Endotracheal intubation is the gold standard technique in the management of airway during anaesthesia [1,2]. However, the technique is associated with morbidities ranging from sore throat to autonomic dysfunction [2]. The LMA Classic-a first-generation Supraglottic Airway Device (SAD) introduced in 1988 has revolutionised airway management. Nonetheless, it is unable to impede the risk of gastric regurgitation and aspiration [3]. Hence, numerous alternatives to LMA such as PLMA, Laryngeal Tube Suction-D, LMA-supreme, i-gel second-generation SADs have been developed [4]. These newer devices considerably vary from the original LMA in their design and offer genuine advantages concerning versatility, safety and efficacy [3].
Several studies have compared the efficiency of i-gel against PLMA and reported that either device can maintain adequate airway sealing pressures, thus facilitating controlled ventilation [2,6,7]. However, studies on post-operative events in the Indian context are quite rare.
Therefore, this study intended to explore the efficacy of i-gel as compared to PLMA in patients undergoing elective surgeries under controlled ventilation. The primary objective was to assess the clinical performance of i-gel against PLMA in terms of insertion characteristics, haemodynamic response, airway seal pressure and MMV. The secondary objective was to assess both devices for upper airway morbidities.
Materials and Methods
This randomised clinical anaesthesia study was conducted at the Department of Anaesthesiology from 2016 to 2017, on 66 adult patients scheduled for elective surgeries under controlled ventilation. After obtaining informed consent, ethical approval from the Institutional ethical committee (STD-/EC/0383/2014), and registration in the Clinical Trial Registry India (CTRI/2018/05/013891) the study patients were recruited under the study.
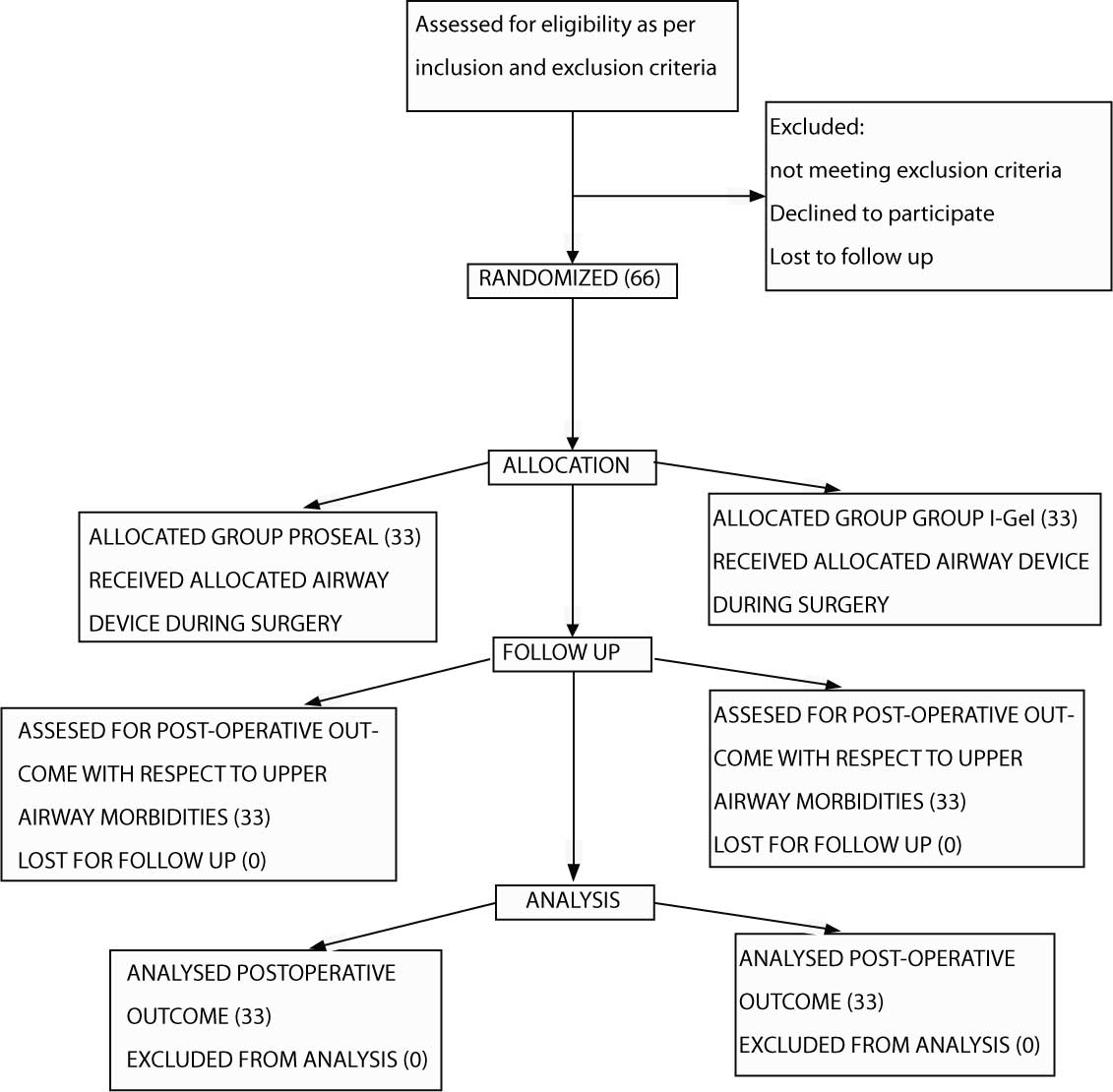
Patients between 18 and 60 years belonging to the American Society of Anaesthesiologists (ASA) Grades I, II and III were included. Patients with upper respiratory tract infection, hiatus hernia, gastrointestinal reflux disease, chronic obstructive pulmonary disease and bronchial asthma were exempted from the study. Patients with predicted difficult intubation with mouth opening <2 cm were also exempted. Eligible patients were allocated randomly into two groups, by computer-generated random numbers. Patients were categorised on the basis of type of airway maintenance device intubated, which included PLMA (group P; n=33) and i-gel (group I=33); [Table/Fig-1].
Flowchart representing patients in the study; group I, i-gel group; group P, proseal laryngeal mask airway group.
Intravenous access was secured with 18 G cannula and patients were shifted to Operation Theatre. Standard monitors like a pulse oximeter, non-invasive Blood Pressure (BP), 3 lead ECG were connected, and baseline vitals were recorded before anaesthetic induction. Patients were pre-induced with inj.midazolam 0.04 mg/kg and inj.glycopyrrolate 0.01 mg/kg, following which anaesthesia was induced with inj.fentanyl 2 mcg/kg, inj.propofol 2 mg/kg and inj.atracurium 0.5 mg/kg intravenously. After mask ventilation for 3 minutes the appropriately sized lubricated (2% lignocaine) SAD was inserted (as per manufacturer’s recommendation). Using cuff pressure manometer (portex manufacturers), PLMA cuff was inflated and maintained <60 cm H2O. Effective ventilation with the device was confirmed by bilateral chest movements on manual ventilation, square wave capnograph trace and adequate exhaled tidal volume. A 14-16-gauge suction catheter was inserted through the drain tube to decompress the stomach. Patients were maintained on oxygen and air mixture, volatile anaesthetic isoflurane (0.5-1 MAC) on IPPV and atracurium 0.1 mg/kg whenever necessary. The respiratory frequency and tidal volume were adjusted at a later stage and to maintain end-tidal carbon dioxide level between 35 to 45 mmHg, intermittent positive pressure ventilation was continued by the mechanical ventilator. The airway sealing pressure was evaluated by closing the expiratory valve of the circle breathing system at a fixed gas flow (oxygen and air) of 5 L/min and once the airway pressure reached equilibrium, the value was noted. The gas leak at seal pressure was noted if an audible sound was heard at the mouth. The following respiratory data was monitored at 1, 5, and 10 minutes after insertion of the device: peak airway pressure, along with the exhaled MMV. Any regurgitation of fluid through the airway or gastric tube was recorded. Pulse rate, systolic/diastolic BP, mean arterial pressure, peripheral capillary oxygen saturation, end tidal carbondioxide were recorded at 1, 5 and 10 minutes after insertion of the device. All patients after surgery received inj.ondansetron 0.1 mg/kg for the prevention of post-operative nausea and vomiting. Residual neuromuscular blockade was antagonised by inj.neostigmine 0.05 mg/kg and inj.glycopyrrolate 0.01 mg/kg. After gentle suctioning of oral secretions with patients in spontaneous breathing with adequate end expiratory tidal volume, SAD was removed without deflation. Post-operatively all the patients received 1g paracetamol intravenously for every 8h.
At extubation, perioperative complications caused by SADs like cough, breath holding or laryngospasm, lip or dental injury, blood staining on the device, sore throat, dysphagia, dysphonia were noted.
The complications observed were graded as follows:
Blood staining: 0-no blood staining, 1-blood staining present;
Sore throat: 0-no sore throat, 1-less severe than that experienced with common cold (mild), 2-similar to that experienced with common cold (moderate) and absence of congestion on examination of the throat, 3-more severe than that experienced with common cold with presence of congestion on examination of throat;
Dysphagia: 0-no difficulty; 1-discomfort on swallowing (mild); 2-pain on swallowing (moderate); 3-severe pain on swallowing (severe).
Hoarseness: 0-no hoarseness; 1-noted by patient (mild); 2-obvious to observer (moderate); and 3-aphonia (severe).
Based on a previous study [7], the proportion of complications of blood staining was 1% in i-gel whereas 20% in PLMA and this difference was statistically significant. In this study expecting the similar difference with the power of 90 and alpha error of 5%, a minimum sample size of 33 in each arm was required.
Statistical Analysis
SPSS software v17 was used to analyse the data. All the quantitative parameters were expressed as Mean±SD while all the qualitative parameters as percentage (%). The mean insertion time between the groups was compared using Mann-Whitney test and post-hoc ANOVA with Bonferroni adjustment, while the complications between the groups were compared using Chi-square test. p<0.05 was considered statistically significant.
Results
Baseline characteristics including operative data of the patients are shown in [Table/Fig-2]. Most of the patients in the study were in the age group of 41 to 60 years (Group P: 42.42%; Group I: 51.52%) with male predominance (Group P: 60.6%; Group I: 54.55%). Age, gender, height, weight, Body Mass Index (BMI), ASA status, duration of surgery (p>0.05) were comparable between the groups.
Patient baseline characteristics and operative data.
| Variables | Group i-gel, (n=33) | Group PLMA, (n=33) | p-value |
|---|
| Age (years)* | 37.18±14.06 | 38.81±13.76 | 0.69 |
| Gender |
| Male | 18 (54.55%) | 20 (60.6%) | 0.81 |
| Female | 15 (45.45%) | 13 (39.39%) |
| Weight (kg)* | 58.81±10.14 | 61.67±13.82 | 0.34 |
| Height (cm)* | 156±6.481 | 157.73±7.81 | 0.61 |
| BMI (kg/m2)* | 24.04±3.18 | 24.68±4.75 | 0.52 |
| ASA Grade |
| Grade 1 | 13 (39.39) | 20 (60.60) | 0.20 |
| Grade 2 | 13 (39.39) | 10 (30.30) |
| Grade 3 | 7 (21.21) | 3 (9.09) |
| Duration | 91.54±47.89 | 91.51±55.41 | 0.58 |
Group I: i-gel group; Group P; Proseal laryngeal mask airway group; *Data expressed in terms of Mean±SD; ASA: American society of anaesthesiologists
Most of the patients in Group I received size 4; while all the patients in group P received size 0 and the difference was found to be significant. PLMA or i-gel insertion was achieved in the first attempt in most of the patients; however not significant. The mean airway seal pressure and MMV were also comparable among both the groups (p≥0.05; [Table/Fig-3]).
Comparison of clinical performance of PLMA and i-gel.
| Variables | Group I, (n=33) | Group P, (n=33) | p-value |
|---|
| Size of SAD |
| 0 | 0 | 33 (100) | <0.05 |
| 3 | 7 (21.21) | 0 |
| 4 | 23 (69.70) | 0 |
| 5 | 3 (9.09) | 0 |
| Insertion attempts |
| 1 | 28 (84.8%) | 28 (84.8%) | 0.57 |
| 2 | 5 (15.2%) | 4 (12.1%) |
| 3 | 0 | 1 (3%) |
| Airway seal pressure (mmH2O) | 23.06±2.92 | 21.27±4.332 | 0.05 |
| Minimum minute ventilation (L/min) | 4.14±0.51 | 4.54±0.879 | 0.09 |
Group I: I-gel group; Group P: Proseal laryngeal mask airway group; SAD: Supraglottic airway devices
Overall, the HR, mean arterial pressure, end-tidal carbondioxide, SPO2 (peripheral capillary oxygen saturation), systolic and diastolic blood pressures were comparable in both groups (ANOVA p>0.05). Also, post-hoc analysis of ANOVA, as depicted in [Table/Fig-4], showed no significant difference in haemodynamic parameters (Bonferroni adjusted p>0.05) between the groups along all the time points.
Haemodynamic response to insertion of both devices at different points.
| Haemodynamic parameter | Type | Time, Mean (SD) |
|---|
| Baseline | 1 min | 5 min | 10 min | 60 min | 6 h | 24 h |
|---|
| Heart rate# | i-gel | 84.27 (11.06) | 78.55 (10.66) | 75.61 (10.76) | 74.03 (10.17) | 82.67 (8.36) | 80.42 (7.73) | 80.52 (7.42) |
| PLMA | 83.67 (14.64) | 80.12 (12.72) | 74.42 (11.96) | 73.42 (11.83) | 85.42 (14.87) | 82.94 (11.69) | 82.79 (9.90) |
| Adj. p-value | | 0.85 | 0.587 | 0.674 | 0.824 | 0.357 | 0.306 | 0.295 |
| Mean arterial pressure (mmHg)# | i-gel | 94.30 (14.84) | 83.2 (11.91) | 81.88 (10.38) | 83.58 (12.25) | 94.18 (12.83) | 90.67 (8.47) | 90.30 (7.80) |
| PLMA | 95.73 (20.80) | 83.1 (14.4) | 83.12 (13.54) | 85.73 (16.02) | 94.03 (16.75) | 92.36 (13.17) | 89.73 (11.81) |
| Adj. p-value | | 0.75 | 0.978 | 0.677 | 0.542 | 0.967 | 0.536 | 0.816 |
| Systolic blood pressure (mmHg)# | i-gel | 134.61 (22.57) | 112.67 (18.52) | 113.30 (16.36) | 114.06 (16.47) | 134.61 (22.03) | 128.79 (18.57) | 127.42 (15.49) |
| PLMA | 140.18 (20.24) | 116.58 (19.27) | 118.30 (18.02) | 120.09 (18.83) | 134.33 (20.33) | 132.82 (20.87) | 127.45 (16.95) |
| Adj. p-value | | 0.295 | 0.404 | 0.242 | 0.178 | 0.958 | 0.41 | 0.994 |
| Diastolic blood pressure (mmHg)# | i-gel | 75.03 (11.44) | 69.27 (10.91) | 67.52 (10.41) | 68.39 (15.83) | 75.61 (9.17) | 73.67 (7.10) | 72.91 (6.88) |
| PLMA | 81.06 (16.86) | 69.70 (16.64) | 67.97 (16.30) | 70.97 (16.46) | 77.21 (16.02) | 74.39 (13.55) | 75.52 (12.97) |
| Adj. p-value | | 0.094 | 0.894 | 0.893 | 0.519 | 0.619 | 0.786 | 0.878 |
| SPO2# | i-gel | 99.03 (1.23) | 99.85 (0.36) | 99.94 (0.24) | 99.97 (0.17) | 99.58 (0.96) | 99.55 (0.93) | 99.64 (0.85) |
| PLMA | 98.88 (1.31) | 99.88 (0.33) | 99.94 (0.24) | 99.94 (0.24) | 99.88 (0.33) | 99.55 (0.86) | 99.61 (0.78) |
| Adj. p-value | | 0.638 | 0.725 | 1 | 0.562 | 0.094 | 1 | 0.882 |
| End tidal carbon dioxide (mmHg)# | i-gel | 28.33 (1.64) | 29.03 (1.38) | 29.52 (1.50) | 29.85 (1.52) | | | |
| PLMA | 28.52 (2.39) | 28.88 (1.69) | 29.73 (1.48) | 28.91 (4.92) | | | |
| Adj. p-value | | 0.958 | 0.794 | 0.714 | 0.106 | | | |
#non-significant; Adj: Adjusted; PLMA: Proseal laryngeal mask airway group; SPO2: Peripheral capillary oxygen saturation
Upper airway morbidity was similar in both devices [Table/Fig-5]. The incidence of bloodstaining was more common with group P (6/33) compared to group I (1/33), found to be statistically significant. Sore throat was seen more in the first-hour post-surgery, however the incidence reduced in 24 hour. Dysphagia and odynophagia were less complained symptoms of sore throat at first hour, however, this reduced in both groups at 24 hour. Although two cases (grade 1) had sore throat with PLMA at 24 hour, with overall severity, the case of i-gel had sore throat of grade 2. Although post-operative airway morbidities were similar in both groups, their incidence in PLMA group was higher than in i-gel group.
Upper airway morbidity in both groups.
| Complications | Group I, (n=33) | Group P, (n=33) | p-value |
|---|
| Intraoperative | |
| Blood staining | No | 32 (96.97%) | 27 (81.81%) | 0.10 |
| Yes | 1 (3.03%) | 6 (18.18%) |
| Post-operative |
| Cough | No | 27 (81.82%) | 26 (78.78%) | 1 |
| Yes | 6 (18.18%) | 7 (21.21%) |
| Hoarseness | No | 32 (96.97%) | 0 | 1 |
| Yes (mild) | 1 (3.03%) | 0 |
| Sore throat |
| 1 h | 0-no sore throat | 23 (69.7%) | 21 (63.64%) | 0.54 |
| 1-mild | 9 (27.27%) | 8 (24.24%) |
| 2-moderate | 1 (3.03%) | 3 (9.09%) |
| 3-Severe | 0 | 1 (3.03%) |
| 6 h | 0-no sore throat | 28 (84.85%) | 24 (72.73%) | 0.48 |
| 1-mild | 4 (12.12%) | 7 (21.21%) |
| 2-moderate | 1 (3.03%) | 2 (6.06%) |
| 24 h | 0-no sore throat | 32 (96.97%) | 31 (93.94%) | 0.22 |
| 1-mild | 0 | 2 (6.06%) |
| 2-moderate | 1 (3.03%) | 0 |
| Dysphagia |
| 1 h | 0-no difficulty | 32 (96.97%) | 27 (81.82%) | 0.11 |
| 1-mild | 0 | 3 (9.09%) |
| 2-moderate | 1 (3.03%) | 3 (9.09%) |
| 6 h | 0-no difficulty | 32 (96.97%) | 30 (90.90%) | 0.13 |
| mild | 0 | 3 (9.09%) |
| moderate | 1 (3.03%) | 0 |
| 24 h | 0-no difficulty | 32 (96.97%) | 32 (96.97%) | 0.36 |
| 1-mild | 0 | 1 (3.03%) |
| 2-moderate | 1 (3.03%) | 0 |
| Odynophagia |
| 1 h | No | 32 (96.97%) | 27 (81.81%) | 0.05 |
| Yes | 1 (3.03%) | 6 (18.18%) |
| 6 h | No | 32 (96.97%) | 32 (96.97%) | 1 |
| Yes | 1 (3.03%) | 1 (3.03%) |
| 24 h | No | 32 (96.97%) | 0 | 0.31 |
| Yes | 1 (3.03%) | 0 |
Group I: I-gel group; Group P: Proseal laryngeal mask airway
Discussion
The study compared the two SADs, PLMA and i-gel, and found that both devices were comparable for airway sealing pressures, MMV, and post-operative airway morbidities. Although the post-operative airway morbidities were noted more for PLMA than i-gel, the mean incidence was not to a statistically significant degree.
Haemodynamic responses are lesser with SADs when compared to tracheal tubes during the intubation and extubation period [2]. In this study as well, responses to the two SADs were similar. Insertion in the first attempt was largely similar in either group in this study. However, PLMA insertion appeared to be slightly disappointing, requiring more attempts due to its foldable cuff, which upon deflation tended to become too soft and cause malpositioning. More commonly, this happens when the tip lays over the tracheal opening instead of oesophageal opening. At such a point, the gas leak would be more from the gastric port. Furthermore, sealing would also be impaired because of this malpositioning. However, none of the cases encountered such a problem in this study; therefore no comment can be made on the cause, findings and management of such cases. Similar studies have also stated that the first attempt success rate was higher with i-gel [1,11].
The mean airway sealing pressure in this study was significantly higher in the i-gel group compared to the PLMA group. Whereas, previous studies [7,11,12] had noted that PLMA had a higher sealing airway pressure. In this study, seal pressure varied upon i-gel insertion and about 30 minutes later. The i-gel, which is made of styrene-ethylene butadiene styrene, a thermoplastic elastomeric material, accommodates itself in the perilaryngeal space, conforming to the anatomy of the perilaryngeal space and forms a seal according to the body temperature. This is a probable reason behind the difference in seal pressure upon insertion and a few minutes later. None of the previous studies tested this hypothesis of variation in the airway seal pressure, and more studies in future may validate the present findings. In this study, MMV was comparable between the PLMA and i-gel groups, indicating either device to be efficient for positive pressure ventilation. Overall, the study indicates that both devices are efficient for controlled as well as positive pressure ventilation. Furthermore, both deliver adequate tidal volumes and attain airway seal needed for good ventilation and protection against aspiration.
Inflatable masks cause venous compression, tissue distortion and nerve injury [13]. The incidence of complications was higher in the PLMA group, comparable to a study by Singh I et al., [11]. Moreover, cases who received PLMA in the third attempt in this study had blood on the device and were found to have sore throat of grade 2, dysphagia of grade 2 and odynophagia, which however resolved within 24 hour. Although it has been reported that insertion attempts do not correlate with the increased incidence of sore throat, in this study there was a direct correlation, suggesting that increased number of insertion attempts might have led to airway trauma causing increased post-operative airway symptoms. The cases complaining of sore-throat immediately after operation were minimal within the i-gel group in this study, similar to other studies [9,14]. Furthermore, the incidence of hoarseness and dysphagia were also less evident in the i-gel group, which correlated well with other similar studies [6,15,16]. The lower incidence of post-operative upper airway morbidities in this study might be due to the soft seal non-inflatable mask of i-gel, which aids in easier insertion without tissue compression [17,18]. Incidence of laryngospasm, bronchospasm, regurgitation, aspiration, lip or dental injury was also not present in either group. Overall, findings of this study suggest that the PLMA has a higher incidence, compared to i-gel, of number of patients complaining of post-operative upper airway morbidities (sore throat, dysphagia, hoarseness of voice, odynophagia) along with severity of symptoms. All the upper airway morbidities were observed more in the initial first post-operative hour than in the subsequent hours.
Limitation(s)
The present study has potential limitations. Firstly, unblinded anaesthesiologists collected the data; therefore, there is a possibility of bias. Secondly, the insertion of both devices was done by a single experienced user and hence the findings may not apply to inexperienced users, such as residents. Thirdly, this study was performed on non-obese patients with normal airways and hence these findings cannot be inferred to apply to obese patients or those with difficulty in airway management. Finally, device insertion was performed after administering muscle relaxant for neuromuscular blockade; therefore, this might also affect the airway seal pressure and lower the values of oropharyngeal leak pressure.
Conclusion(s)
PLMA and i-gel both were found to be efficient SADs for intraoperative airway maintenance, while the incidence of post-operative airway morbidities was less in i-gel group. Significantly, low incidence of blood on device and high airway seal pressure with i-gel indicates that it might be an ideal alternative to PLMA among patients undergoing elective surgeries undercontrolled ventilation.
Group I: i-gel group; Group P; Proseal laryngeal mask airway group; *Data expressed in terms of Mean±SD; ASA: American society of anaesthesiologists
Group I: I-gel group; Group P: Proseal laryngeal mask airway group; SAD: Supraglottic airway devices
#non-significant; Adj: Adjusted; PLMA: Proseal laryngeal mask airway group; SPO2: Peripheral capillary oxygen saturation
Group I: I-gel group; Group P: Proseal laryngeal mask airway