Correspondence- ‘Role of Diffusion Weighted Imaging in Differentiating Benign from Pathological Vertebral Collapse using ADC Values’; Is It Possible to Discriminate Multiple Myeloma with Magnetic Resonance Imaging?
Takahiko Nagamine1
1 Doctor, Department of Emergency Medicine, Sunlight Brain Research Center, Hofu, Yamaguchi, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Takahiko Nagamine, 4-13-18 Jiyugaoka, Hofu, Yamaguchi, Japan.
E-mail: tnagamine@outlook.com
Dear Editor,
I read with great interest the article by Mahale R et al., reporting a novel technique to evaluate vertebral fractures [1]. I recently experienced a compression fracture patient with Multiple Myeloma (MM) and tried Mahale’s method to distinguish between benign and malignant collapses. I admire Mahale’s method, but more research is needed to apply this method. A fractured patient with MM was presented and this method was discussed.
Vertebral collapse as a result of osteoporosis, infection or malignant diseases are very common. Since the management and prognosis differs in these entities, it is extremely important to make a sharp distinction between benign and malignant collapses. Magnetic Resonance Imaging (MRI) is the established technique for distinguishing imaging features. However, vertebral collapses caused by MM seldom show malignant signs on MRI [2].
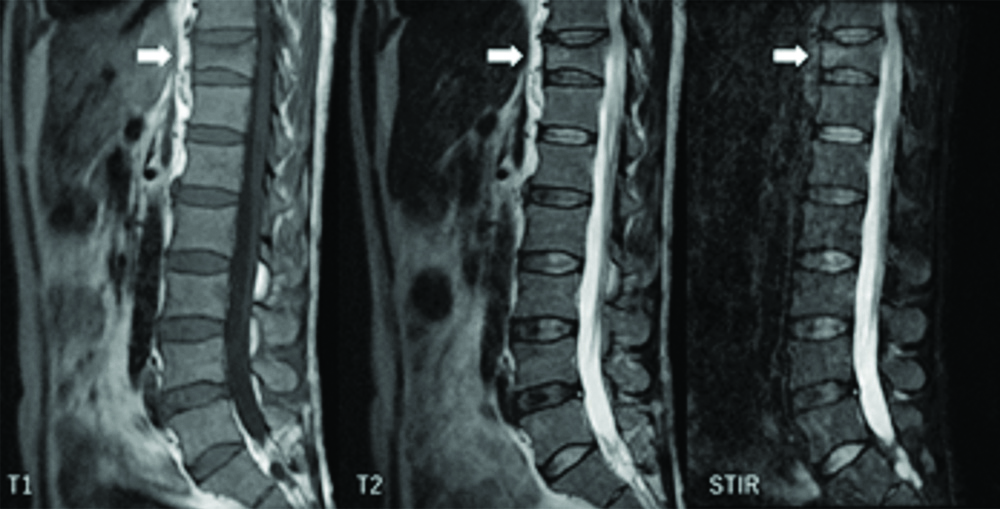
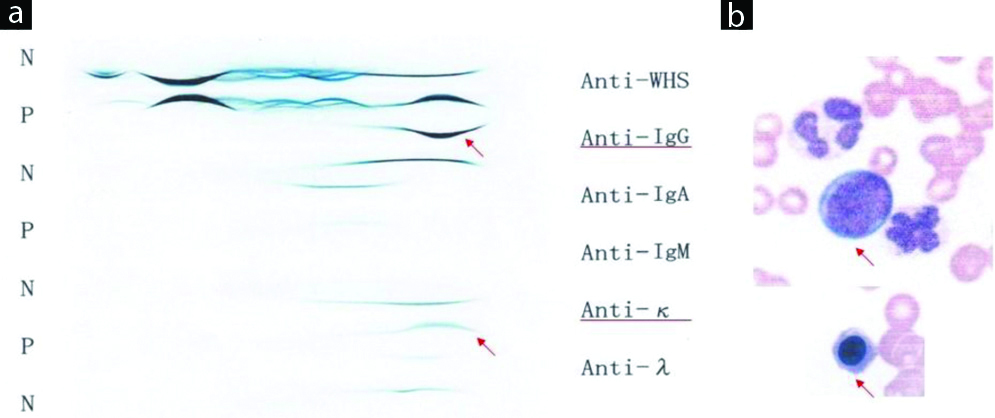
A 52-year-old Japanese man with no significant past medical history, presented to an orthopaedic clinic with severe low back pain. X-ray of his spine revealed compression fracture at 11th thoracic spine (Th11). He was started on non-steroidal anti-inflammatory drugs. But his mobility gradually declined due to severe resting pain over the next two weeks and finally transferred to our hospital. MRI of his Th11 spine showed a band sign with low signal on T1-weighted image and a slight high signal on Short-Tau Inversion Recovery (STIR) image that is compatible with benign vertebral fracture [Table/Fig-1]. I performed Diffusion Weighted Imaging (DWI) was done on the patient to confirm his spinal pathology, resulted that Apparent Diffusion Co-Efficient (ADC) value was calculated as 1.1×10-3 mm2/s which was just the borderline between benign and malignant collapses. However, his serum protein level was high (10.5 g/dL). Serum immuno-electrophoresis indicated a monoclonal gammopathy with a markedly elevated immunoglobulin G level in association with a kappa light chain [Table/Fig-2a]. Some large unclassified cell and erythroblast were seen in his peripheral blood [Table/Fig-2b]. He was diagnosed as having MM with plasmablastic transformation. Anti-myeloma treatment including melphalan and prednisone started after confirmation of the diagnosis by bone marrow examination and led to a decline in monoclonal immunoglobulin G concentration.
Magnetic Resonance Image (MRI) shows a band pattern at Th11 that appears as areas of low signal on T1-weighted image and slight high signal on Short-Tau Inversion Recovery (STIR) image (white arrows), indicative of osteoporotic benign vertebral fracture.
(a) Serum immuno-electrophoresis indicated a monoclonal elevation of immunoglobulin G level with a kappa light chain (red arrows); (b) Peripheral blood smear showed a large unclassified cell and erythroblast (red arrows).
A band-like signal on MRI that was seen in present patient was mainly associated with benign collapses. On the contrary, posterior wall diffuse protrusion, pedicle involvement, and posterior involvement strongly indicate malignant collapses, which was not seen in present patient. Malignant collapses caused by MM may sometimes show benign features on MRI [3]. I read with great interest the article by Mahale R et al., reporting a novel technique to evaluate vertebral fractures [1]. They stated that ADC values could distinguish malignant collapses from benign fractures. Benign collapses have less barriers for the movement of water molecules whereas malignant collapses have numerous cellular tissues, resulted in diffusion restriction. Therefore, the ADC value of malignant collapses is significantly higher than that of benign collapses. However, the index patient’s ADC value was just borderline between benign and malignant according to the Mahale’s criteria [3].
At present, the clinical application of DWI may remain a challenge probably because technical factors including the definition of Regions Of Interest (ROI) and DWI protocols could influence the results of the ADC values. Further studies are needed to confirm the efficacy of adding DWI to conventional MRI in order to detect malignant vertebral fractures.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 11, 2019
Manual Googling: Feb 18, 2020
iThenticate Software: Feb 22, 2020 (10%)
[1]. Mahale A, Maruvaneni S, Kumar A, Ullal S, Fernandes M, Role of diffusion weighted imaging in differentiating benign from pathological vertebral collapse using ADC valuesJ Clin Diagn Res 2019 13(2):TC01-05. [Google Scholar]
[2]. Mauch JT, Carr CM, Cloft H, Diehn FE, Review of the imaging features of benign osteoporotic and malignant vertebral compression fracturesAJNR Am J Neuroradiol 2018 39(9):1584-92.10.3174/ajnr.A552829348133 [Google Scholar] [CrossRef] [PubMed]
[3]. Takigawa T, Tanaka M, Sugimoto Y, Tetsunaga T, Nishida K, Ozaki T, Discrimination between malignant and benign vertebral fractures using magnetic resonance imagingAsian Spine J 2017 11(3):478-83.10.4184/asj.2017.11.3.47828670417 [Google Scholar] [CrossRef] [PubMed]