOFBs [1,2]. Higher copper content in a foreign body would cause significant clinical features; pure copper causes acute chalcosis with severe inflammation. If copper content is less than 85% chronic chalcosis may occur [3]. In present case, the patient had minor trauma with unknown particle while at work four months before the onset of symptoms. The decrease in vision was insidious in onset but gradually progressed to severe visual loss. Absence of history of associated redness in the eye was suggestive of indolent nature of IOFB.
Copper has an affinity for basement membranes and may be deposited over descemet’s membrane seen clinically as Kayser-Fleischer ring, over the anterior lens capsule as yellowish brown pigmentation forming sunflower cataract. Other reported changes due to copper IOFBs include fibrillary degeneration of the vitreous, vitreous fibrosis, non-granulomatous inflammatory reaction, chronic uveal inflammation, retinal pigment epithelial clumping, retinal detachment, and phthisis bulbi [4]. Current case presented with characteristic Kayser-Fleischer ring, sunflower cataract and vitreous strands which led us to the diagnosis of chalcosis bulbi. CT scan confirmed the presence of a metallic foreign body in vitreous cavity.
In early stage of metallosis, removal of IOFB may reverse ERG changes [5] but in present case ERG response was extinguished which occurs in end stage of metallosis and is suggestive of poor visual prognosis. Besides this, PR was inaccurate and vitreo-retina surgery in such eyes may increase the risk of phthisis bulbi. The patient underwent cataract removal for cosmetic purposes alone. Phacoemulsification and intra ocular lens implantation was done; anterior lens capsule obtained was studied with H&E stain and copper specific Orcein stain.
Histochemical detection of copper through a positive orcein stain has been classically described for chronic liver diseases. Orcein stain has very high sensitivity for copper and is able to detect lower copper concentrations [6]. Anterior lens capsule has been studied in cases of pseudoexfoliation syndrome and diabetic eyes through histochemical analysis [7,8]. Copper deposition in anterior lens capsule is also described in cases of multiple myeloma and Wilson’s disease [9,10]. In present case, H&E stain showed yellow-gold granular deposits in posterior part of the capsule adjacent to lens epithelial cells. Orcein staining of these deposits showed a positive reaction for copper.
Conclusion(s)
This report intends to propose Orcein staining of the anterior lens capsule as a marker for presence of copper content of retained IOFB. This technique is a cheaper and a much more widely accessible alternative to transmission electron microscopy and spectroscopy, especially in developing countries. To best of our knowledge, no prior histochemical analysis of anterior lens capsule in chalcosis bulbi has been published.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 30, 2020
Manual Googling: Feb 25, 2020
iThenticate Software: Mar 14, 2020 (11%)
[1]. Yang Y, Yang C, Zhao R, Lin L, Duan F, Lou B, Intraocular foreign body injury in children: Clinical characteristics and factors associated with endophthalmitisBr J Ophthalmol 2019 [Epub ahead of print]10.1136/bjophthalmol-2019-31491331554633 [Google Scholar] [CrossRef] [PubMed]
[2]. Kuhn F, Morris R, Posterior segment intraocular foreign bodies: Management in the vitrectomy eraOphthalmology 2000 107(5):821-22.10.1016/S0161-6420(00)00078-6 [Google Scholar] [CrossRef]
[3]. Ravani R, Kumar V, Kumar A, Kumar P, Chawla S, Ghosh S, Fleck-like deposits and swept source optical coherence tomography characteristics in a case of confirmed ocular chalcosisIndian J Ophthalmol 2018 66(11):164010.4103/ijo.IJO_437_1830355890 [Google Scholar] [CrossRef] [PubMed]
[4]. Rosenthal AR, Marmor MF, Leuenberger P, Hopkins JL, Chalcosis: A study of natural historyOphthalmology 1979 86:1956-72.10.1016/S0161-6420(79)35324-6 [Google Scholar] [CrossRef]
[5]. Ugarte M, Nicol DA, Jones NP, Charles SJ, Chronic intraocular copper foreign body and candida: A unique combinationOculImmunol and Inflamm 2009 17(5):356-60.10.3109/0927394090307537019831572 [Google Scholar] [CrossRef] [PubMed]
[6]. Bunton TE, Comparison of three histochemical staining methods for the detection of copper in white perch (Moroneamericana) with abnormal hepatic copper storageJ Comparative Pathology 1990 102(1):25-31.10.1016/S0021-9975(08)80004-7 [Google Scholar] [CrossRef]
[7]. Dark AJ, Streeten BW, Cornwall CC, Pseudoexfoliative disease of the lens: A study in electron microscopy and histochemistryBritish Journal of Ophthalmology 1977 61(7):462-72.10.1136/bjo.61.7.462889759 [Google Scholar] [CrossRef] [PubMed]
[8]. Ozdamar Y, Ozogul C, Elgin U, Acaroglu G, Helvacioglu F, Zilelioglu O, Histopathologic investigation of anterior lens capsule in diabetic eyesInvest Ophthalmol Vis Sci 2010 51(13):4599 [Google Scholar]
[9]. Shah S, Espana EM, Margo CE, Ocular manifestations of monoclonal copper-binding immunoglobulinSurvey of Ophthalmology 2014 59(1):115-23.0.1016/j.survophthal.2013.03.00224112547 [Google Scholar] [CrossRef] [PubMed]
[10]. Jang HJ, Kim JM, Choi CY, Elemental analysis of sunflower cataract in Wilson’s disease: A study using scanning transmission electron microscopy and energy dispersive spectroscopyExperimental Eye Research 2014 121:58-65.10.1016/j.exer.2014.02.00324534570 [Google Scholar] [CrossRef] [PubMed]