The United Nation country members have pledged to put universal health coverage as a central policy for health systems on the agenda to achieve the goals of sustainable development by 2030 [1-3]. Countries need progress to strengthen their health systems and improve the level and distribution of health in at least three dimensions, including expanding population coverage, costs, and services package. However, because of limited resources, policymakers inevitably have to prioritise among demographic groups and health care services provided to them, making them face ethical challenges in the decision-making of resource allocation [4].
On the other hand, some typical ways of defining and approaching universal coverage require deciding on procedures that may not be ethically justifiable. Policymakers need to account for the ethical dimensions of universal coverage policy-making to address the ethical challenges and to differentiate between fair and unfair ways in moving towards universal coverage [5].
Policy-making decisions in health-related areas are complex and value-driven. Given that the field of medical ethics focuses on ethical issues in the clinical background, in recent years, health policy-making ethics has been postulated as a new field of study that analyses the moral problems related to population and policymaking of health system’s macro issues. Alongside this, it has become more common and desirable to use ethical frameworks and principles needed for policy-making, especially in the context of resource allocation [6-8].
An inquiry into the ethical dimensions of universal health coverage policy-making is also considered as a study in the field of health policy-making ethics. Despite the fact that there is still no significant research on health policy-making ethics, the current systematic review has been conducted by examining the recommendations of international organisations, national experiences, and findings of studies. The study examines the role and application of ethics in policy-making of universal health coverage and identifies the principles and criteria of ethical frameworks to help develop a ground to study health policy-making ethics and to present clear guidance policymakers to use for universal health coverage. It provides a model for other countries that have not yet created a clear ethical framework for policy-making on universal health coverage in their health system to act based on the experiences of other countries and the recommendations made in studies in line with their local conditions.
Materials and Methods
This systematic review used PRISMA guideline and searched the Scopus and PubMed databases for papers published from January 2010 to March 2018. The year 2010 was chosen as it was the year when the World Health Organisation (WHO) published and delivered the framework of universal health coverage to countries, although countries may have taken measures for universal coverage policies in the form of insurance systems or increased state protection. Nevertheless, the basis for inclusion in this study was the history of publishing the experiences of countries in this regard.
Studies included in which: 1) the ethical dimensions of the universal health coverage policy-making were studied. Therefore, if some sources addressed the effects of universal coverage policy-making on ethical values or principles, they were not included; 2) Studies that have focused on the dimensions of policy-making ethics on universal health coverage at macro level; therefore, those studies were not addressed that merely considered the details of universal coverage, including the covered population, coverage of costs, and development of a package of covered services, and ethical challenges and issues; 3) The study, while referring to the role of ethics in policy-making on health universal coverage, has delivered the ethical framework containing the ethical principles or criteria used in policy-making. Therefore, those cases that have merely referred to delivering the ethical challenges and issues and have not provided a framework were excluded; 4) In terms of study type, the recommendations of international organisations, national experiences, or the results of original research studies, reviews or commentaries that have been published in peer-reviewed journals with English language were included. State and organisational reports, books or chapters from books, abstract of conference articles, proceedings, theses, editorials, letters, and prints were not included. For searches in databases, the following search strategies were used:
Using the Medical Subject Headings (MeSH), we searched “Ethics”, “Morals” and “Universal Health Care" and for searches in database, the following search strategies were used. TITLE-ABS-KEY (“ethics” or “ethical framework” OR “principle” OR “ethical basis” OR “moral *” OR “fair*” OR equity) AND TITLE-ABS-KEY (“universal health coverage “OR” UHC “OR” universal coverage “OR” universal health care “OR” universal access”).
The databases reviewed in this study include PubMed and Scopus. The extracted articles were managed using EndNote 9 software from the beginning to the end of the systematic review. The initial articles were reviewed based on the title and abstract. After removing duplicates, if the articled fitted into the criteria of the study, their full texts were examined, and selected papers were identified.
Certain forms were designed to extract the data of the selected articles. After reading the full text of the articles, a summary of their details were recorded in tables. Moreover, the forms were modified and finalised during the process. The data were analysed using the thematic analysis method and categorised into two groups according to the data extraction forms. The first group was related to articles that were the result of a research study, authors’ opinions, and recommendations from International Organisations; the second group concerned with articles that reflected the experiences of different countries in terms of the ethical dimensions of universal coverage policies. The extracted data of both groups were classified into three themes, including the role of ethics in universal health, ethical principles, and ethical criteria.
Results
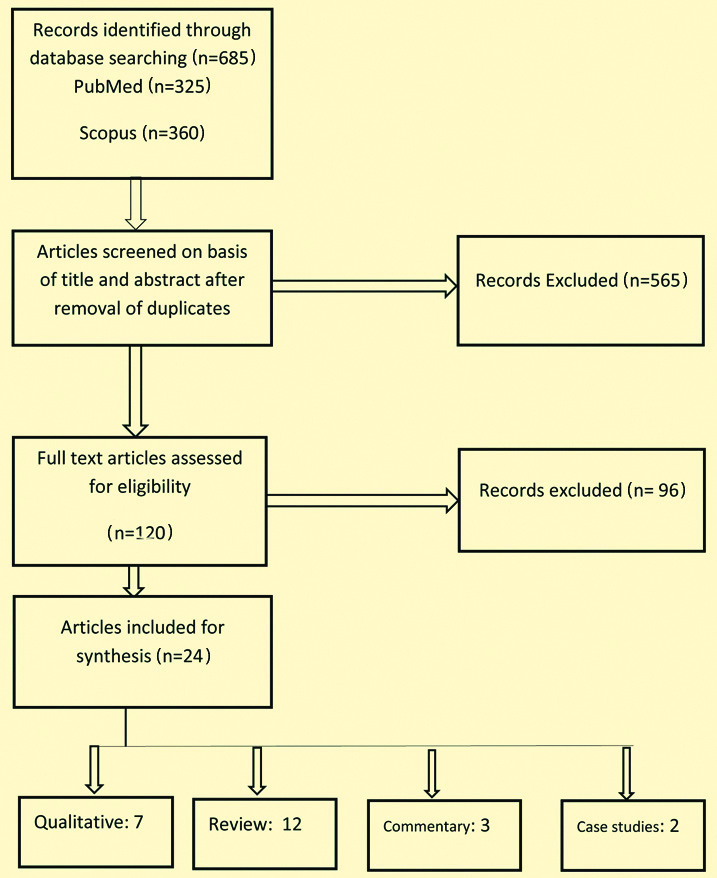
In order to identify the ethical frameworks introduced in the policy-making of universal health coverage, as outlined in [Table/Fig-1], a systematic search was conducted in the PubMed database, yielding 325 articles, and in Scopus, yielding 360 articles. After the duplicates were removed, the articles were studied based on the title and abstract, among which 120 articles were selected as relevant. The articles with accessible full texts were studied, of which 24 were selected in line with the inclusion and exclusion criteria, including seven qualitative studies, 12 review studies, three commentary studies, and two case studies. These articles were categorised into two groups. The first group expresses the ethical frameworks introduced in the studies. [Table/Fig-1] presents the characteristics of these studies and the dimensions of their ethical framework. The second group is concerned with the experiences of countries in applying the ethical principles and criteria in the universal coverage policy-making as outlined in [Table/Fig-2] [9-32].
Flow diagram of study selection.
Ethical principles and criteria in the universal coverage policy-making [9-32].
| Voorhoeve A et al., [9,10] | Norheim OA [11] | Reis AA [12] | Allotey P et al., [13] | Sridhar D et al., [14] | Fattore G and Tediosi F [15] | Rodney AM and Hill PS [16] | Butiler SA [17] |
|---|
| Type of article | Precise | Case studies | Commentary | Commentary | Background paper | Review | Review | Narrative review | Philosophical |
|---|
| Ethical principle | - Fairness in coverage and service provision- Benefit maximisation- Fair contribution- Accountability | - Promote health maximisation- Fair distribution- Protection against poverty | - Solidarity- good governance (effective governance)- fairness, equity, and benefit maximisation | - Vulnerability- good governance | - minimum core obligation- progressive realisation - cost-effectiveness- shared responsibility- participatory decision making- prioritising vulnerable or marginalised groups | - equity- solidarity | -equity | - solidarity |
| Ethicalcriteria | -Coverage and use should be based on need; extra weight should be given to the needs of the worse off.-One aim should be to generate the greatest sum of health-related well-being in a given population-Contributions should be based on ability to pay and not need-Cost-effectiveness-improving the lot of the worse off-Financial risk protection.-First expand coverage for high-priority services to everyone-Ensure that disadvantaged groups are not left behind. | -promote health maximisation- fair distribution Protection against poverty | -Solidarity-good governance (effective governance)-fairness, equity, and benefit maximisation | | -minimum core obligation-progressive realisation-cost-effectiveness-shared responsibility-participatory decision making-prioritising vulnerable or marginalised groups | -equity-solidarity | | |
| Country of study | Scandinavian countries (Sweden, Denmark, Norway) | Thailand | Africa |
|---|
| Author | Hofmann B [18] | Tangcharoensathien V et al., [19,20] | Tantivess S et al., [21] | Youngkong S et al., [22] | Harris B et al., [23] | Doherty JE et al., [24] | Yamin AE and Maleche A [25] |
|---|
| Type of article | Review | Original | Commentary | Original | Original | Original | Qualitative study | Review |
|---|
| Ethical principle | Sweden | Denmark | Norway | - equity- efficiency | | | - Fairness- Rational- Transparent | - Social solidarity | - fairness | - human rights principles |
| - human dignity- needs- solidarity- cost-effectiveness | - equality- solidarity- security and safety- autonomy | - severity of disease- equal access- solidarity with vulnerable- individual rights to access to health |
| Ethical criteria | | The values of social and social justice, the cost of effectiveness, democracy and customer influence. | Potential effects, efficiency, and effectiveness in Norway have been put in place as criteria to measure the extent of the patient’s needs. | - cost-effectiveness- equity | - cost-effectiveness- budget impact- Priority to the worse-off | - cost-effectiveness- budget impacts- equity- solidarity | - Size of the population affected by disease- Severity of disease- Effectiveness of health intervention- Variation in practice- Economic impact on household expenditure- Equity/ethical and social implication | - Vertical equity- Horizontal equity | | - Cost-effectiveness- Financial risk protection- Severe disease- Disadvantaged population |
| Country of study | United states | Germany | Japanese | Latin America | Pakistan | Burkina Faso |
|---|
| Author | Macnaughton G et al., [26] | Buss R et al., [27] | Shibuya K et al., [28] | Atun R et al., [29] | Cubillos L et al., [30] | Tasneem B et al., [31] | Agier I et al., [32] |
|---|
| Type of article | Case study | Review | Review | Review | Review | Review | Original |
|---|
| Ethical principle | human right principles:- Universality- Equity- Accountability- Transparency participation | - solidarity- self-governance | - solidarity- egalitarian- financial sustainability- fairness- equity | - solidarity- equity- collective action | - right based approach | - fairness- accountability | - sustainability- solidarity |
Role of Ethics in Universal Health Coverage Policy-Making
As shown in [Table/Fig-3], ethics can be contributory in four fields of universal health coverage policy-making, including its roles as the driving force, guidance for decision-making, provider of public acceptance, and a guarantee for justice administration, as explained below:
The Role of Ethics in universal health coverage policy-making.
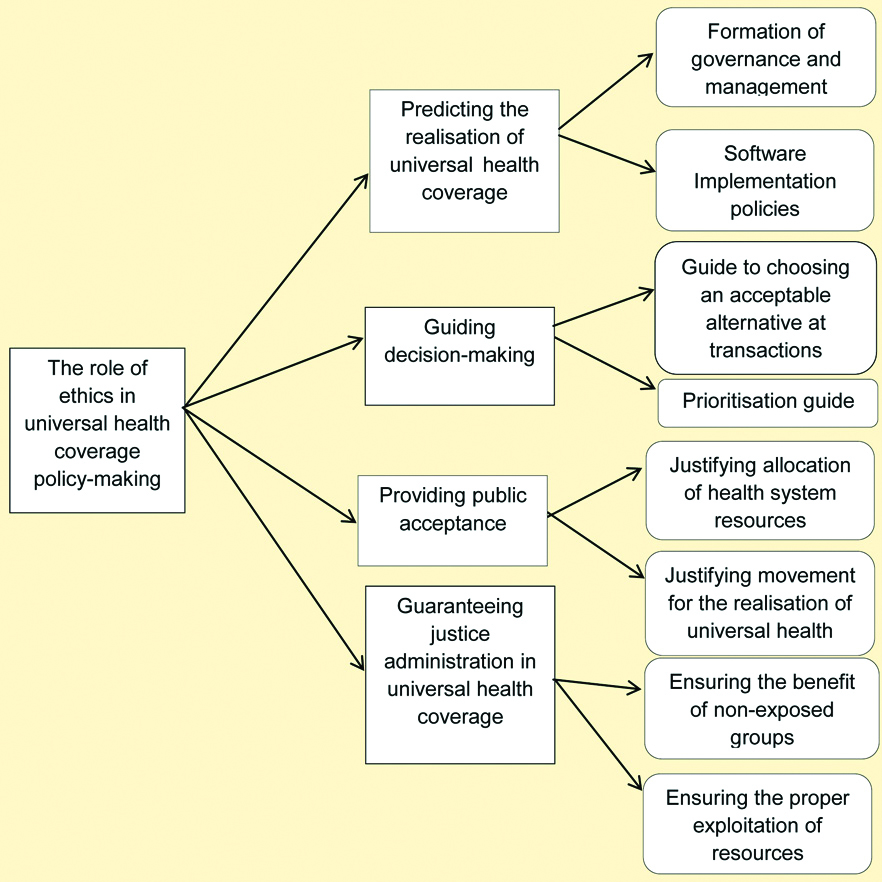
- Predicting the Realisation of Universal Health Coverage
According to the results of the analysis, ethics as a driving force stimulates the achievement of universal coverage goals to strengthen health systems and promote the level and distribution of health and clinical services among the population [9]. Governance and health management models are not neutral to values. In fact, principles and values shape governance and management in order to meet the goals of universal health coverage. On the other hand, ethical values and norms act as the software for implementing the policies that are against the structure, organisation, and technology, which act as the hardware [15].
- Guiding Decisions
Through delivering some principles [25,26], ethics provides guidance [21] and a basis [12] for policymakers when deciding and evaluating reforms and issues of universal health coverage, such as the formulation of a services package [21]. Especially when policymakers are confronted with challenging situations or limited resources, they are determined to prioritise things. Hence, decisions may be made that may improve progress towards the ultimate goal of ensuring that everyone has access to the required health services [9].
Ethical principles help policymakers in their recognition of the acceptability of a universal health coverage tool and guide them to choose between the three dimensions of population, coverage, and cost for allocating the limited resources [9,11,20,21]. It also provides guidance for surveys that may be encountered by policymakers in each dimension of the health universal coverage.
Considering the increase in health costs and the need for careful monitoring of health care and the importance of health technologies development, it has become possible to prioritise work at a general level. Meanwhile, the ethical priority is considered as one of the priority approaches that are possible through introducing ethical principles and values. Ethics plays a central role in deciding which service should be developed first, who should be covered first, and how to move from pay to prepayment [9,18,22].
- Providing Public Acceptance
Another role for ethics in the universal health coverage policy-making process is its ability to justify the allocation of health resources by delivering some criteria for explicit and clear quotas [21]. Also, by explaining and justifying the move to achieve universal health coverage [12], it facilitates public acceptance of decisions about health services coverage [22].
- Guaranteeing Justice Administration in Universal Health Coverage
As a type of vital infrastructure, ethics ensures that justice is administered in the exploitation of health services by all community members [13,19]. By presenting ethical principles, it helps countries to perform reasonably and accurately on the limited resources of the health system through the creation of a proper resource-prioritising process to achieve sustainable universal coverage [24] Moreover, establishing a comprehensive health coverage based on ethics enables policymakers to overcome social inequalities [29] and prioritise addressing the problems of disadvantaged populations and individuals suffering from poverty due to lack of government’s commitment and limited resources due to health costs [21,31]. Failure to comply with ethical principles may deprive vulnerable groups of adequate or quality healthcare services. Therefore, paying attention to these principles while moving towards universal coverage targets were emphasised until they benefit health services as other advantaged people [16].
The Ethical Framework for Universal Health Coverage Policy-making
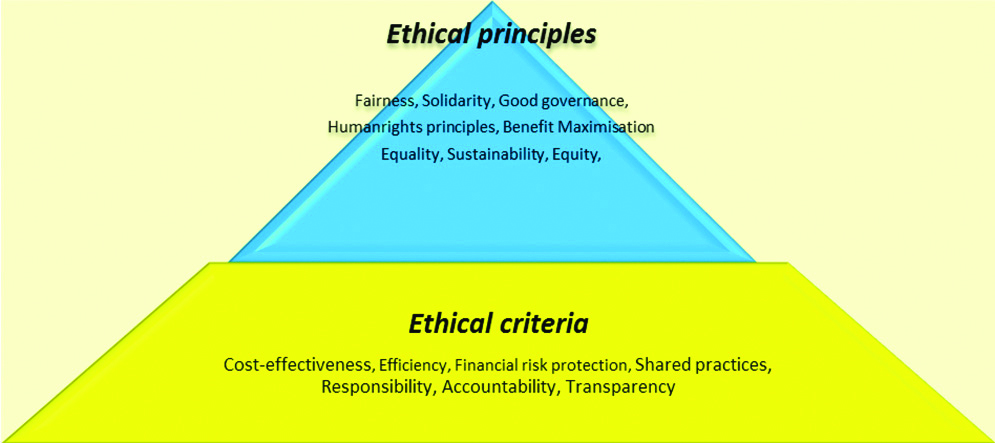
Based on the findings, as presented in [Table/Fig-4], the dimensions of the ethical framework presented in the studies comprise the two levels of ethical principles and ethical criteria. Ethical principles are more general; ethical criteria are in line with the principles, yet in more specific and applied terms. Some studies have covered the principles, while others have only provided the criteria. These will be discussed below.
The Ethical Framework for universal health coverage policy-making.
- Principles of Fairness, Justice, Equity, and Equality
When policy-makers are confronted with limited resources, the ethical principles of fairness, justice, equality, and equity can help provide an acceptable decision-making and prioritisation path, through which one can ensure fair universal health coverage [33]. Also, when faced with threats, the policymakers can build on the principle of fairness in policy-making, as fairness leads to the overall distribution of interests and burdens in the community and plays a central role in universal coverage [5].
Fairness can be expressed in terms of resource allocation policies, service coverage, provision of services, and financial participation [9,11]. Different groupings are also presented in terms of justice. Some have put forward horizontal justice, and some have mentioned vertical justice [23], while some have considered the principle of social and geographical justice [18]. Some countries, such as Japan, have built on both principles of justice and fairness and have emphasised the egalitarian principle to benefit the principle of equality [28]. On the other hand, countries, such as Thailand, have just stated the principle of justice, and Pakistan has expressed the principle of fairness [31]. In Norway, equality is mentioned as for access to services [18]. As outlined in [Table/Fig-2], all studies have mentioned fairness and equity as principles. In the case of justice, however, some studies have introduced it as a principle, while others have considered it to be a criterion.
- The Principle of Benefit Maximisation and the Criteria of Efficiency and Cost-effectiveness
Regarding the fact that policymakers are obliged to prioritise resource allocation at the macro, mid, and micro levels of the health system when moving towards the realisation of the universal health coverage, it would be highly controversial to balance between the criteria of benefit maximisation, efficiency, and cost-effectiveness. In countries such as Germany and the United States, the cost-effectiveness criterion has not been accepted by some ethical experts, while the criterion is used in some African countries and Thailand [11,21,25].
Maximising the benefits analyses the short-term and long-term effects of resource allocation to maximise the benefits and obtain the highest possible level of health for the population [9,11,20,21]. The efficiency criterion is used to minimise the consumed resources. Following both of these dimensions, policymakers use the cost-effectiveness criterion to select priority services for coverage [9,34].
- The Principle of Solidarity
The principle of solidarity means joint actions that represent collective commitment to bear the financial, social, and emotional costs to help others. This principle, as an infrastructure concept, can help policymakers to explain and justify moving towards universal coverage and provides the basis for designing redistribution and accumulation mechanisms in the funds [12]. Despite the emphasis of most countries on the principle of solidarity, in Norway, the principle of solidarity with vulnerable groups has been mentioned [18], and in Southern Africa, the principle of social solidarity has been highlighted [23].
- Sustainability Principle
This principle focuses on the way resources are exploited so that they can be saved for future use, and therefore, policymakers should use resources for universal coverage purposes to improve sustainability [35].
A consideration of this principle makes the health system responsive to the needs of the covered population against the threats posed by demographic, economic, and political changes. That is why Burkina Faso and Japan have called for this principle for policy-making concerning universal coverage reforms in the country. Of course, in Japan, financial sustainability has been highlighted [28,32].
- The Principle of Good Governance
The principle of good governance is considered as the foundation and basis for moving towards universal health coverage across the country, which is the basis for policymakers’ decision-making. This principle, sometimes referred to as effective governance, refers to a set of processes that distribute the response among actors of the health system in an optimal way [12,13]. Among the studied countries, Germany refers to the Bismarck Insurance on the Principle of Self-Governance, which supervises the governance of a joint system of the provider and payer of health services [27].
- The Criterion of Financial Risk Protection
This criterion is used to protect the non-prosperous, vulnerable, on the sideline groups to ensure that they are considered by policy-makers when moving towards universal health coverage targets [14,25]. According to this criterion, policymakers should account for the economic effects of their decisions on household expenses and protect the vulnerable groups against poverty [11,22].
The outcome of this criterion is the contribution in payment based on one’s strength, not one’s need; in that case, financial contribution from healthy people can be used to help vulnerable people of poor health conditions. Alongside this, coverage policy-making and service benefits should be based on need whereby further weight should be given to the more disadvantaged people [9,32].
- The Principle of Human Rights
Paying attention to the principles of human rights stems from a legal approach to universal health coverage policy-making [30]. It involves learning, justice, accountability, transparency, and participation. These principles, based on an individual’s right for access to health services, oblige policymakers to make decisions in a way that human rights can be preserved [12,18]. Some countries covered in this study, such as the United States, have considered all principles of human rights, whereas Pakistan has emphasised the principle of accountability, Thailand has highlighted the principle of transparency, and Latin American countries have emphasised the principle of partnership [22,26,29,31].
Discussion
Given the importance of universal health coverage as an international commitment, attention to its various dimensions, including the ethical dimension, is essential for policymakers. Most studies in this area have focused on the policies of countries on the development of coverage, population, and services, and the ethical approach has not been addressed [1]. While there are reviews on ethics in the field of general health or health leadership, based on our knowledge, however, this is the first systematic review performed on the ethical dimensions of health policy-making with a focus on universal health coverage [18,29].
Some reviews have also considered the ethical implications of universal coverage [33,34]. Meanwhile, it is necessary to consider both ethical policy-making and policy-making ethics. Researchers have less covered this dimension. This study attempts to focus on this approach.
Regarding the role of policy-making ethics on universal health coverage, findings suggested that ethics plays a role as a guide when designing and choosing policies as well as being a driving force behind the initiation of the policy-making process. In implementing the adopted policies, ethics paves the ground for public acceptance, thereby making the implementation of the policies more appropriate and guaranteeing the policymakers’ aims of justice administration in universal health coverage.
Health policy-making ethics can be considered as a trend in applied The numbers presented besides the terms represent the frequency of studies expressing that principle or criterion. ethics. Its application is based on ethical frameworks comprising a set of ethical principles and criteria. As illustrated in [Table/Fig-5], most studies have emphasised the use of the principles of human rights, solidarity, justice, fairness, cost-effectiveness, and financial risk protection in the policy-making of universal health coverage.
Ethical Principles and criteria for universal health coverage policy-making.
The numbers presented besides the terms represent the frequency of studies expressing that principle or criterion.
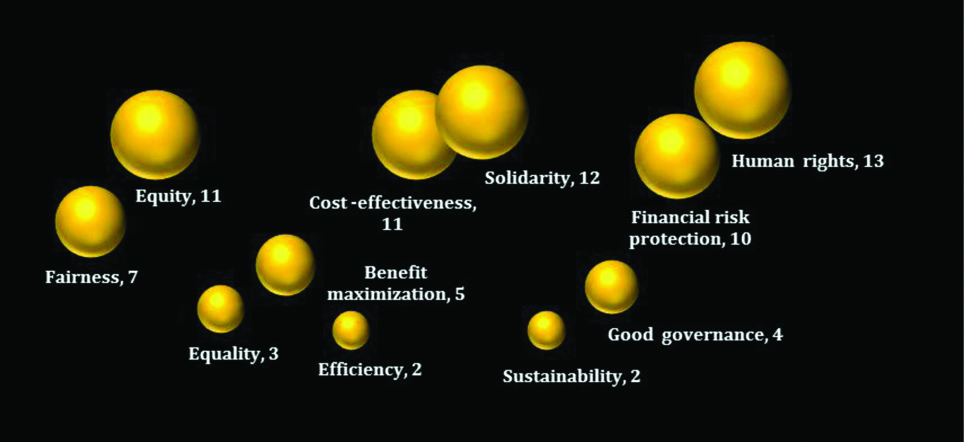
The findings of the study indicated the difference in ethical frameworks introduced by different countries. The function of these principles is to explain and justify the movement towards universal coverage. Therefore, varying cultural and social conditions, the political orientation of countries, and the type of local values underlie the differences in the principles and criteria presented.
Limitation(s)
- The recent emergence of the scientific field of ethics in health policy-making and the lack of research studies in this field.
- The difficulties associated with the interdisciplinary nature of ethics and policy-making as related to universal health coverage.
- Lack of research studies that have examined the ethical dimensions of policy-making for universal health coverage.
- Ethical principles and criteria were examined at the general level of policy-making for universal health coverage, and they were not explored in detail at the level of population, the service package design, and the cost coverage.
- Some definitions of ethical principles and criteria are provided on some of which there is not unanimous agreement among researchers.
- The unexpressed and unclear principles of normative ethics and ethical principles and criteria in studies.
- No precise and comprehensive description is presented in the literature as for the context of the conflicts between ethical principles and criteria in one framework or as to the way to prioritise them in the policymaking process.
Conclusion(s)
In moving towards the realisation of universal health coverage by 2030, countries should consider both, the experience of other countries and build on research to formulate a moral framework that can guide the principles and criteria of their ethical frameworks. A clear ethical framework will make policy-makers less error-prone and facilitate more precise policy-making. As a result, ethics can play its true role and function in universal health coverage policy-making and help in solving the ethical challenges and the problems with which policymakers confront. Of course, further research would be required on the ethical dimensions of policy-making for population size, service package design, and cost coverage.
Directing attention to the ethical dimensions of universal health coverage policy-making ensures that ethical values and principles are realised, while maintaining transparency in decision-makers holds authorities accountable for providing universal health. Yet, it should not lead to ignoring other dimensions of universal health coverage, such as political commitment, provision of the required finance, the regulatory rules, and its implementation. Ethical criteria and criteria should be regarded as one of the dimensions of the policymaker’s guide and not as the sole contributor. Policymakers need to account for other areas such as political values in their community. Of course, how to balance and establish the interaction between ethical principles and political principles also requires separate scrutiny, which is recommended to be explored in future.
Given the emergence of the scientific field of health ethics policy-making, the ethical principles and criteria identified in this study can be considered in other fields of health policy-making. Future research may assess the generalisability of these principles so that, as in the principles of medical ethics, some principles may gradually emerge in health policy-making on which scholars and policymakers agree in terms of title, concept, and application.