A Forearm Gossypiboma which Mimicked a Deep Seated Abscess: A Case Report from a Tertiary Care Institute in Eastern Part of India
Sanyal Kumar1, Sanjay Kumar Pandey2
1 Senior Resident, Department of Physical Medicine and Rehabilitation, AIIMS Patna, Patna, Bihar, India.
2 Associate Professor and Head, Department of Physical Medicine and Rehabilitation, AIIMS Patna, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Sanyal Kumar, Room No. G-11, PG-1 (Hostel 11), AIIMS Patna, Patna, Bihar, India.
E-mail: kumar.sanyal@gmail.com
Gossypiboma is a foreign body that contain non absorbable cotton matrix, retained in tissue after a surgical procedure. 24-year-old male who came to our outpatients department with soft cystic painful swelling over ulnar side of Left forearm having sero-sanguinous discharge for last 6 months. Open reduction and internal fixation was done for fracture distal end radius, 2 years back followed by plate in situ which was removed 6 month back. Radiograph showed soft tissue swelling with healed fracture and multiple screw foot print present over distal end of radius. MRI showed thick calcified abscess, which appear isointense on T1WI and heterogeneous hyper intense on T2WI in intramuscular and intermuscular plane in posterior compartment of right forearm. Incision and drainage was done through open exploration with extraction of retained gauge piece and removal of dead and necrosed tissue. Postoperative period was uneventful and patient was well during 3 month follow-up.
Forearm abscess, Foreign body, Musculoskeletal system
Case Report
A 24-year-old male reported a not so common case of gossypibomas in the forearm. The patient presented with a painful nonpulsatile soft cystic swelling of 3 × 4 cm over ulnar aspect of right forearm, underlying skin raised, red and warm with serosanguineous discharge since past 6 months. Pain was continuous in nature with only partial relief after taking some pain killers on his own.
There was no history of systemic illness like fever, loss of appetite or weight loss. He was operated for forearm fracture (distal end radius) through open reduction and internal fixation which was done 2 years back at some private hospital in eastern part of India. At same hospital setting removal of internal fixator was performed 6 months after surgery followed by painful swelling over ulnar side of right forearm.
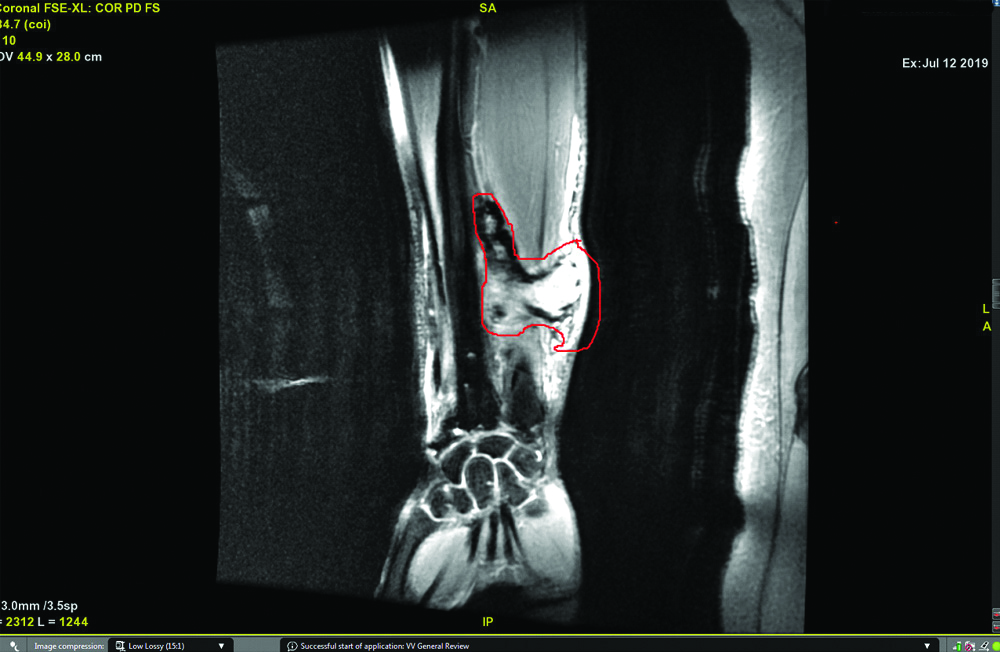
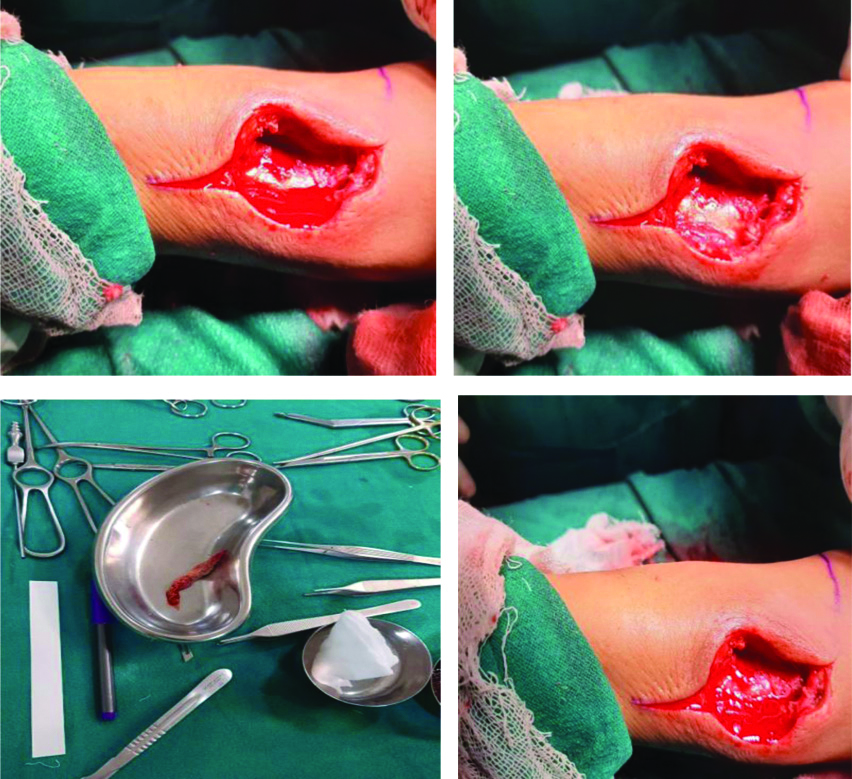
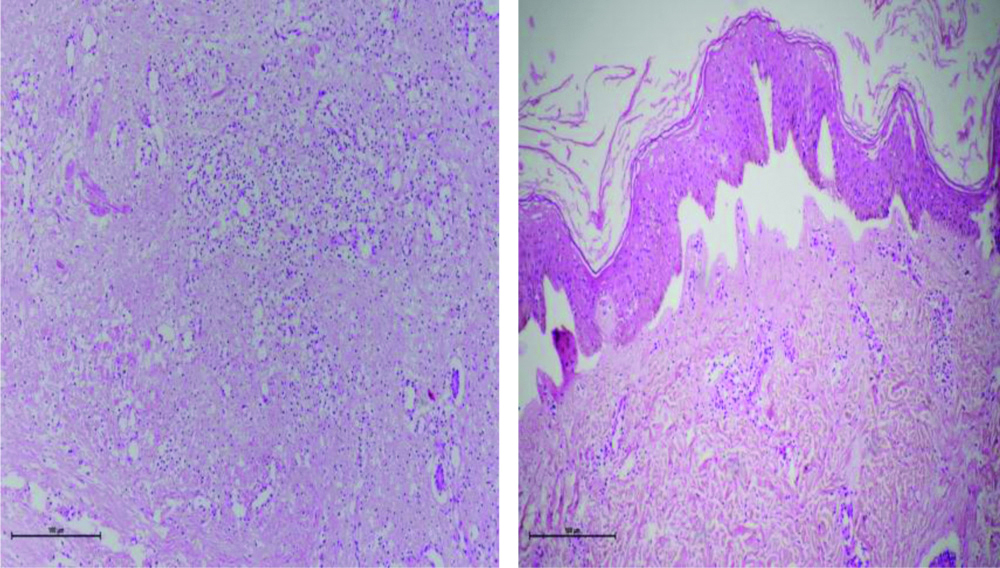
General and systemic examination was within the normal limit. On local examination swelling was painful, soft cystic in nature, skin was nonadherent to superficial structure, fixity was present with deeper structures, sign of local inflammatory reaction was present over underlying skin. Based on the clinical findings provisional diagnosis as a deep seated abscess was formed postoperatively. On laboratory examination, WBC counts within the normal range (7460/μL; normal reference range, 4,000-10,000/μL), differential count raised eosinophil (11%; normal reference range, 1-6%), ESR and CRP were raised (40 mm/hr and 44 mg/L; normal reference range, 0-10 mm/hr and 0-5 mg/L respectively). On digital X-ray right forearm shows soft tissue swelling with old heeled fracture and multiple screws foot print present over distal end of radius. MRI right forearm shows 8.3×1.6×1.0 cm (CC×TR×AP) thick walled abscess, appearing isointense on T1WI, hetregenous hyperintense on T2WI in the posterior compartment of right forearm, with intramuscular and intermuscular fascial plane components. Outer rim enhance after gadolinium contrast. The abscess cranially predominantly within deeper muscular plane and caudally it extend superficial muscular plane. On the basis of clinical and radiological finding preoperative possible diagnosis of deep seated abscess extending from deeper to superficial plane of forearm muscles made. With unusual finding in MRI [Table/Fig-1] we kept in mind foreign body in situ as a differential diagnosis. Incision and drainage was performed through open exploration followed by extraction of a foreign body removed from facial plane, extending from deep to superficial muscular plane. Multiple adhesions with moderate amount of dead and necrosed tissue were excised. Extracted foreign body, yellowish in colour with multiple cotton thread apparently made up of cotton matrix [Table/Fig-2] and subsequently confirmed by histopathology [Table/Fig-3] was indeed a gauge piece surrounding yellow chalky like material with granulation tissue. Postoperative period was uneventful and patient was informed about extraction of foreign material which is most likely cotton matrix. Stitches were removed after 10 days. Pain, swelling and local inflammatory reaction of underlying skin were subsided.
Preoperative MRI finding shows hetregenous hyperintense on T2WI in the posterior compartment of right forearm, with intramuscular and intermuscular fascial plane components. Outer rim enhance after gadolinium contrast.
Intraoperative finding of incision and drainage followed by removal of dead and necrosed tissue along with removal of gauge piece.
Histopathology shows skin covered tissue with underlying granulation tissue with focal area of necrosis with textile fiber. (H&E stain)
Discussion
These retained surgical gauge piece inside the patient body after many surgical procedure are mainly iatrogenic [1,2,3]. Gawande AA et al., studied 61 patients with retained foreign bodies after previous surgery and found surgical sponge in 69% of subjects and instruments such as clamp, retractor, and electrode in 31% [4]. Incidence of gossypiboma is more common in abdomino-pelvic surgeries as compare to surgeries involving extremities, including the paraspinal areas [5,6]. The space is very small in operating site of extremity especially forearm; incidence of gossypiboma in extremity is not very common. Gossypibomas are sub classified into an acute and a chronic form [5,6,7]. In the acute form, the patients often become symptomatic in the early postoperative period. This phase is dominated by exudative reactions with formation of abscess and fistulous tracts to the skin surface [8,9]. The chronic form is categorised by a well-encapsulated aseptic foreign body granuloma, with non-specific subjective symptoms [8,10]. In the present case there is acute presentation of gossypiboma; with formation of abscess associated with serosanguinous continuously discharging fistulous tract. Many risk factors have been reported for leaving sponge and instruments, but these are more common in emergency setup, as there is risk of an unexpected change in procedure, long duration surgery, practice of sponge counts is not very regular, less experienced staff, inadequate number of staff, frequent change in operating room staff, patients’ unstable condition, and obesity of patients [8,9]. Making the diagnosis of gossypibomas is clinically challenging. Thus various imaging modalities are required for the same. If gauge piece contain radiopaque marker it can easily be identified on plain and digital X-ray, without marker it difficult to identify [1]. They appear to have inconstant magnetic resonance signal intensity that is subjected to the amount of fluid and protein associated with the lesion. On MRI they appear as well-defined masses with fibrous capsules exhibiting low signal intensity on T1-weighted imaging, high central signal intensity with a hypo intense rim on T2-weighted imaging and strong peripheral enhancement on contrast-enhanced images. The major difference arises from T2-weighted images characterised by heterogeneous signals composed of mainly dark signals. Since gauze fibres appear as low intensity strips on T2-weighted imaging [11], this may characterise gossypiboma on MRI. The mass in the present case showed iso- to hypo intense signal intensity on T1-weighted imaging with peripheral rim enhancement with low heterogeneous signal intensity on T2-weighted imaging in coherence with the literature [5]. Most presented case reports demonstrated that the clinical symptoms associated with this lesion were treated satisfactorily by complete removal of the masses [5]. On differential aspect we decide to explore and remove the content. Foreign body unintentionally left during a surgical procedure have serious medicolegal aspect and underreported. Patient were informed regarding the surgical finding and counselled. Medical and legal records are imported in this case so kept safe in medical record section of hospital [8,11].
Similar reported cases with their mediolegal aspects are quoted in [Table/Fig-4]. Preventive measures are very important to avoid retention of gauge piece during surgical procedure; recommended WHO guidelines for safe surgery to minimise such complications should strictly be followed. WHO surgical safety checklist helps the surgeon and its team to minimise intraoperative complication during a surgical procedure. Checklist divided into three phases. First phase start with before and after induction of anaesthesia, second phase before surgical incision and third phase after wound closure. Each phases verbally coordinated by appropriate team member or coordinator. First phase coordinator check and insure with the anaesthetist, patient’s identity, procedure, site of operation, consent for surgery and anaesthesia, risk of blood loss during procedure, airway difficulty, allergic reaction and also look for anaesthesia machine and anaesthetic medication. During this phase surgeon also help the anaesthetist for blood loss, procedure, allergies and other complication regarding procedure. During second phase each team members introduce him/her and designated work profile during procedure. All team members verbally confirm the patient’s identity, procedure and site of operation. Coordinator also looks for prophylactic antibiotic have been given before 60 minute of procedure. At the third phase after wound closure team member further review the procedure and count the instrument and gauge piece used. Coordinator check and confirmed the instruments and gauge piece used and also labelled the specimen receive during procedure. Coordinator address the issue happened during the procedure. After successfully completion of checklist, patient shifted to recovery room with proper discussion of postoperative management. WHO checklist is complicated so one person should be assigned till all the members are familiar with the checklist [2].
Gossypibomas cases reported with their medicolegal aspects.
| References | Age/gender | Initial surgery | Interval Period | Preliminary diagnosis | Procedure/Intraoperative finding | Medico legal issues |
|---|
| M EI Fortia et al., [12] | 41 Y/F | Open cholicystectomy | 3 months | Primary small bowel tumour | Explorative laprotomy f/b extraction of gauge piece | Informed to patientNo malpractice claim.Avoid such postoperative foreign body retention radiologist should also take part and performed pre and post operative diagnostic procedure. |
| Garg M and Aggarwal AD, [5] | 41 Y/F | Abdominal hysterectomy | 2 months | Inconclusive? suspicious of foreign body | Explorative laprotomy f/b extraction of gauge piece | Informed to patientNo malpractice claim.Local law authority were involve to define responsibilities and compensation in such medico legal cases |
| Biswas RS et al., [9] | 39 Y/M45 Y/F | Emergency appendicectomyOpen cholecystectomy | One month7th day | Intestinal obstructionStromal tumour | Explorative laprotomy f/b removal of intraluminal gauge pieceExplorative laprotomy f/b removal of intraluminal gauge piece | Not reported.For such incident medical fraternity mainly operated surgeon may prosecuted under section 304A IPC. |
| Arora RK and Johal KS, [13] | 18 Y/M | Open reduction f/b plate and screw fixation of periprosthetic fracture femur | 2 years | Failed implant with soft tissue calcification | Freshening of bone f/b interlocking nail fixation of fracture segment with removal gauge piece from fracture segment | Not reported.Surgeon is fully responsible for misshapen. Strict training is schedule to prevent such complication |
| Boussaid M et al., 2017 [10] | 47 Y/F | Mastectomy | 4 years | Recurrence | Exploration f/b removal of mass | Not informedLast operation is considered for such malpractice if patient had multiple surgeries at same site and Supreme court expedite recoupment for such patients. |
Conclusion(s)
Extremity gossypiboma especially in forearm is not so common. Nonspecific clinical and radiological feature gossypiboma are difficult to diagnose. If a patient presented with swelling with or without discharging sinus over a previously operated site, gossypiboma must include in the differential diagnosis. Prevention is best to avoid retention of gauge piece during a surgery, counting and matching the sponge pieces before and after surgery. In addition radiopaque gauge piece marker should be used to easily identify retain gauge piece.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 16, 2019
Manual Googling: Feb 20, 2020
iThenticate Software: Feb 29, 2020 (9%)
[1]. Maier M, Bratschitsch G, Friesenbichler J, Bodo K, Leithner A, Holzer LA, Pathologic fracture of the distal humerus due to a textilomaJ Shoulder Elbow Surg 2016 25:e304-08.10.1016/j.jse.2016.07.02427663747 [Google Scholar] [CrossRef] [PubMed]
[2]. Rydenfalt C, Johansson G, Odenrick P, Åkerman K, Larsson PA, Compliance with the WHO surgical safety checklist; Deviations and possible improvementsInt J Qual Health Care 2013 25:182-87.10.1093/intqhc/mzt00423335056 [Google Scholar] [CrossRef] [PubMed]
[3]. Malot R, Meena DS, Gossypiboma of the thigh mimicking soft tissue sarcoma: 176 case report and review of literatureJ Orthop Case Rep 2012 2:21-24. [Google Scholar]
[4]. Gawande AA, Studdert DM, Orav EJ, Brennan TA, Zinner MJ, Risk factors for retained instruments and sponges after surgeryN Engl J Med 2003 348:229-35.10.1056/NEJMsa02172112529464 [Google Scholar] [CrossRef] [PubMed]
[5]. Garg M, Aggarwal AD, A review of medicolegal consequences of gossypibomaJ Indian Acad Forensic Med 2010 32(4):0971-73. [Google Scholar]
[6]. Pezzilli R, Mauloni PA, Pagano N, Gossypibomas as a rare cause of common bile duct dilationHepatobiliary & Pancreatic Diseases International 2019 18:498-500.10.1016/j.hbpd.2019.07.00931378473 [Google Scholar] [CrossRef] [PubMed]
[7]. Butt UI, Shafiq AB, Umar M, Ashfaq M, Ayyaz M, Transmigration and spontaneous passage of a gossypiboma documented on contrast studyAnnals of Medicine and Surgery 2019 38:42-44.10.1016/j.amsu.2018.10.02230655970 [Google Scholar] [CrossRef] [PubMed]
[8]. Lotfinia I, Mahdkhah A, Spinal textiloma after diskectomy: A case report and review of the literatureWorld Neurosurg 2020 134:343-47.10.1016/j.wneu.2019.08.22731520757 [Google Scholar] [CrossRef] [PubMed]
[9]. Biswas RS, Ganguly S, Saha ML, Saha S, Mukherjee S, Ayaz A, Gossypiboma and surgeon- Current medicolegal aspect- A reviewIndian J Surg 2012 74(4):318-22.10.1007/s12262-012-0446-323904722 [Google Scholar] [CrossRef] [PubMed]
[10]. Boussaid M, Mesrati MA, Jouirou R, Abdejlil N, Zakhama A, Chadly A, Breast Textiloma: An unending medico-legal issue about a case reportInt J Surg Case Rep 2017 34:17-19.10.1016/j.ijscr.2017.03.00428324800 [Google Scholar] [CrossRef] [PubMed]
[11]. Mercier M, Noailles T, Sali E, Carret P, Duvauferrier R, Rouvillain JL, What type of imaging work-up will help to confirm the diagnosis of gossypiboma in the limb? Review of literatureOrthop Traumatol Surg Res 2016 102:795-800.10.1016/j.otsr.2016.06.01027521180 [Google Scholar] [CrossRef] [PubMed]
[12]. El Fortia M, Bendaoud M, Sethi S, Abdominal Gossypiboma (Textilioma)The Internet Journal of Radiology 2007 9:110.5580/13b8 [Google Scholar] [CrossRef]
[13]. Arora RK, Johal KS, Gossypiboma in thigh- A case reportJ Orthop Case Rep 2014 4(3):22-24. [Google Scholar]