Outcomes of Arteriovenous Fistula and Arteriovenous Graft in Patients on Maintenance Haemodialysis in a Tertiary Care Centre
Elayaperumal Indhumathi1, Srivatsa Angraje2, Jayakumar Macha3
1 Associate Professor, Department of Nephrology, Sri Ramachandra Institute of Higher Education and Research (Deemed to be University), Chennai, Tamil Nadu, India.
2 Senior Resident, Department of Nephrology, Sri Ramachandra Institute of Higher Education and Research (Deemed to be University), Chennai, Tamil Nadu, India.
3 Professor and Head, Department of Nephrology, Sri Ramachandra Institute of Higher Education and Research (Deemed to be University), Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Elayaperumal Indhumathi, E 19, Staff Quarters, Sri Ramachandra Medical College, Porur, Chennai-600116, Tamil Nadu, India.
E-mail: drindhusrmc@yahoo.com
Introduction
Arterio-Venous (AV) fistula is the preferred choice of vascular access in all haemodialysis patients but AV graft may be an alternate option in selective patients.
Aim
To compare and evaluate the primary and cumulative patency of patients with AV Fistula (AVF) and AV Graft (AVG) undergoing maintenance haemodialysis.
Materials and Methods
This was a retrospective study of the data of 32(33.7%) patients with AVG and 63(66.3%) patients with AVF between November 2013 and December 2018. Primary survival and cumulative patency between AVF and AVG were compared using Kaplan Meier survival curves and Log Rank tests.
Results
AVF group had more males (47.6%) compared to AVG group (37.5%) but the mean age in both the groups was almost similar with 57.1 and 57.2 years respectively. Primary survival was longer for AVF than AVG (34.1 vs 25.1 months; HR-3.85; 95% CI: 1.696-8.752; p=0.001). Thrombosis occurred more in AVG than AVF (59.4% vs 28.6%; p=0.007) and hence required more interventions (40.6% vs 12.7%; p=0.003). Interventions were more salvageable in AVG group compared to AVF (34.4% vs 11.1%; p=0.01). Infections were seen only in AVG (15.6% vs Nil; p=0.003). Total cumulative patency did not show significant difference between groups (38.5 months vs 33.3 months; HR-1.508; 95% CI 0.8-2.6; p=0.152). Mortality was high in patients with AVG compared to AVF (18.8% vs 4.8%; p=0.05).
Conclusion
Based on the study findings it can be stated that AVF has better primary access survival compared to AVG and graft requires more interventions which are more salvageable than fistula. Total cumulative patency between fistula and graft do not differ significantly.
Mortality, Survival, Vascular access
Introduction
A well-functioning vascular access is the Achilles heel for the haemodialysis patients. Among different vascular accesses available AVF is considered superior in view of long patency rate, lower complications, low cost and better patient survival [1]. In 1990s, there was an increased use of AVG for haemodialysis that resulted in higher cost and hospitalisations. Hence in 2003, the “Fistula First Breakthrough Initiative” was implemented to increase the use of AVF for dialysis. Atleast 65%of patients should be dialysed through AVF by 2009 according to the revised goal and the challenge is in creating functioning AVF for dialysis [2].
Site of creation of vascular access, outcome and temporal profile between the creation of AVF/AVG and initiation of dialysis vary between different countries and choosing the best option is a big challenge. There is large shift in creation of AVF from lower limb to upper arm in USA [3,4] but in India majority of fistula creations are in upper arm. Primary failure rates of AVF range between 30 and 70% [5]. It is due to early thrombosis and failure of the fistula to mature. Risk factors include older age, coronary artery disease, peripheral vascular disease [5] with diseased vasculature requiring further procedures to create a functioning fistula. Although AVG requires more interventions to maintain patency, AVF requires more interventions for achieving maturation while waiting for the fistula to mature; Central Venous Catheter (CVCs) has to be inserted with its related complications such as sepsis, central venous stenosis preventing the placement of access [6].
Thus, an AVG and CVC use in selective group of dialysis patients is required as AVF may not be suitable for all patients. In elderly dialysis patients with multiple co-morbidities, tenuous vasculature and limited life expectancy, creation of AVF may be challenging compared to young individuals [7] as advantages of AVF are best seen with increased longevity of life [8]. Placement of AVG is advantageous in such scenarios.
Although thrombosis and infection rates are high with AVG, many newer techniques are available to manage these complications [9,10]. Patients with AVG should be kept under aggressive surveillance so that early intervention done can significantly increase the secondary patency rates [11]. Compared with thrombosed fistulae, revisions of grafts are far more successful [10-12].
In this study, the primary survival and total cumulative patency of the vascular access, complications and mortality of patients with AVF or AVG undergoing maintenance haemodialysis were analysed.
Materials and Methods
This was a retrospective study of patients on haemodialysis in a tertiary care centre where about 350 adult patients underwent maintenance haemodialysis between November 2013 and December 2018. During this period AVG was created for 32 patients and the remaining was on AVF. All patients with AVG and 63 patients with AVF, selected by simple random method in a ratio of 1:2 for the comparative purpose, were included in this study. Hospital medical records and the outpatient dialysis database were used to collect the study data. The procedures followed were in accordance with the Helsinki Declaration of 1975 that was revised in 2000. Paediatric patients undergoing dialysis were excluded from the study. Data was censored at kidney transplantation, death, withdrawal from dialysis by the patient, or at the end of the study.
As per hospital procedure, prior to vascular access creation, all patients were assessed by the vascular surgeon and access modality was selected based on medical history, physical examination including inspection and palpation of the vessels and if required ultrasound screening. Doppler study of the vessels was not done for all patients due to logistic reasons. Creation of autogenous AVF was the primary option and if the vessel size was smaller than 2 mm for radiocephalic AVF and less than 3 mm for brachicephalic AVF, with the concurrence of radiologist and vascular surgeon AVG was done. Synthetic expanded Polytetrafluoroethylene graft (ePTFE) of 6 mm size was used for all patients requiring AVG. Either straight or looped AVG was used. Cannulation of AVF in the dialysis unit was done after a minimum period of four weeks and AVG after one week.
AVG and AVF were done by the same vascular surgeon and the graft used was PTFE. Post-procedure all patients were given aspirin and clopidogrel for about 30 days. Interventions of the vascular access done include either thrombectomy or angioplasty. Brachiocephalic anastamosis in the non-dominant arm was the common site of vascular access for both AVF and AVG. Primary survival of the vascular access was defined as time in months till the first failure after creation and total cumulative survival was the time from the vascular access creation till the failure after the first intervention or till the end of the study [13]. Patient characteristics including demographic data, co-morbidities, vascular access variables such as AVF or AVG, date of creation, site, complications, duration of primary survival, interventions done and cumulative patency of the access, patient survival, laboratory values of both AVF and AVG were collected and compared between the two groups. Lab data was done at the time of creation of vascular access and culture samples were taken whenever the patient has got fever or non-healing of the access site.
Statistical Analysis
Data analysis was done using SPSS version 16. All categorical variables were expressed as numbers and percentages, continuous variables as mean±standard deviation. Values between two groups were compared by Student’s t-test or by the Mann-Whitney test, as appropriate. Fisher’s-exact test or the chi-square test was used for categorical variables. Univariate and multivariate analysis were done with access survival as the outcome variable. All statistical tests were performed two-tailed, and a significance level of p<0.05 was considered as statistically significant.
Primary access survival and cumulative patency between AVF and AVG were compared using Kaplan Meier survival curves and Log Rank tests. Hazard Ratios (HR) for graft failure relative to fistula and 95% Confidence Interval (CI) were analysed. We also evaluated the effects of patient demographics and clinical factors on primary survival, cumulative patency, complications and mortality on both AVF and AVG.
Results
Analysis of the data of 32 patients undergoing haemodialysis through AVG and randomly selected 63 patients through AVF during the period between November 2013 and December 2018 was done. Among 63 patients in AVF group 30 were men (48%) and in AVG group 12 (38%) were men (p=0.38). Majority of them were less than 65 years of age in both the groups (p=0.78). Overall, the mean age was 57 years and it was 57.1 years for AVF (47.6% males) and 57.2 years for AVG (37.5% males). Diabetes mellitus was present in 56% of patients with AVF and 59% with AVG (p=0.10). Dialysis vintage was longer in patients with AVG than with AVF (p=0.001). Patient characteristics are summarised in [Table/Fig-1] and there was no statistical difference noted between the groups.
| Variable | All (n=95) | AVF (n=63) | AVG (n=32) | p-value |
|---|
| Mean age (year) | 57.1±10 | 57.1±10.6 | 57.2±9.7 | 0.95 |
| <65 yrs | 76 (80%) | 51 (81%) | 25 (78%) | 0.78 |
| >65 yrs | 19 (20%) | 12 (19%) | 7 (21.9%) | 0.38 |
| Male | 42 (44%) | 30 (48) | 12 (38%) | 0.38 |
| Co-morbidities |
| DM | 54 (57%) | 35 (56 %) | 19 (59%) | 0.10 |
| HT | 83 (87%) | 55 (87.3%) | 28 (87.5%) | 0.97 |
| CAD | 33 (35%) | 20 (31.7%) | 13 (40.6%) | 0.39 |
| PVD | 1 (1%) | 1 (1.6%) | 0 | 0.36 |
| CVA | 7 (7%) | 2 (3.2 %) | 5 (15.6%) | 0.04 |
| LV dysfunction | 40 (42%) | 27 (42.9%) | 13 (40.6%) | 0.90 |
| Dialysis vintage (in months) | 29 | 22.35±14.7 | 42.09±27.2 | 0.001 |
| Site of access |
| Brachiocephalic | 66 | 35 | 31 | 0.34 |
| Left arm | 47 | 27 | 20 | 0.80 |
| Right arm | 19 | 8 | 11 | 0.19 |
| Radiocephalic | 28 | 28 | 0 | <0.001 |
| Femoral | 1 | 0 | 1 | 0.36 |
DM: Diabetes mellitus; HT: Hypertension; CAD: Coronary artery disease; PVD: Peripheral vascular disease; CVA: Cerebro vascular accident; LV: Left ventricle
Laboratory values of both the groups are given in [Table/Fig-2]. Wound infection was noted more in patients with AVG than with AVF (8% VS 25%, p=0.03). Primary survival was longer for AVF than AVG as shown in [Table/Fig-3] 34.1 vs 25.1 months; HR-3.85; 95% CI: 1.696-8.752; p=0.001).
| Variable | All | AVF | AVG | p-value |
|---|
| Haemoglobin (g/dL) | 8.47±1.5 | 8.7±1.6 | 7.9±1.3 | 0.02 |
| WBC count/cumm | 9921.38±4465.4 | 9848.5±4561.1 | 10062±4341.9 | 0.82 |
| Platelet count/cumm | 2.76±0.7 | 2.31±0.6 | 1.97±0.5 | 0.01 |
| Albumin (g/dL) | 3.33±0.4 | 3.39±0.5 | 3.21±0.49 | 0.09 |
| Calcium (mg/dL) | 8.34±0.91 | 8.28±0.89 | 8.44±0.85 | 0.42 |
| Phosphorous (mg/dL) | 5.42±1.7 | 5.54±1.7 | 5.17±1.6 | 0.32 |
| iPTH (pg/mL) | 327.54±284.4 | 372.9±310.9 | 238.25±185.7 | 0.06 |
| Uric acid (mg/dL) | 6.34±3.10 | 6.34±2.26 | 2.26±0.28 | 0.17 |
| Blood culture | 19 (20%) | 9 (14.3%) | 10 (31.2 %) | 0.06 |
| Urine culure | 21 (22%) | 11 (17.5%) | 10 (31.2%) | 0.19 |
| Wound culture | 13 (14%) | 5 (7.9%) | 8 (25%) | 0.03 |
| LV EF (%) | 53.92 | 54.14±7.5 | 53.50±7.7 | 0.70 |
iPTH: Intact parathyroid hormone; LV EF: Left ventricular ejection fraction
Primary survival of vascular access comparing AVF and AVG.
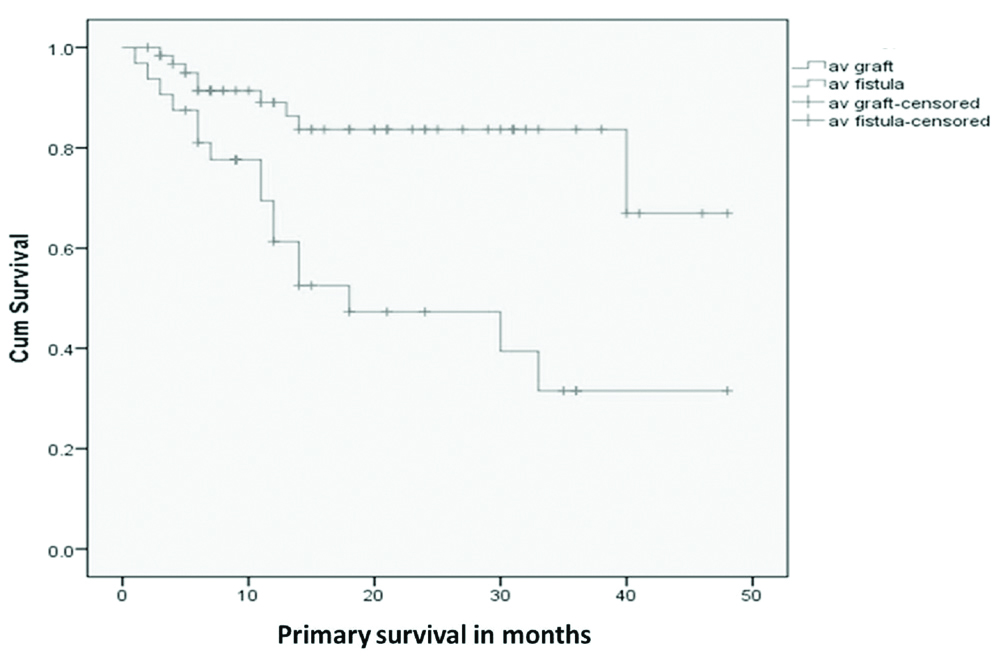
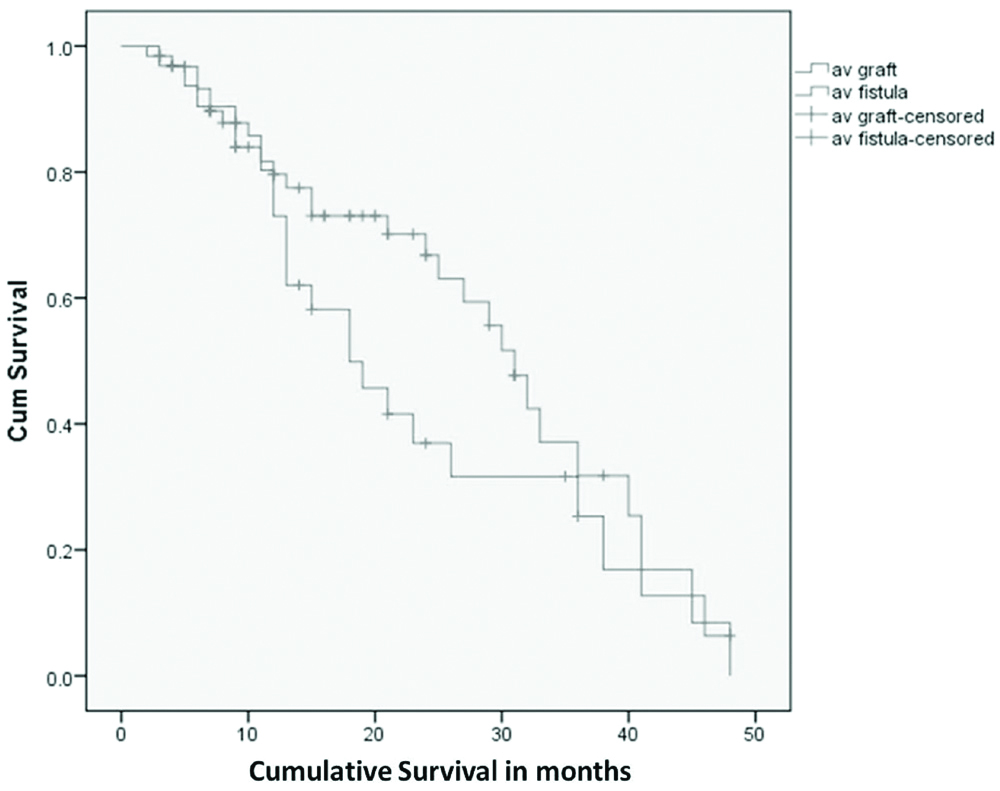
Vascular access thrombosis occurred more in AVG than AVF (59.4% vs 28.6%; p=0.007) and hence required more interventions (40.6% vs 12.7%;p=0.003). Thrombectomy was done more in patients with AVG than with AVF (34.3% vs 4.7%) and more number of patients with AVF require angioplasty than in patients with AVG (7.9% vs 6.2%). Interventions were more salvageable (34.4% vs 11.1%; p=0.01) in AVG group compared to AVF. Access infections were seen only with graft in the present study (15.6% vs Nil; p=0.003). Total cumulative patency after interventions did not show significant difference between the groups (38.5 vs 33.3 months; HR 1.508; 95% CI 0.8- 2.6; p=0.152) as shown in [Table/Fig-4]. AVG group had more mortality compared to AVF (18.8% vs 4.8%; p=0.05). Vascular access and patient outcome data are given in [Table/Fig-5]. Causes of mortality in the vascular access were sepsis (43%), coronary artery disease (29%), both sepsis and coronary artery disease (14%) and cerebrovascular accident (14%). No significant difference was noted in the primary survival of the vascular access among AVF and AVG in diabetic patients (16.5 vs 17 M; p=0.235) and in elderly patients (16.7 vs 11.57 M; p=0.126). On multivariate regression analysis as shown in [Table/Fig-6], patients with coronary artery disease, left ventricular dysfunction and male gender were at high risk for access failure (p ≤0.05) and AVF had better access survival than AVG.
Cumulative patency of the vascular access comparing AVF and AVG.
Vascular access and patient outcome.
| Variable | All (n=95) | AVF (n=63) | AVG (n=32) | p-value |
|---|
| VA infection | 5 (5.2%) | 0 | 5 (15.6%) | 0.003 |
| VA thrombosis | 37 (39%) | 18 (28.6%) | 19 (59.4%) | 0.007 |
| Interventional pro | 21 (22%) | 8 (12.7%) | 13 (40.6%) | 0.003 |
| Thrombectomy | 14 (14.7%) | 3 (4.7%) | 11 (34.3%) | 0.002 |
| Angioplasty | 7 (7.3%) | 5 (7.9%) | 2 (6.25%) | 0.602 |
| VA salvaged | 18 (19%) | 7 (11.1%) | 11 (34.4%) | 0.01 |
| Primary survival (months) | 16.6 | 34.2 | 25.1 | 0.001 |
| Total cumulative survival (months) | 18.4 | 38.5 | 33.3 | 0.15 |
| Mortality | 9 (9.4%) | 3 (4.8%) | 6 (18.8%) | 0.05 |
VA: Vascular access
Univariate and multivariate cox regression analysis of access survival.
| Variables | Univariate analysis | p-value | Multivariate analysis | p-value |
|---|
| OR (95% CI) | | OR (95% CI) | |
| AV graft | 3.853 (1.696-8.752) | 0.001* | 3.795 (1.154-12.483) | 0.028 |
| Hypertension | 3.222 (1.158-8.961) | 0.025* | 0.530 (0.149-1.890) | 0.328 |
| History of LVD | 2.608 (1.035-6.566) | 0.042* | 13.902 (2.550-75.789) | 0.002 |
| Gender | 1.362 (0.614-3.025) | 0.447 | 3.743 (1.112-12.60 | 0.033 |
| Age (years) | 0.987 (0.946-1.030) | 0.545 | 0.965 (0.919-1.014) | 0.160 |
| Diabetes mellitus | 0.739 (0.337-1.621) | 0.451 | 0.400 (0.142-1.127) | 0.083 |
| Coronary artery disease | 1.097 (0.472-2.550) | 0.830 | 5.719 (1.237-26.447) | 0.026 |
| Peripheral vascular disease | 20.45 (0.000-3081) | 0.801 | 0.123 (0.012-1.856) | 0.991 |
| History of CVA | 0.686 (0.16-2.943) | 0.612 | 1.037 (0.149-7.218) | 0.971 |
LVD: Left ventricular dysfunction; CVA: Cerebro vascular accident
Discussion
To the best of our knowledge, this study is the first one from Indian subcontinent comparing the access and survival outcome of patients with AVF and AVG though articles had been published on AVF. In this study, the primary survival of AVF was better than AVG. However the total cumulative patency after intervention did not show significant difference between AVF and AVG in consistent with majority of the studies [11,14]. But some studies had shown better cumulative patency for AVF. Maturation failure requiring more number of interventions is common in elderly population with AVF whereas patients with AVG require more interventions to maintain patency so that the cumulative patency of the vascular access do not differ significantly [13-15].
A well-functioning vascular access is the achilles heel for the haemodialysis patients. AVF is considered the preferred vascular access for haemodialysis [16,17]. Earlier the primary failure rate of AVF was low with around 10% [16,15], but now it is as high as 30%-60%. This is due to increased number of creation of AVF following “Fistula First” initiative and done in all patients requiring vascular access including elderly with multiple co-morbidities, obese and patients with prior AVF failure in whom vascular biology is not good [15,18]. The lesions causing primary failure of AVF include pre-existing arterial and venous stenosis, presence of accessory veins and an acquired lesion, juxta-anastomotic stenosis, the most common cause of primary failure. Regardless of the aetiology, the pathologic evaluation of this lesion is always consistent with neo-intimal hyperplasia. This primary failure of AVF can be prevented by doing pre-operative venous mapping, careful selection of the surgeon and monitoring of the access at four weeks. Once functional, AVF has greater patency rate with less complications and interventions compared to AVG [19].
In this study, the vascular access thrombosis occurred more in AVG than AVF (59.4% vs 28.6% p=0.007) requiring more interventions such as thrombectomy, angioplasties and surgical revision in patients with AVG compared to AVF (40.6% vs 12.7% p=0.003). Also, noted was that the thrombosed grafts had better salvage rates (8 months vs. 4 months, p<0.001) than AVF. When stenotic lesions especially that occurring at venous outflow anastamosis develop in association with an AVG, it often results in thrombosis with graft dysfunction and failure. Other causes include infection, pseudoaneurysm and intractable central vein stenosis. Although AVG tends to have more thrombosis, aggressive surveillance for graft stenosis and early intervention with advanced endovascular techniques available now has increased the secondary patency rate, significantly so that the total cumulative patency of AVF and AVG did not show marked difference. Interventions done on AVG were more salvageable than done on AVF (34.4% vs 11.1% p=0.01) in this study cohort. This is similar to other studies where the need for interventions to maintain patency was less among AVF compared to AVG [20]. Thirty percent of AV fistulae may not mature successfully for cannulation with the need for interventions [21,22].
Infection of the vascular access was noted in patients with AVG and none of the patient with AVF had infection in this study. Mortality was high with AVG group compared to AVF (18.8% vs 4.8%; p=0.05). This is similar to another nationwide study in which mortality rate for AVG was higher compared to AVF [1].
The impact of patient demographics and clinical parameters on the access and patient survival was evaluated. Men compared to women and patients with CAD had more vascular access failure in this study. Elderly patients undergoing dialysis is on the rise globally with its associated challenges. Poor vascular biology, co-morbidities and reduced life span pose a big issue as far as the vascular access is concerned. Elderly patients, particularly those with multiple co-morbidities, whose survival may not be longer can benefit from AVG rather than AVF as the benefits of AVF are not immediate [23]. No significant difference of access or patient survival of AVF and AVG group was noted between elderly and non-elderly patients in the index study. This lack of association is consistent with several previous reports [6,18].
There are conflicting reports regarding the association of outcome of patient survival and vascular access in elderly patients with AVF and AVG. In one study, lower graft survival was shown in elderly population [24]. Another study reported better patient survival with AVF in elderly male diabetic and better access patency with AVF in elderly female diabetic patients than AVG [10]. But in this study, no significant difference was noted in access survival among patients with AVF and AVG with and without diabetes in consistence with other studies [25]. On multivariate regression analysis as shown in [Table/Fig-5] AVF had better access survival than AVG and patients with coronary artery disease, left ventricular dysfunction and male gender are at high risk for access failure (p≤0.05).
Limitation(s)
Limitation of the study include small sample size and retrospective analysis of the dialysis data.
Conclusion(s)
In conclusion, based on the study findings it can be stated that AVF has better primary access survival compared to AVG and graft requires more interventions which are more salvageable than fistula. Total cumulative patency between fistula and graft do not differ significantly. AVF is the preferred choice for vascular access in haemodialysis patients but AVG has to be kept as an alternate option in a sub-group of patients with high risk of maturation failure with limited life expectancy.
DM: Diabetes mellitus; HT: Hypertension; CAD: Coronary artery disease; PVD: Peripheral vascular disease; CVA: Cerebro vascular accident; LV: Left ventricle
iPTH: Intact parathyroid hormone; LV EF: Left ventricular ejection fraction
VA: Vascular access
LVD: Left ventricular dysfunction; CVA: Cerebro vascular accident
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 23, 2020
Manual Googling: Feb 21, 2020
iThenticate Software: Mar 14, 2020 (8%)
[1]. Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J, Type of vascular access and survival among incident haemodialysis patients: The Choices for Healthy Outcomes in Caring for ESRD (CHOICE) StudyJ Am Soc Nephrol 2005 16(5):1449-55.10.1681/ASN.200409074815788468 [Google Scholar] [CrossRef] [PubMed]
[2]. Fistula First National Vascular Access Improvements Initiative. Available at: http://www.fistulafirst.org/. [Accessed January 19, 2007] [Google Scholar]
[3]. Pisoni RL, Zepel L, Fluck R, Lok CE, Kawanishi H, Süleymanlar G, International differences in the location and use of arteriovenous accesses created for haemodialysis: Results from the Dialysis Outcomes and Practice Patterns Study (DOPPS)Am J Kidney Dis 2018 71(4):469-78.10.1053/j.ajkd.2017.09.01229198387 [Google Scholar] [CrossRef] [PubMed]
[4]. Saran R, Robinson B, Abbott KC, Agodoa LY, Albertus P, Ayanian J, US renal data system 2016 annual data report: Epidemiology of kidney disease in the United StatesAm J Kidney Dis 2017 69(3):A7-8.10.1053/j.ajkd.2017.01.03628236830 [Google Scholar] [CrossRef] [PubMed]
[5]. Brown RS, Patibandla BK, Goldfarb-Rumyantzev AS, The survival benefit of “Fistula First, Catheter Last” in haemodialysis is primarily due to patient factorsJ Am Soc Nephrol 2017 28(2):645-52.10.1681/ASN.201601001927605542 [Google Scholar] [CrossRef] [PubMed]
[6]. Lacson Jr E, Lazarus JM, Himmelfarb J, Ikizler TA, Hakim RM, Balancing fistula first with catheters lastAm J Kidney Dis 2007 50(3):379-95.10.1053/j.ajkd.2007.06.00617720517 [Google Scholar] [CrossRef] [PubMed]
[7]. Lazarides MK, Georgiadis GS, Antoniou GA, Staramos DN, A meta-analysis of dialysis access outcome in elderly patientsJ Vasc Surg 2007 45(2):420-26.10.1016/j.jvs.2006.10.03517264030 [Google Scholar] [CrossRef] [PubMed]
[8]. Park HS, Kim WJ, Kim YK, Kim HW, Choi BS, Park CW, Comparison of outcomes with arteriovenous fistula and arteriovenous graft for vascular access in haemodialysis: A prospective cohort studyAm J Nephrol 2016 43(2):120-28.10.1159/00044488927022896 [Google Scholar] [CrossRef] [PubMed]
[9]. Rajan DK, Clark TW, Simons ME, Kachura JR, Sniderman K, Procedural success and patency after percutaneous treatment of thrombosed autogenous arteriovenous dialysis fistulasJournal of Vascular and Interventional Radiology 2002 13(12):1211-18.10.1016/S1051-0443(07)61967-8 [Google Scholar] [CrossRef]
[10]. Ponikvar R, Surgical salvage of thrombosed arteriovenous fistulas and graftsTherapeutic Apheresis and Dialysis 2005 9(3):245-49.10.1111/j.1774-9987.2005.00264.x15966999 [Google Scholar] [CrossRef] [PubMed]
[11]. Kakkos SK, Haddad R, Haddad GK, Reddy DJ, Nypaver TJ, Lin JC, Results of aggressive graft surveillance and endovascular treatment on secondary patency rates of Vectra vascular access graftsJ Vasc Surg 2007 45(5):974-80.10.1016/j.jvs.2007.01.01117466789 [Google Scholar] [CrossRef] [PubMed]
[12]. Shenoy S, Allon M, Beathard G, Brouwer-Maier D, Dember LM, Glickman M, Clinical trial end points for haemodialysis vascular access: Background, rationale, and definitionsClin J Am Soc Nephrol 2018 13(3):490-94.10.2215/CJN.1332121629487092 [Google Scholar] [CrossRef] [PubMed]
[13]. Lok CE, Oliver MJ, Su J, Bhola C, Hannigan N, Jassal SV, Arteriovenous fistula outcomes in the era of the elderly dialysis populationKidney Int 2005 67(6):2462-69.10.1111/j.1523-1755.2005.00355.x15882293 [Google Scholar] [CrossRef] [PubMed]
[14]. Lee T, Barker J, Allon M, Comparison of survival of upper arm arteriovenous fistulas and grafts after failed forearm fistulaJ Am Soc Nephrol 2007 18(6):1936-41.10.1681/ASN.200610111917475812 [Google Scholar] [CrossRef] [PubMed]
[15]. Lok CE, Sontrop JM, Tomlinson G, Rajan D, Cattral M, Oreopoulos G, Cumulative patency of contemporary fistulas versus grafts (2000-2010)Clin J Am Soc Nephrol 2013 8(5):810-18.10.2215/CJN.0073011223371955 [Google Scholar] [CrossRef] [PubMed]
[16]. Beathard GA, Fistula First National Vascular Access Improvement Initiative A Practioners’s Resource Guide to Haemodialysis Arteriovenous Fistulas ESRD Network 13 2004 [Google Scholar]
[17]. Tonnessen BH, Money SR, Embracing the fistula first national vascular access improvement initiativeJ Vasc Sur 2005 42(3):585-86.10.1016/j.jvs.2005.05.03016171614 [Google Scholar] [CrossRef] [PubMed]
[18]. Viecelli AK, Tong A, O’Lone E, Ju A, Hanson CS, Sautenet B, Report of the Standardised Outcomes in Nephrology-Haemodialysis (SONG-HD) consensus workshop on establishing a core outcome measure for haemodialysis vascular accessAm J Kidney Dis 2018 71(5):690-700.10.1053/j.ajkd.2017.12.00329478866 [Google Scholar] [CrossRef] [PubMed]
[19]. Harms JC, Rangarajan S, Young CJ, Barker-Finkel J, Allon M, Outcomes of arteriovenous fistulas and grafts with or without intervention before successful useJ Vasc Sur 2016 64(1):155-62.10.1016/j.jvs.2016.02.03327066945 [Google Scholar] [CrossRef] [PubMed]
[20]. Shingarev R, Maya ID, Barker-Finkel J, Allon M, Arteriovenous graft placement in predialysis patients: A potential catheter-sparing strategyAm J Kidney Dis 2011 58(2):243-47.10.1053/j.ajkd.2011.01.02621458898 [Google Scholar] [CrossRef] [PubMed]
[21]. Schild AF, Perez E, Gillaspie E, Seaver C, Livingstone J, Thibonnier A, Arteriovenous fistulae vs. arteriovenous grafts: A retrospective review of 1,700 consecutive vascular access casesJ Vasc Access 2008 9(4):231-35.10.1177/11297298080090040219085891 [Google Scholar] [CrossRef] [PubMed]
[22]. Wolford HY, Hsu J, Rhodes JM, Shortell CK, Davies MG, Bakhru A, Outcome after autogenous brachial-basilic upper arm transpositions in the post-National Kidney Foundation Dialysis Outcomes Quality Initiative eraJ Vasc Surg 2005 42(5):951-56.10.1016/j.jvs.2005.07.04216275453 [Google Scholar] [CrossRef] [PubMed]
[23]. O’Hare AM, Vascular access for haemodialysis in older adults: A “patient first” approachJASN 2013 24(8):1187-90.10.1681/ASN.201305050723813217 [Google Scholar] [CrossRef] [PubMed]
[24]. Windus DW, Jendrisak MD, Delmez JA, Prosthetic fistula survival and complications in haemodialysis patients: Effects of diabetes and ageAm J Kidney Dis 1992 19(5):448-52.10.1016/S0272-6386(12)80953-X [Google Scholar] [CrossRef]
[25]. Miller PE, Carlton D, Deierhoi MH, Redden DT, Allon M, Natural history of arteriovenous grafts in haemodialysis patientsAm J Kidney Dis 2000 36(1):68-74.10.1053/ajkd.2000.826910873874 [Google Scholar] [CrossRef] [PubMed]