Class III anomalies are among the problems that are more difficult to treat in orthodontic malocclusions [1]. In the current day and age, patients with Class III malocclusion are more concious of the visible effects on the facial appearance [2,3], due to their unfavourable effects on the psychosocial status of the patients. Components of Class III malocclusions are mandibular prognathism, maxillary retrognathism, or a combination of these two conditions [1].
Orthognathic surgery or camouflage treatment in adult patients and orthopedic treatments are preferred in young adolescents during growth and developmental period. Maxillary protraction treatment, which is frequently used in the treatment of skeletal Class III malocclusions related to maxillary retrognathism, also has undesirable effects [4].
In tooth-assisted maxillary protraction applications, undesirable dental effects develop as a consequence of protruding of the incisors along with the skeletal movement of the maxilla and increasing the vertical direction parameters as a result of extrusion of the maxillary molars. Due to the extrusion of the molar teeth, the clockwise rotation in the mandible, the counter-clockwise rotation in the maxilla causes an increase in the measurements in the vertical dimension of the patient [5,6]. Especially in patients with a high-angle growth pattern, if the need for maxillary protrusion is increased compared to patients with normal growth patterns, such maxillary protraction applications may reduce overbite and increase the vertical dimensional measurements [7].
Various methods are applied in Class III patients with high-angle growth pattern in order not to increase vertical dimension more. In the literature, it is recommended to use Nanda-type [8] and Grummons-type [9] face masks in order not to increase the vertical direction dimensions for this type of patient. Also, skeletal anchorage methods [10,11], which enable us to apply force over the center of the resistance, are also used successfully.
This study aimed to assess the craniofacial and soft tissue effects of the maxillary protraction with skeletal anchorage along with Petit-type facemask when used for the treatment of high-angle Class III young adolescent patients due to maxillary retrognathia.
Materials and Methods
A retrospective study of patients with high angle growth pattern Class III malocclusions treated with maxillary protraction skeletal anchorage between June 2018 and June 2019 years in Suleyman Demirel University, Orthodontic Department of Dentistry. Ethical approval of this retrospective study was obtained from Clinical Research Ethics Committee of Süleyman Demirel University Faculty of Medicine (Ethics approval decision number: 28.05.2019/190) and parents of the patients had signed an informed consent form allowing the authors to use their data (images, cephalograms, etc.,) for scientific purposes. The sample size was calculated based on a significance level of 0.05 and a power of 80%. It was determined that 15 patients were required by performing power analysis.
One of the two authors regularly scanned the archives to determine the study samples according to inclusion criteria as follows: [1] skeletal and dental Class III malocclusion due to maxillary retrognathia (SNA <80° and ANB <0°); [2] high-angle growth pattern (SN-GoGn >38°); [3] treated using face mask with mini-plate anchorage inserted in the lateral nasal wall; [4] no extraction except third molars; [5] no systemic disease and congenital anomalies.
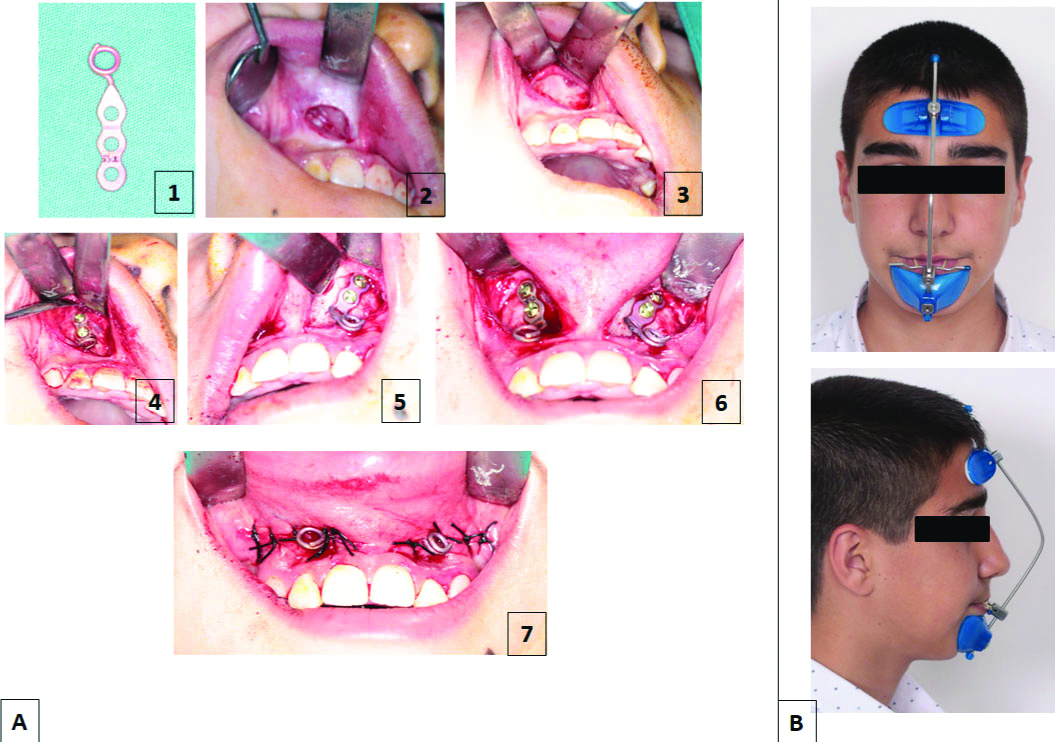
A total of 23 patients selected from the archives were evaluated in terms of the application of face mask and vertical direction measurements. 15 patients with inclusion criteria were identified. Six patients were excluded because of different maxillary protraction, and 2 patients were excluded from the study due to inadequate records. According to the cervical vertebral maturation method, all patients were in the prepubertal and pubertal stage of skeletal maturity (Stage 1-4). This study consisted of 15 patients (7 females and 8 males; mean age, 11.96±1.03 years) treated using face mask with mini-plate anchorage inserted in below the Apertura piriformis region. Maxillary protraction was applied by placing two I shaped titanium mini-plates (Stryker, Leibinger, GmbH and Co KG, Freiburg, Germany). A mucoperiosteal flap was made and elevated from maxillary lateral incisor and canines to the lateral nasal wall on both sides under local anesthesia. At this stage, more attention has been paid to avoid harming canine teeth. Titanium mini-plates were modified according to the Apertura piriformis anatomic structures and then placed with 3 monocortical mini-screws (diameter, 1.5 mm; length, 7 mm). After 1 week for soft-tissue healing, protraction forces were applied with 5/16 medium pull elastics immediately. Force levels measured by a dynamometer (Correx 0-250 g, Bern, Switzerland).
Petit-type face-mask was used with an approximately 500 g bilateral, same force applied with an antero-inferior force vector of approximately 30° to the occlusal plane from the hooks of the mini-plates. Patients used a total of 6 months’ Petit-type face mask for the first three months throughout the day (approximately, 18-20 hours in a day), the next 3 months for 12 hours a day [Table/Fig-1,2 and 3]. The duration of treatment of the patients is 7 months on average (0.61±0.21 years).
Mini-plates and surgical placement of mini-plates: a- 1) I shaped titanium; 2, 3) a mucoperiosteal flap elevated; 4) mini-plate placed; 5) mini-plate secured with mini-screws; 6) 2 mini-plates placed; 7) sutures placed along with hooks for elastics and B) Petit type Face-Mask used in the study.
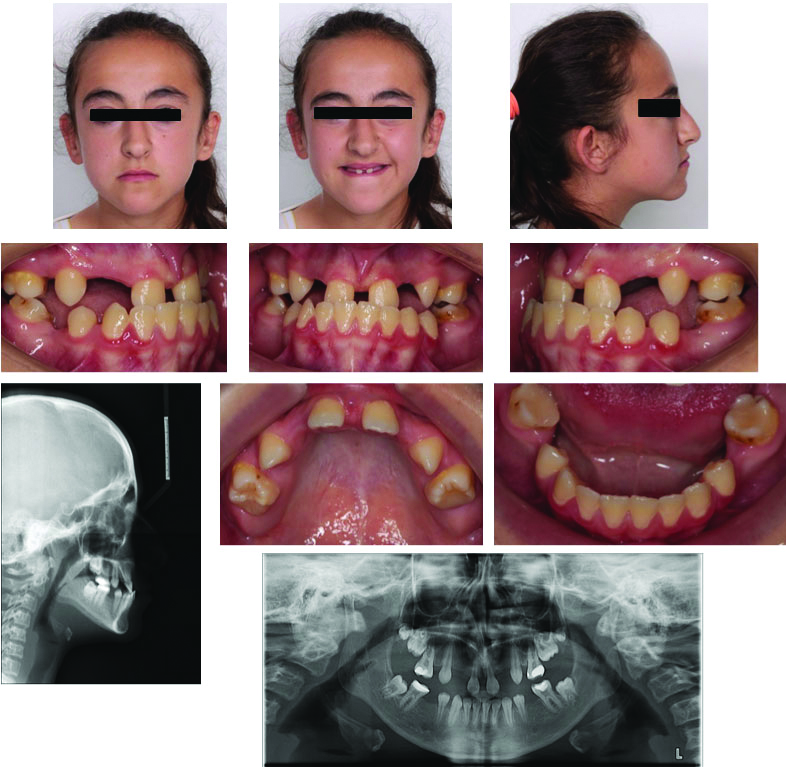
Pre-treatment intraoral, extraoral photos lateral cephalogram and orthopantogram radiographs in Class III malocclusion patient with maxillary retrognathia, negative overjet.
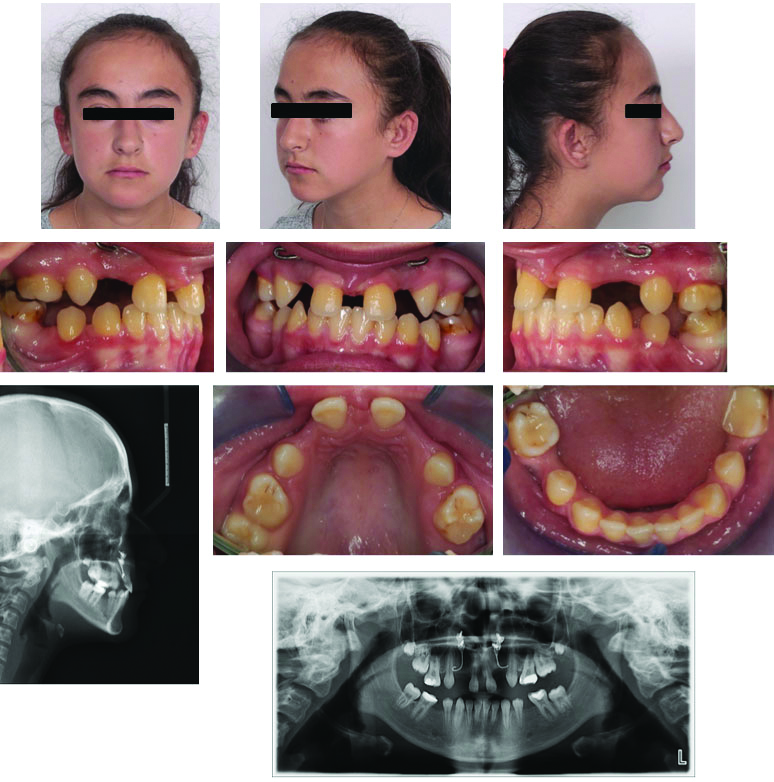
Post-protraction intraoral, extraoral photos lateral cephalogram and orthopantogram radiographs in Class III malocclusion patient with improved facial profile and dental malocclusion with positive overjet.
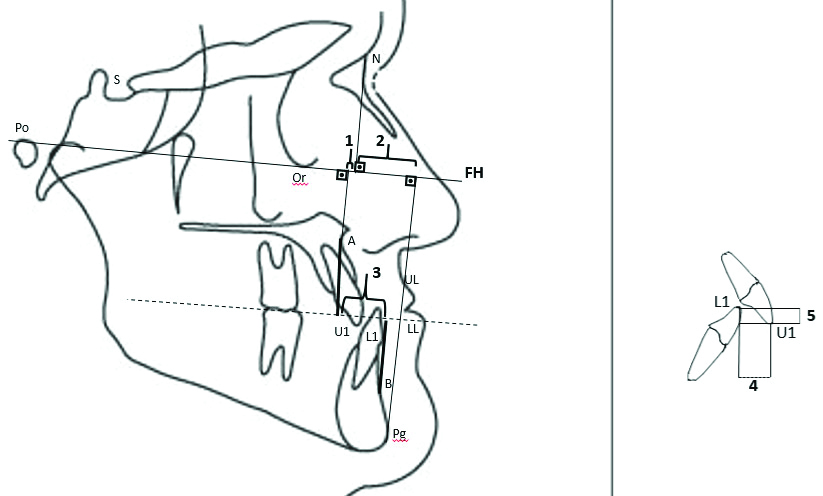
Cephalograms were taken (Planmeca Promax, Planmeca Co., Ltd., Helsinki, Finland) at the beginning (T1) and after 6 months of maxillary protraction therapy (T2). An imaginary line which passes via tuberculum sella and wing point (junction of the contour of the ala major with jugum sphenoidale) was used as the Horizontal Reference Line (HRL) and a line perpendicular through tuberculum sella as a Vertical Reference Line (VRL) [Table/Fig-4].
Reference planes used in the study and linear measurements according to reference planes: (1) A-VRL; (2) UL-VRL; (3) L1-VRL; (4) LL-VRL; (5) U1-VRL; (6) B-VRL; (7) Pg’-VRL; (8) Pg-VRL.
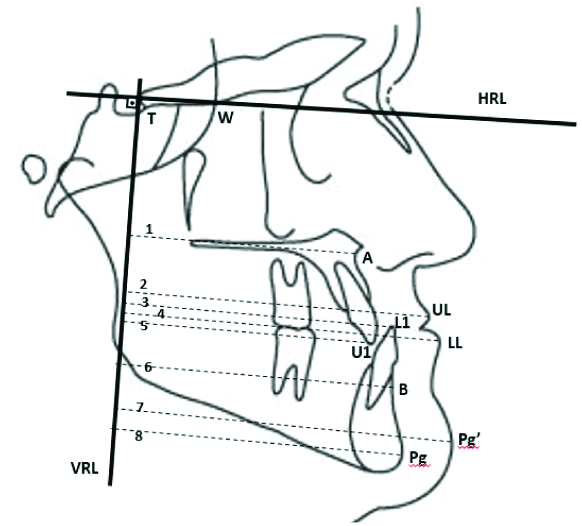
After calibration, all radiographs were traced blindly by a single researcher [Table/Fig-4,5,6 and 7]. (Steiner, Tweed, Wits and McNamara Analysis was used, measurements were also made based on the reference planes) were made to evaluate and compare the craniofacial and soft tissue effects of the maxillary protraction using Dolphin Imaging Version 11.8.06.24 Premium software (Dolphin Imaging and Management Solutions, Chatsworth Calif).
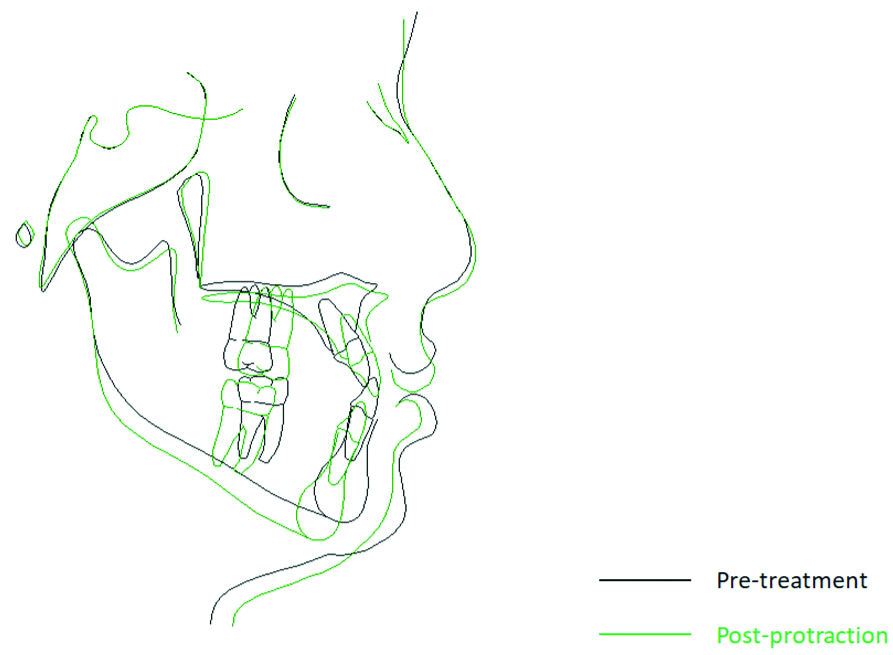
Superimpositions of cephalometric tracings (Cranial Base (Sella/Nasion) for overall change during treatment).
Cephalometric angular measurements: (1) SNA°; (2) SNB°; (3) ANB°; (4) SN-GoGn°; (5) U1-PP°; (6) IMPA°; (7) SN-PP°
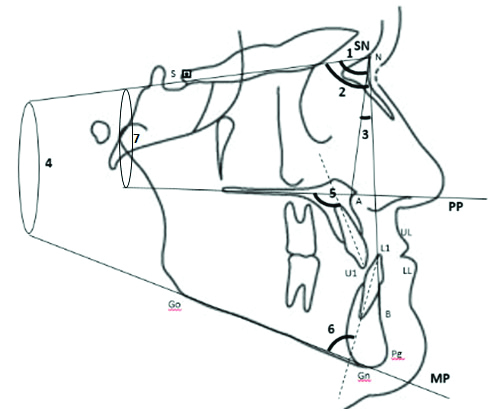
Cephalometric linear measurements: (1) NPerp-A (mm); (2) NPerp-Pg (mm); (3) Wits (mm); (4) Overjet (mm); (5) Overbite (mm)
Statistical Analysis
All statistical analyses were performed using the SPSS software package program (SPSS for Win, ver 21.0; SPSS Inc., Chicago, Ill) for all tests. Eight radiographs were selected randomly 15 days after the first evaluation, and all measurements were performed again by the same researcher. The method error was detected using the Houston test [12]. It was observed that the coefficient of reliability for all of our measurements was high (highest value SNA° 0.998, A-VRL 0.975; the lowest value SNB° 0.876).
The parametric tests were used for statistical evaluation since the Shapiro-Wilks test showed normally distributed variables. The paired t-test was applied to evaluate differences between pre-(T1) and post-(T2) treatment variables. The significance level was set at p<0.05.
Results
The descriptive data, including chronological age, the gender distribution is shown in [Table/Fig-8]. The mean chronological age was 11.96±1.03 years. The mean duration of treatment was 0.61±0.21 years. The initial cephalometric values of the patients are shown in [Table/Fig-8]. The patients had skeletal Class III malocclusion due to the maxillary retrognathism, high-angle growth pattern, proclined upper incisors, and retroclined lower incisors. Changes occurred during maxillary protraction; the statistical comparison of these changes is shown in [Table/Fig-8]. The total superimposition of cephalometric tracings of one of the patients in the present study is shown in [Table/Fig-5].
Demographic datas, ınitial cephalometric values for study subjects and statistical evaluations of changes obtained in maxillary protraction.
| Parameters | Norm values | Pre treatment | Post protraction | Mean changes | | |
|---|
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | p |
|---|
| Demographic data | | | | | | |
| Chronological age (Years) | | 11.96±1.03 | 12.46±0.83 | 0.50±0.93 | | - |
| Gender distribution (Female/Male) | | 7 Female/8 Male | | | - |
| Maxillary measurements | SNA (°) | 82±2 | 76.56±0.79 | 80.04±0.61 | 3.48±0.42 | 0.000 | *** |
| N Perp A (mm) | 0±2 | -4.66±2.74 | -0.82±2.63 | 3.84±0.64 | 0.000 | *** |
| CoA (mm) | 85±5 | 80.19±0.74 | 84.95±0.69 | 4.76±0.41 | 0.000 | *** |
| A-VRL (mm) | - | 45.52±3.16 | 49.46±2.52 | 3.94±0.81 | 0.000 | *** |
| Mandibular measurements | SNB (°) | 80±2 | 78.78±0.82 | 78.28±0.93 | -0.50±0.30 | 0.132 | NS |
| N Perp Pg (mm) | -4±5 | 6.10±0.49 | 5.07±0.33 | -1.03±0.50 | 0.027 | * |
| CoGn (mm) | 112±5 | 116.57±0.46 | 117.31±0.29 | 0.74±0.21 | 0.352 | NS |
| B-VRL (mm) | - | 44.84±2.79 | 43.99±2.71 | -0.85±0.28 | 0.487 | NS |
| Pog-VRL (mm) | - | 44.53±3.56 | 43.02±3.71 | -1.51±0.50 | 0.698 | NS |
| Vertical measurements | SN-GoGn (°) | 32±6 | 38.98±1.01 | 39.23±1.03 | 0.25±0.21 | 0.741 | NS |
| PP-MP (°) | 28±3 | 32.8±2.5 | 33.04±2.53 | 0.24±0.14 | 09.258 | NS |
| SN-PP (°) | 8±3 | 11.68±2.43 | 11.48±2.44 | -0.19±1.33 | 0.018 | * |
| SN-Occ (°) | 16±4 | 18.71±1.84 | 18.88±1.79 | 0.17±0.12 | 0.016 | * |
| Maxillo- mandibular measurements | ANB (°) | 2±2 | -2.08±0.69 | 1.76±0.85 | 3.85±0.46 | 0.000 | *** |
| Wits (mm) | 1±1 | -4.36±1.45 | 0.51±0.88 | 4.88±0.70 | 0.000 | *** |
| Dentoalveolar measurements | U1-PP (°) | 110±5 | 129.44±4.22 | 126.31±4.41 | -3.12±0.42 | 0.007 | ** |
| IMPA (°) | 90±5 | 87.16±2.62 | 86.70±2.70 | -0.46±0.24 | 0.249 | NS |
| U1-VRL (mm) | - | 118.06±5.02 | 116.46±4.70 | -1.60±0.91 | 0.024 | * |
| L1-VRL (mm) | - | 60.36±1.13 | 59.11±1.22 | -1.24±0.82 | 0.367 | NS |
| Overjet (mm) | 2±2 | -1.44±0.99 | 2.12±1.07 | 3.56±1.01 | 0.000 | *** |
| Overbite (mm) | 2±2 | 0.76±1.49 | 0.41±1.45 | -0.35±0.66 | 0.489 | NS |
| Soft tissue measurements | Nasolabial angle | 105±5 | 112.34±3,78 | 104.25±4,21 | -8.09±0.99 | 0.000 | *** |
| UL-S (mm) | 0±2 | -2.16±0.31 | 0.41±0.24 | 2.57±0.43 | 0.000 | *** |
| LL-S (mm) | 0±2 | 0.98±0.34 | 0.66±0.51 | -0.32±0.44 | 0.007 | ** |
| UL-VRL (mm) | - | 61.06±4.31 | 64.20±3.91 | 3.13±0.74 | 0.000 | *** |
| LL-VRL (mm) | - | 63.20±4.61 | 62.53±4.61 | -0.66±0.48 | 0.159 | NS |
| Pog(s)-VRL (mm) | - | 61.20±4.07 | 58.93±4.31 | -2.26±1.03 | 0.365 | NS |
P: Results of paired t-test; SD: Standard deviation. *p<0.05; **p<0.01; ***p<0.001; NS: Not significant p>0.05
In this study, the skeletal class III relationships and anterior cross-bites were improved; maxillary measurements significantly increased (SNA° 3.48±0.42°; A–VRL 3.94±0.81 mm; NPerp-A 3.84±0.64 mm; p<0.001), SNB° decreased (-0.50±0.30°; p > 0.05), ANB° increased (3.85±0.46°; p<0.001) and SN-GoGn° slightly increased (0.25±0.21°; p > 0.05) which resulted in 3.94 mm forward movement (A-VRL) and 0.19 degree clockwise rotation (SN-PP) in the maxilla and 0.25 degree rotation in the mandible (SN-GoGn)(p<0.001).
In order to determine the amount of advancement of the maxilla, the vertical distance of point A to the VRL was examined, and the monthly advancement rate was determined by dividing the change after the protraction and the duration of treatment. As a result of an average of 7 months of protraction, the rate of maxillary advancement was determined as 0.53 mm per month.
The maxillary and mandibular incisors showed retroclination (-3.12±0.42 p<0.01;-0.46±0.24°; respectively). The changes in skeletal and dental parameters caused a significant increase in overjet (3.56±1.01 mm; p<0.001) and decrease overbite (-0.35±0.66 mm; p > 0.05) measurements. The upper lip moved forward (3.13±0.74 mm; p<0.001), and the lower lip (-0.66±0.48 mm; p > 0.05) and soft tissue pogonion (-2.26±1.03 mm; p>0.05) moved backward.
After obtaining at least 2 mm positive overjet of patients and completing at least 6 months of maxillary protraction, fixed orthodontic treatments were initiated for patients who were in permanent dentition, and the mini-plates remained in the mouth and continued to use face masks for retention at night. Mini-plates were removed at the end of treatment.
Discussion
For individuals with a high angle growth pattern, the growth rate of the jaw in the vertical direction is higher than in the normal growth pattern. If these individuals can not compensate for the growth in the vertical direction of the jaws, the open bite can occur [13]. If individuals with high-angle growth patterns have class III malocclusion due to maxillary retrognathism, the treatment becomes more complicated [7].
When the tooth-supported face mask used in Class III malocclusion therapy, there is an increase in the vertical direction measurements of the patients due to the extrusion of the maxillary molars and due to the clockwise rotation of the mandible [14-17]. Different methods are used for maxillary protraction in individuals with high-angle growth pattern. Grummons type [9] face mask which does not support the chin side to reduce the clockwise rotation of the mandible, Nanda-type, Grummons-type [8] face mask which has the possibility of applying force over the resistance center of the maxilla, and skeletal anchorage supported face mask which can apply force in front of the resistance center of maxilla [10,11].
Many researchers have defined the center of resistance of maxillae [18-22]. When the protraction force is applied over the center of resistance of the maxillary, the counter-clockwise rotation of the maxilla descends to a minimum and is prevented in the complications that occur in the vertical direction. Similar to this study in the literature, skeletal anchorage assisted maxillary protraction applications are available [10,11,23]. However, the difference in the current study is that there is no intraoral unit {Rapid Maxillary Expansion (RME) etc.,} within the mouth. With this application, pure skeletal protraction was made without support from the teeth. Thus, the extrusion in the posterior teeth associated with the expansion is prevented and therefore vertical measurements are minimised.
When the changes caused by the treatment were evaluated, it was found that the maxilla moves forward 3.9 mm. In similar studies Kırcelli BH and Pektas ZO detected the maxilla moves forward 4.82 mm as a result of a face-mask for 10 months, Sar C et al., moved forward 3.11 mm in 7 months, and Elnagar MH et al., 4.87 mm in 8 months [10,24,25]. As a result, an increase was observed in the maxillary measurements. The face mask showed a reduction in mandibular measurements supported by chin and improvement in maxillo-mandibular measurements. Retrusions were seen in the lower incisors due to the chin part of the face mask and in the upper incisors due to the change of the inclination of the palatal plane due to the application of force in front of the resistance center of the maxilla. Overjet has been improved due to both maxillary and mandibular changes. The increase in vertical measurement and the decrease in overbite were minimised because of the skeletal anchorage support during the protraction and because there was no intraoral unit supporting the teeth. When soft tissue measurements were evaluated, significant improvement was also observed in the soft tissue profile of the patients, with the upper lip moving forward and lower lip moving backward.
Approximately, 3.12 retrusion in the palatal plane angle with upper incisor was observed in the treatment period this can be explained by the increasing lip pressure on the maxillary incisors after eliminating the anterior cross-bite.
The rotational direction of the mandible in posterior direction and an increase in the mandibular plane was observed as an increase of 0.25 degrees(p>0.05), thus there was no significant effect on the mandible. The researchers Sar C, Kircelli BH, Elnagar MH found increases in the SN/GoGn angle of 1.2, 1.29 and 2.03 degrees. A minimal decrease of 0.19 degrees was detected in the slope of the palatal plane [10,11,24,25]. The reason for the low vertical increase in this study may be due to the pure skeletal effect and the absence of a device such as RME etc., in the mouth. The side effects in the tooth-borne anchorage caused by traditional maxillary protraction were avoided with the method used in the current study. As for the use of Apertura piriformis region anchorage, the inability to place mini-plates in the owing to limited space in patients and the 2-step local surgery involved placement and removal of mini-plates are considered to be the clinical disadvantages of this method. RME, which is frequently used in the treatment of Class III malocclusion with face mask, is known to affect the circum-maxillary sutures and forward movement of the maxilla [25-28]. In this study, A point was displaced only due to the forward movement of the maxilla without any movement in any point due to RME. In a study, Sar C et al., applied RME and mini-plates with face mask in growing patients. Maxillary protraction rates with RME and skeletal anchorage was 0.45 mm [10]; Elnagar MH et al., 0.59 mm/month [25]. In this study, Point A moved 0.53 mm/month.
Limitation(s)
The clinical studies should include the control group to differentiate the treatment applied from the changes that occur with growth and development. It is not ethical to keep these Class III patients to create a control group without treating them [29]. The control group was not included in the study due to medical ethics.
After the retention and long-term results of the studies, it attracts more attention of the readers and makes the study more valuable. As this study was retrospective and the selection was made from the archive, all patients could not be reached for long-term follow-up. This method requires long-term study and results to determine the amount of relapse and recurrence.
Conclusion(s)
The method of skeletal anchorage with Petit-type facemask is one of the alternative treatment methods in patients with high angle Class III young adolescent patients. Approximately, 3.9 mm forward movement is observed in the maxilla, while rotational movements in both the maxilla and the mandible are minimalised.
This method has minimised vertical dimensional measurements and undesirable dento-alveolar effects due to a lack of support from the teeth. Negative overjet was corrected skeletally by the maxillary advancement rather than dento-alveolar correction.
Future studies can be done comparing both in terms of different maxillary protraction methods and different anchorage units treatment effectiveness. In addition, relapse amounts can be revealed by comparing long term results in terms of relapse.
P: Results of paired t-test; SD: Standard deviation. *p<0.05; **p<0.01; ***p<0.001; NS: Not significant p>0.05