The amount of discomfort occurring during orthodontic treatment determines the acceptance of the orthodontic appliance [1]. The pain which is defined as an unpleasant feeling and a bad subjective experience is considered as the most annoying factor and the most important reason making patients refrain from seeking orthodontic treatment [2,3]. Oliver RG and Knapman YM studied the attitude of patients towards orthodontic treatment and found that pain and appearance from the appliance were the main cause of discouragment [4]. Jones ML investigated the initial discomfort due to arch wire placement [5]. Haynes SM rated the pain as the first reason which made the patient stopped the orthodontic treatment, whereas the second one was the effect of the orthodontic appliance on the patient’s daily social life [6].
All discomforts caused by orthodontic appliance have a negative effect on the degree of orthodontic appliance acceptance which reflects on the degree of patient cooperation [7]. Patient cooperation is defined medically as a range of coincidence between personal behaviour and the medical or health advice presented to him [8]. In orthodontics, cooperation is defined as a degree of patient’s response to the instructions presented to him during orthodontic treatment [9].
The therapeutic effects of a removable orthodontic appliance whatever its design are essentially based on patient cooperation [1]. Unfortunately, the removable orthodontic appliances could cause pressure on the oral mucosa, tension on soft tissues, tongue discomfort and impairments in other oral functions such as speech, swallowing and breathing, in addition to the worsening of the aesthetic appearance, and all these negative effects reduce the acceptance of removable orthodontic appliance [10]. The acceptance of a removable orthodontic appliance is affected by several factors such as appliance design, appliance volume, and appliance stability in the mouth [11].
Few studies have evaluated the patient acceptance of the orthodontic appliances used for treating Class III cases in general and Class III functional appliances in particular [2,12,13]. Removable appliances were evaluated by a series of publications by Sergl HG et al., in Germany [1,10,14]. Additionally, there are only a few Randomised Controlled Trial (RCT) in the literature that evaluated patients’ responses towards orthodontic treatment. Class II growing patients undergoing functional orthopedic treatment were evaluated by Idris G et al., [15], Khattab TZ et al., compared labial brackets versus lingual brackets in terms of speech and functional impairments [16]., whereas Saleh M et al., detected the levels of acceptance after applying the RMR when treating children with Class III malocclusion in the late primary dentition and early mixed dentition and recorded high levels of acceptance [17].
Bone-anchored intermaxillary elastics have been proposed as a method of correcting Class III deformities [18,19]. Although, bone-anchored intermaxillary traction group was compared to the removable mandibular retractor in terms of skeletal and dentoalveolar changes [20], the published paper did not report any information about the associated levels of pain and discomfort as well the general acceptability to this treatment modality. Therefore, this study was done as an extension to the previous study [20] to evaluate the levels of pain, discomfort, and acceptance between two treatment modalities of Class III correction of growing patients in the late mixed dentition period.
Materials and Methods
A randomised controlled trial was conducted at the Orthodontic Department of the University of HamaDental School (Formerly known as University of Al-Baath Dental School), Syria between February and October 2015, the total duration of the study was 12 months. This research was approved by the University of Hama Dental School Local Ethics Committee (UBDS-3819-2015PG) and was funded by the University of Hama Postgraduate Research Budget (830295205667DEN). This trial was prospectively registered at the University of Al-Baath Postgraduate Research Registry (Number: Dent12/2323/9980PG) and then it was retrospectively registered at Clinical Trials.gov (NCT03976635) on the 6th of June, 2019.
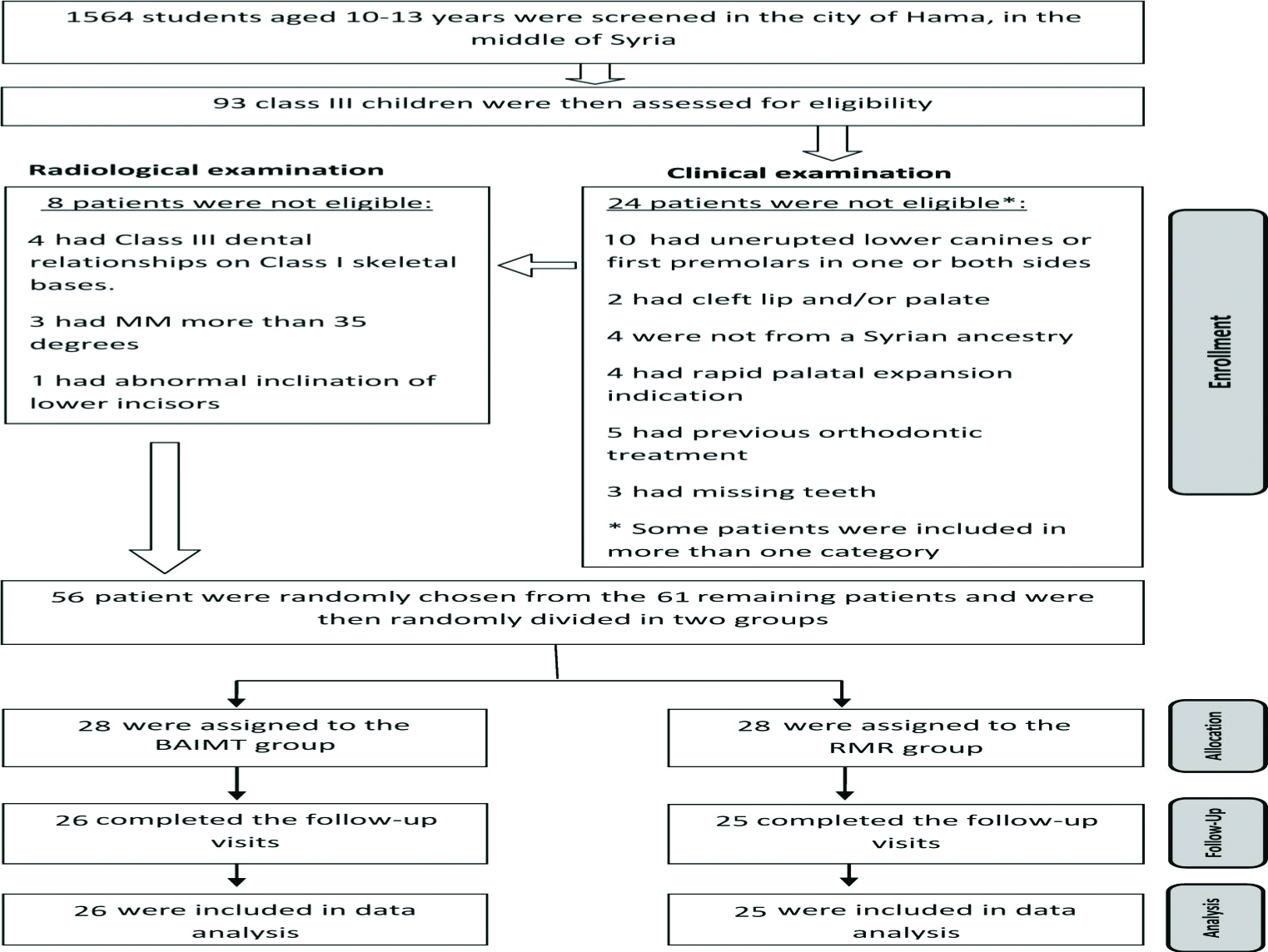
A total of 1564 primary school students were screened at seven primary schools. These schools were randomly chosen from fourteen schools in the city of Hamah. 93 Children (11-12 years) were assessed primarily by the presence of anterior crossbites. 61 subjects out of 93 were eligible to enter the RCT, 56 patients were randomly selected and assigned to the two groups in a 1:1 allocation ratio by creating a randomisation list using Minitab® V16 (Minitab Inc., Pennsylvania, PA, USA). The CONSORT flow diagram of participants’ recruitment, follow-up, and entry into data analysis is given in [Table/Fig-1].
The CONSORT flow diagram of patients’ recruitment and follow-up.
Estimation of the Sample Size
Sample size calculation was undertaken using Minitab® 16 (Minitab Inc, State College, PA, USA). It was postulated that the smallest difference requiring detection for the variable ‘Pain’ was 1 point on the 4-point Likert-scale and the standard deviation of this variable was found to be 1.23 in a previous publication [17]. Therefore, employing a two-sample t-test with a power of 80% and a 5% significance level.
Inclusion and Exclusion Criteria
Inclusion Criteria: 1) Dental class III malocclusion according to Angle; 2) Presence of anterior crossbite on two teeth or more; 3) Skeletal class III relationship confirmed radiographically (-4<ANB<+1); 4) The lower incisors have normal inclination (IMPA angle not exceeding 100° and not less than 85°); 5) Late mixed dentition or the beginning of the permanent dentition; 6) Eruption of the lower canines and first premolars on both sides; 7) Absence of craniofacial syndromes or cleft lip and/or palate abnormalities; 8) no supernumerary teeth or missing teeth except for the third molars; 9) no previous orthodontic treatment; and 10) age between 11-12 years [20].
Exclusion Criteria: 1) Diseases that prevent the application of mini-implants (e.g., Osteoporosis- cortisone and its derivatives treatment); 2) The roots of the canine are so close to the first premolar; and 3) Long face (MM angle greater than 30° or SN-MP angle greater than 36°).
Fifty-six patients (27 females and 29 males) were included in this trial, and their baseline characteristics are given in [Table/Fig-2]. Although the sample size estimation revealed that 25 patients in each group were required (i.e., 50 patients totally), additional six patients were included to avoid the risk of withdrawal (i.e., 28 patients in each group and 56 patients in total).
Baseline sample characteristics (Age and sex).
| Variable | BAIMT* (n=28) | RMR** (n=28) | Both groups (n=56) |
|---|
| Age (mean±SD) (Years) | 11.49±0.88 | 11.42±0.92 | 11.46±0.89 |
| Sex: n (%) |
| Male | 13 (46.4%) | 16 (57.1%) | 29 (51.8%) |
| Female | 15 (53.6%) | 12 (42.9%) | 27 (48.2%) |
* BAIMT: Bone-Anchored Intermaxillary Traction group;
** RMR: Removable Mandibular Retractor group
All patients were given Information sheets and their informed consent was obtained.
Intervention Group: Bone-Anchored Intermaxillary Traction (BAIMT)
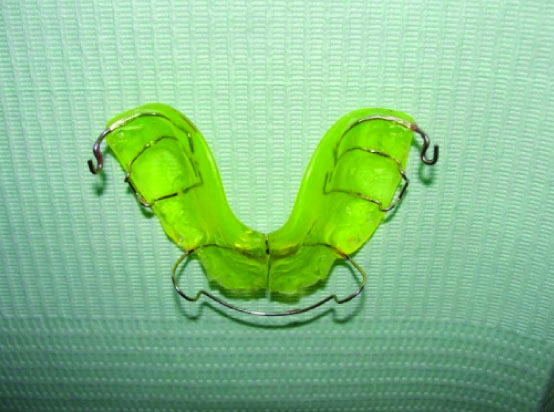
This system included: 1) upper removable appliance with bilateral posterior smooth bite plate; 2) Howley arch (0.7 mm of stainless steel); 3) Tow Adam’s clasps on the upper first molars (0.7 stainless steel wire); and 4) posterior hooks (made of 0.9-mm stainless steel wire) for attaching elastics positioned distal to the molars [Table/Fig-3] [20].
The upper removable appliance used in the BAIMT group.
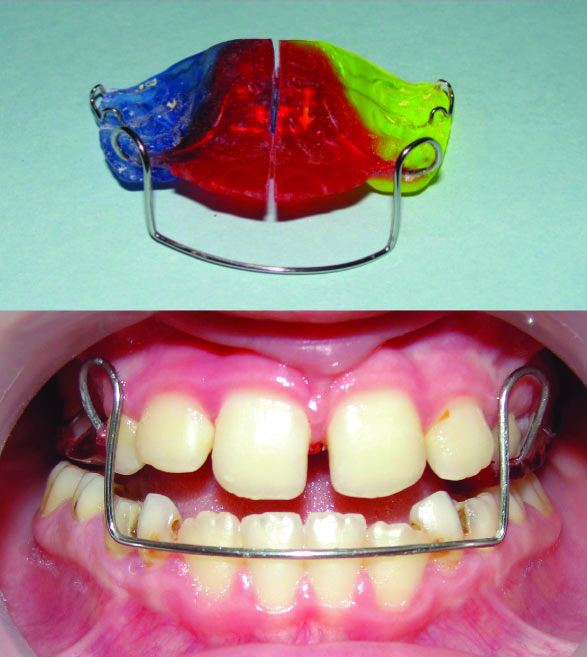
Two micro-implants (O.S.A.S., Dewimed®, Tuttlingen, Germany; 1.6-mm diameter, 8-mm length) were applied under local anaesthesia into the buccal alveolar bone between the roots of mandibular canine and first premolar on both sides with about 45-60° insertion angle with alveolar bone. To assure a proper insertion without injuring neighboring roots, a periapical radiograph was taken beforehand. After one week of insertion, intermaxillary elastics (American Orthodontics, Sheboygan, WI, USA) were applied between the mandibular micro-implants and the upper removable appliances’ hooks [Table/Fig-4], generating a 125-g force per side of the jaw in the first week (5/16-inch) followed by 3/16 medium size generating of about 200-g per side until the end of treatment [20]. Patients were asked to wear elastics for 16 hours per day, replace elastics on a daily basis or when they were damaged.
The application of intermaxillary elastics in the BAIMT group.

Control Group: the Removable Mandibular Retractor (RMR)
The design of RMR is given in [Table/Fig-5]. The RMR was applied for 16 hours per day, including bedtime. The appliance was activated every 20 days to ensure the passive touch of the reverse bow with the cervical regions of the lower anterior teeth.
The Removable Mandibular Retractor appliance.
In both groups, in order to keep the patients under control regarding their compliance, all patients in both groups were seen following appliances’ application within one week and two week sequentially. After that monthly visits started in which Adam’s clasps were tightened and the incisor relationships were observed until the transition from a negative into a positive overjet was achieved as a sign of a successful treatment [21].
Outcome Measure: Questionnaire
A standardised questionnaire was used to assess pain, discomfort and functional impairments’ levels during the first six months of treatment. This questionnaire was first suggested by Sergl HG and Zentner A, modified by Saleh M et al., and was further modified by us to conform to the current trial [14,17]. This questionnaire was written in a clear Arabic language. A pilot study was performed on the intended questionnaire (included six questions) to detect any difficulty in understanding its contents and any additional complaints that could have arisen by the wear of the two appliances. The pilot study sample consisted of ten Class III subjects (5 males and 5 females). The mean age of the sample was 11 years±3 months. The questionnaires were filled after 1 week (T1) and after 2 weeks (T2). The pilot study revealed that there was no requirement for any modification.
This questionnaire had the following six questions: 1) Do you have a sense of tension and pressure in soft tissue?; 2) Have you experienced any degree of pain or discomfort; 3) Do you feel that your articulation has changed?; 4) Do you have difficulty in swallowing?; 5) Do you have a sense of your mandible movement being restricted?’; and 6) Do you have any feeling of embarrassment or lack of confidence. Four possible answers of a Likert scale were used and given in [Table/Fig-6]. Each questionnaire was filled by the patient in the presence of one of his/her parents at the following assessment times: (T1) one day following appliance insertion, (T2) one week later, (T3) six weeks later, (T4) after three months and (T5) after 6 months of appliance insertion.
Patient responses on the questionnaires administered at five assessment times following appliance’ placement in the two groups.
| BAIMT group | RMR group |
|---|
| Patients’ response % | Patients’ response % |
|---|
| Q | 0 | 1 | 2 | 3 | p (vs T0) | 0 | 1 | 2 | 3 | p (vs T0) |
|---|
| Q1 |
| T1 | 5.26 | 10.53 | 36.84 | 47.37 | <0.001* | 15.79 | 57.89 | 15.79 | 10.53 | <0.001* |
| T2 | 10.53 | 10.53 | 52.63 | 26.32 | <0.001* | 26.32 | 52.63 | 10.53 | 10.53 | 0.001* |
| T3 | 15.79 | 36.84 | 42.11 | 5.26 | <0.001* | 42.11 | 42.11 | 10.53 | 5.26 | 0.004* |
| T4 | 42.11 | 36.84 | 15.79 | 5.26 | 0.004* | 57.89 | 36.84 | 5.26 | 0.00 | 0.014* |
| T5 | 57.89 | 31.58 | 5.26 | 5.26 | 0.014* | 78.95 | 21.05 | 0.00 | 0.00 | 0.1 |
| Q2 |
| T1 | 5.26 | 5.26 | 36.84 | 52.63 | <0.001* | 63.16 | 21.05 | 10.53 | 5.26 | 0.022* |
| T2 | 5.26 | 21.05 | 52.63 | 21.05 | <0.001* | 68.42 | 21.05 | 5.26 | 5.26 | 0.036* |
| T3 | 21.05 | 36.84 | 31.58 | 10.53 | 0.001* | 73.68 | 15.79 | 10.53 | 0.00 | 0.059 |
| T4 | 47.37 | 31.58 | 15.79 | 5.26 | 0.006* | 78.95 | 21.05 | 0.00 | 0.00 | 0.1 |
| T5 | 63.16 | 26.32 | 5.26 | 5.26 | 0.022* | 89.47 | 10.53 | 0.00 | 0.00 | 0.371 |
| Q3 |
| T1 | 5.26 | 57.89 | 31.58 | 5.26 | <0.001* | 0.00 | 5.26 | 15.79 | 78.95 | <0.001* |
| T2 | 15.79 | 63.16 | 15.79 | 5.26 | <0.001* | 0.00 | 10.53 | 31.58 | 57.89 | <0.001* |
| T3 | 42.11 | 42.11 | 10.53 | 5.26 | 0.004* | 5.26 | 5.26 | 52.63 | 36.84 | <0.001* |
| T4 | 68.42 | 21.05 | 5.26 | 5.26 | 0.036* | 10.53 | 21.05 | 52.63 | 15.79 | <0.001* |
| T5 | 73.68 | 21.05 | 5.26 | 0.00 | 0.059 | 15.79 | 42.11 | 31.58 | 10.53 | <0.001* |
| Q4 |
| T1 | 47.37 | 42.11 | 5.26 | 5.26 | 0.006* | 31.58 | 42.11 | 15.79 | 10.53 | 0.002* |
| T2 | 63.16 | 26.32 | 5.26 | 5.26 | 0.022* | 36.84 | 36.84 | 21.05 | 5.26 | 0.003* |
| T3 | 73.68 | 15.79 | 5.26 | 5.26 | 0.059 | 52.63 | 31.58 | 10.53 | 5.26 | 0.009* |
| T4 | 84.21 | 5.26 | 5.26 | 5.26 | 0.181 | 57.89 | 36.84 | 5.26 | 0.00 | 0.014* |
| T5 | 89.47 | 5.26 | 5.26 | 0.00 | 0.371 | 68.42 | 31.58 | 0.00 | 0.00 | 0.036* |
| Q5 |
| T1 | 63.16 | 26.32 | 5.26 | 5.26 | 0.022* | 5.26 | 21.05 | 63.16 | 10.53 | <0.001* |
| T2 | 73.68 | 15.79 | 5.26 | 5.26 | 0.059 | 5.26 | 31.58 | 57.89 | 5.26 | <0.001* |
| T3 | 84.21 | 5.26 | 5.26 | 5.26 | 0.181 | 10.53 | 47.37 | 36.84 | 5.26 | <0.001* |
| T4 | 84.21 | 10.53 | 5.26 | 0.00 | 0.181 | 31.58 | 47.37 | 21.05 | 0.00 | 0.002* |
| T5 | 89.47 | 10.53 | 0.00 | 0.00 | 0.371 | 52.63 | 36.84 | 10.53 | 0.00 | 0.009* |
| Q6 |
| T1 | 42.11 | 36.84 | 10.53 | 10.53 | 0.004* | 10.53 | 10.53 | 36.84 | 42.11 | <0.001* |
| T2 | 47.37 | 36.84 | 10.53 | 5.26 | 0.006* | 10.53 | 10.53 | 36.84 | 42.11 | <0.001* |
| T3 | 63.16 | 31.58 | 0.00 | 5.26 | 0.022* | 10.53 | 21.05 | 42.11 | 26.32 | <0.001* |
| T4 | 68.42 | 26.32 | 5.26 | 0.00 | 0.036* | 21.05 | 26.32 | 42.11 | 10.53 | 0.001* |
| T5 | 78.95 | 21.05 | 0.00 | 0.00 | 0.1 | 26.32 | 31.58 | 31.58 | 10.53 | 0.001* |
Possible answers: 0 indicates “No, not at all”; 1, “Slightly”; 2, “Yes, to some degree”; and 3, “Yes, indeed, I can confirm this.’ * A significant difference=p<0.05, The statistical test was Wilcoxon signed-rank matched-pairs
Statistical Analysis
Descriptive and inferential statistics were performed using Minitab® V15 (Mintab Inc., Pennsylvania, USA). Wilcoxon signed-rank matched-pairs tests were used to detect significant differences between assessment times, whereas Mann-Whitney U tests were used to detect significant differences between the two groups. The level of significance was set at 0.05.
Results
Baseline Sample Characteristics
The BAIMT group (A mean age of 11.3 years) and the control group RMR group (A mean age of 11.5 years). The baseline characteristics of the included patients in each group are shown in the [Table/Fig-2].
Questionnaire Findings
At T0, all answers in relation to the six questions were identical (patients chose answer “no, not at all”). Therefore, these data are omitted from the [Table/Fig-6] and the [Table/Fig-7].
Comparison between the two groups at five assessment times.
| BAIMT group | RMR group | p-value BAIMT vs RMR |
|---|
| Q | Mean | SD | Mean | SD |
|---|
| Q1 | | | | | |
| T1 | 2.26 | 0.87 | 1.21 | 0.86 | 0.001* |
| T2 | 1.95 | 0.91 | 1.05 | 0.91 | 0.004* |
| T3 | 1.37 | 0.83 | 0.79 | 0.86 | 0.032* |
| T4 | 0.84 | 0.90 | 0.47 | 0.61 | 0.210 |
| T5 | 0.58 | 0.84 | 0.21 | 0.42 | 0.136 |
| Q2 | | | | | |
| T1 | 2.37 | 0.83 | 0.58 | 0.90 | <0.001* |
| T2 | 1.90 | 0.81 | 0.47 | 0.84 | <0.001* |
| T3 | 1.32 | 0.95 | 0.37 | 0.68 | 0.002* |
| T4 | 0.79 | 0.92 | 0.21 | 0.42 | 0.028* |
| T5 | 0.53 | 0.84 | 0.11 | 0.32 | 0.054 |
| Q3 | | | | | |
| T1 | 1.37 | 0.68 | 2.74 | 0.56 | <0.001* |
| T2 | 1.11 | 0.74 | 2.47 | 0.70 | <0.001* |
| T3 | 0.79 | 0.86 | 2.21 | 0.79 | <0.001* |
| T4 | 0.47 | 0.84 | 1.74 | 0.87 | <0.001* |
| T5 | 0.32 | 0.58 | 1.37 | 0.90 | <0.001* |
| Q4 | | | | | |
| T1 | 0.68 | 0.82 | 1.05 | 0.97 | 0.214 |
| T2 | 0.53 | 0.84 | 0.95 | 0.91 | 0.105 |
| T3 | 0.42 | 0.84 | 0.68 | 0.89 | 0.227 |
| T4 | 0.32 | 0.82 | 0.47 | 0.61 | 0.142 |
| T5 | 0.16 | 0.50 | 0.32 | 0.48 | 0.155 |
| Q5 | | | | | |
| T1 | 0.53 | 0.84 | 1.79 | 0.71 | <0.001* |
| T2 | 0.42 | 0.84 | 1.63 | 0.68 | <0.001* |
| T3 | 0.32 | 0.82 | 1.37 | 0.76 | <0.001* |
| T4 | 0.21 | 0.54 | 0.90 | 0.74 | 0.002* |
| T5 | 0.11 | 0.32 | 0.58 | 0.69 | 0.012* |
| Q6 | | | | | |
| T1 | 0.90 | 0.99 | 2.11 | 0.99 | 0.001* |
| T2 | 0.74 | 0.87 | 2.11 | 0.99 | <0.001* |
| T3 | 0.47 | 0.77 | 1.84 | 0.96 | <0.001* |
| T4 | 0.37 | 0.60 | 1.42 | 0.96 | <0.001* |
| T5 | 0.21 | 0.42 | 1.26 | 0.99 | <0.001* |
* A significant difference P<0.05; The statistical tests were Mann-Whitney U-tests
Answers to Question 1: ‘Do you have a Sense of Tension and Pressure in Soft Tissue?’
One day following appliances’ placement, the patients of both groups reported a highly significant increase of pressure and tension in the soft tissue. Gradual improvements in patients’ assessment were recorded by the time [Table/Fig-6]. However, the differences were significant during all assessment times in the BAIMT group and till six weeks (T3) in the RMR group when compared to the data obtained before insertion the appliances (T0). Significant inter-group differences with respect to tension and pressure in soft tissue were detected only at T1, T2 and T3 (p=0.001, p=0.004, p=0.032, respectively).
Answers to Question 2: ‘Have you Experienced any Degree of Pain?’
Patients in the BAIMT group reported significantly higher degrees of pain than what was recorded by patients in the RMR group [Table/Fig-7]. Significant differences were detected at all assessment times in the BAIMT group when compared to the records obtained at T0, whereas these differences were significant only at T1 (p=0.022) and T2 (p=0.036) in the RMR group [Table/Fig-6]. After six months of intervention (T5), the pain disappeared for almost all the patients in the RMR group but still noticed to some degrees by the patients in the BAIMT group with an insignificant intergroup difference at this time point (p=0.054).
Answers to Question 3: ‘Do you feel that your Articulation has changed?’
In the RMR group, the patients reported a highly significant deterioration of their articulation immediately following appliance’ insertion (p<0.001). At the subsequent assessment times, remarkable improvements of patients’ assessment for their speech were observed; nevertheless, the articulation was still given a significantly poorer rating than what was recorded at T0 [Table/Fig-6]. Lower levels of speech impairments were recorded by the patients in the BAIMT group and the differences between the two groups were statistically significant at all assessment times (p<0.001; [Table/Fig-7]).
Answers to Question 4: ‘Do you have Difficulty in Swallowing?’
After appliance’ placement, some degrees of swallowing difficulties were recorded in both groups. Although these difficulties were more often observed by patients in the RMR group, the differences between the two groups were insignificant at all assessment time points [Table/Fig-7].
Answers to Question 5: ‘Do you have a Sense of your Mandible Movement being Restricted?’
In both groups, the patients complained about some degrees of mandibular movement restriction one day following insertion (T1). Important improvements were observed later in the BAIMT group as the majority of patients (approx. 90%) stated that they were able to move their mandibles freely after six months of appliance placement (T5). However, the restriction of mandibular movements was more often encountered in the RMR group with significant intergroup differences at all assessment times.
Answers to Question 6: ‘Do you have any Feeling of Embarrassment or Lack of Confidence?’
There were significant differences between the two groups regarding the levels of shyness and lack of confidence after appliances’ placement at all assessment times (p<0.001). More than half of the patients in the RMR group rated their lack of confidence to be at moderate to severe levels until three months of intervention (T4). After six months of appliances’ insertion (T5), the majority of patients (≈79%) in the BAIMT group stated that they had no treatment-related shyness, whereas approximately the same percentage of patients in the RMR group was still suffering from different levels of lack of confidence at this point of time [Table/Fig-6].
Discussion
In this randomised controlled trial, a relatively new method of skeletal-anchored intermaxillary traction was compared to a traditional way of treating Class III malocclusion using the removable mandibular retractor. These two treatment protocols differ in terms of appliance design, force vectors, force application points, and treatment duration; however, each of these appliances has its effects on oral comfort. Therefore, this study was conducted to compare the level of pain, discomfort and acceptance between these two treatment modalities.
In the current study, the pressure and tension of the soft tissue were more intense in the BAIMT group. This finding can be explained by the difference in the intermaxillary action between the two treatment protocols; in the BAIMT group the use of intermaxillary Class III elastics which extended from the upper appliance’ hooks to the lower mini-implants may have caused more tension power between the two jaws than what did the removable mandibular retractor in the RMR group, in which the intermaxillary effects concentrated on the cervical portion of the lower anterior teeth as stated previously by Saleh M et al., [21]. Previous studies have reported lower degrees of tension and pressure in the soft tissue than what was recorded in the BAIMT group in the present study, this can be explained by the application of an approximately continuous action provided by the intermaxillary elastics [10,12].
Higher degrees of pain were recorded by patients in the BAIMT group especially immediately after appliance’ placement. It seems to be that this pain was mostly caused by the insertion of mini-implants. This finding was not in agreement with either the study by Lee TCK et al., who stated that 72.2% of their subjects reported a little pain [22] or the study by Kuroda S et al., in which only 25% of the patients reported pain after mini-implants’ insertion [23]. However, this perception of pain gradually decreased by time but was still significantly higher than what was recorded at T0. The traction caused by the Class III intermaxillary elastics may have played a role in this long-term feeling of pain. The relatively low levels of pain reported by the patient in the RMR group were in agreement with those reported by Saleh M et al., who stated that most patients had no pain feeling after one week of appliance use [21].
Significant deteriorations of speech were recorded in both groups but significantly higher in the RMR group. Important speech problems disappeared within three months after appliance placement for almost all patients in the BAIMT group but still reported by about half of the patients in the RMR group. Speech impairments are common during orthodontic treatment; however, some appliances have an interfering effect of speech production over other appliances [16]. Saleh M et al., reported lower degrees of speech impairments after applying the Removable Mandibular Retractor (RMR) than what was found in the current study [21], this difference might be due to the variation of age range between the two studies. In the current study, the older aged patients (mean age 11.5) were more capable to recognise speech disturbances than the patients of mean age 7.6 who were treated by Saleh M et al., [21].
Some swallowing difficulties were reported by the patients during assessment times with insignificant differences between the two groups. This finding can be interpreted by the presence of the bilateral posterior bite blocks in both groups which in turn prevented normal mastication and swallowing procedures. This finding was comparable with that by Stewart FN et al., who found that swallowing difficulties were more observed with removable appliances due to a relatively large bulk of the acryl that impaired the general oral activities including swallowing [24].
The presence of the reverse Hawley bow which was fabricated to seat at the level of the cervical portion of the lower anterior teeth has been found to have a significant impact on mandibular movement restriction in the RMR group in which patients still reported some degrees of restriction of the mandibular movement even after six months of intervention. On the other hand, the lower levels of restrictions recorded by the subjects in the BAIMT group can be explained by the fact that the intermaxillary traction generated by the Class III elastics decreases rapidly by time unlike the traction provided by the stainless steel wire of the Hawley bow in the RMR group.
As expected, patients treated with the RMR recorded more levels of shyness and lack of confidence than those treated in the BAIMT group. This finding can be explained by two reasons: (1) the presence of the anterior reverse Hawley bow made the RMR appliance more visible to the others when compared with the lateral positioned intermaxillary elastics in the BAIMT group, and (2) the higher levels of speech difficulties experienced by the patients in the RMR group than what was reported by the BAIMT group patients. It has been shown in previous reports that patients’ confidence is directly affected by both the visibility of the orthodontic appliance and the impairments of speech caused by this appliance [16]. Our results do not agree with those by Saleh M et al., who recorded lower levels of shyness and lack of confidence than what was found in the RMR group in the current study [21]. Again, this difference can be explained by the different age range, the patients included in the present study were older and had more developed social relationships especially in the school.
According to the findings of this study, the most life-affecting difficulties like speech impairment, mandibular movement restriction and lack of confidence were found to be more noticed by the patients with the RMR at all assessment times. On the other hand, the patients in the BAIMT group recorded higher levels of pain and soft tissue tension especially after appliances’ placement, and important improvements of these parameters occurred during observation periods.
Limitation(s)
The generalizability of these results might be limited. In this trial, a specific design of a bone-anchored intermaxillary traction technique was applied in which a removable appliance was used as an upper anchorage unit, however, mini-implants and mini-plates are employed recently for this purpose and yet not considered in the current study. Another source of limitation is that the oral impacts were subjectively assessed by patients and therefore might have been influenced by their emotional status and environmental factors.
Conclusion(s)
Impairments of oral functions were commonly observed during the early treatment stages of both appliances. However, these impairments gradually decrease by time. Patients treated with the BAIMT technique experienced more degrees of pain and soft tissue tension than patients treated with the removable mandibular retractor, especially at the first stage of treatment. Patients treated with the removable mandibular retractor suffered from speech impairment, mandibular movement restriction and lack of confidence more than those treated with the BAIMT technique at all assessment times. However, there is a need for further investigations to evaluate the influence of different available types of BAIMT techniques on oral comfort and patient acceptance.