One of God’s most precious gift to humankind is his vision. The eventual moulding of a person’s potentiality lies in his nature, his environments and the quality of his eyesight. Childhood is the formative period which determines one’s physical, intellectual and behavioural pattern. Any problem in vision during these years can hamper the performance of a child in future [1]. Refractive error is an optical system defect intrinsic to the eye, which precludes the light from getting focussed at the retina; thus, reducing normal vision [2]. Refractive error which is left uncorrected is the prime cause of subnormal vision across the world and the second cause of “treatable blindness” [3,4]. It was observed that about 2.3 billion people around the world have refractive errors. Out of these, only few ie 1.8 billion have access to an ophthalmologist for consultation and its correction which leaves around 500 million people, mostly in developing countries, with uncorrected refractive error [5]. Strikingly, 12.8 million are visually impaired because of refractive errors in 5-15-year-old children [6]. Children adapt to the subnormal eyesight by sitting close to the blackboard, keeping their books closer to the eyes while reading, squeesing their eyes and ultimately ignoring work which requires visual concentration. Neither are children mature enough to indicate their difficulties related to vision at an early stage nor the parents are able to notice the gradual development of the refractive error; hence screening is essential [7]. It secondarily has a significant effect on a child’s future employment, earning capacity, family and community, ultimately affecting the growth of a country as a whole.
It is a priority on the global level to undertake an initiative for the elimination of avoidable blindness by WHO: VISION 2020- The Right to Sight [8,9].
Another essential problem often left ignored, which must be looked into in these formative years, is of Colour Blindness. Congenital cases are usually X linked recessive, hence seen mostly in males [10]. Colour-blind people are usually unaware of their defect and they adapt to the environment [11]. Its early detection will allow the parents and teachers to make necessary alterations in teaching [12]. This study can help to plan a practical approach and tackle the burden of readily correctable refraction problems in children of 6-15 years of age group and it can also raise awareness regarding the current statistics on the burden of refractive error and colour blindness in school-going children in this area. Hence, the present study was carried out with an aim to find the prevalence of refractive error among school-going children between 6 to 15 years of age group in Wardha, to find out the different forms of refractive error among the study group, and to find out the prevalence of colour blindness in the study group.
Materials and Methods
A Prospective cross-sectional study was conducted from September 2017-August 2019 in six co-educational schools of Wardha district in which school camps were organised and students of age 6-15 years and of classes 1st to 10th standard participated. Wardha district comprises of 8 Tehsils (Ashti, Karanja, Arvi, Seloo, Wardha, Deoli, Hinganghat, Samudrapur). Population or Wardha District: is 1,300,774 (total population, including institutional and household population). The population of Urban Wardha being-106,444. The Sex Ratio Of Wardha District is 946 [13]. The institutional ethics committee approved the study (IEC Clearance number: DMIMS(DU)/IEC/2017-18/6659) and Prewritten informed consent forms explaining the nature of study and requirement for mydriasis if the subnormal vision was diagnosed was distributed to the parents before the camps were conducted. However, all students were screened according to the school health camp.
Inclusion Criteria
School going children of age 6 years-15 years who were randomly selected and whose parents or legal guardians were ready to give informed consent. The co-educational schools in the study were randomly selected to ensure adequate representation of population.
Exclusion Criteria
Five-year-old children as they tend to be uncooperative for the visual acuity test as suggested by the study on a refractive error by Dandona R et al., were excluded and non-cooperative child, children with conditions that affect visual functions other than refractive errors like: Corneal opacities and Cataracts, ocular injuries and Ptosis were also excluded [14]. Taking 10.12% as prevalence of refractive error with reference to a study performed by Deshpande Jayant D and Malathi K where they studied the prevalence of ocular morbidities among school children in North and according to it a sample size of 725 patients was needed and present study targeted 865 participants [15].
The list of all students was taken from attendance register along with age, address, parents occupation. All students aged 6-15 years from the selected class, except those who were absent were screened. Children were inquired regarding present and past ophthalmological complaints. Torchlight examination was performed. Snellen’s chart was used to take visual acuity for distance. Visual acuity testing for near vision was done by Jaeger’s chart. Colour vision was taken using Ishihara chart (38 plate version) in a well-illuminated room at a distance of 75 centimetres [16]. Visual acuity of students already wearing glasses was also taken for further improvement. If the vision was less than or equal to 6/9 according to Snellen’s chart, Retinoscopy was performed using a self-illuminating streak retinoscope (HEINE) after mydriasis by homatropine keeping a working distance of 66 cm. A 2% Homatropine (eye drops were put in the conjunctival sac twice (15 minutes apart). If the dilation was not achieved, it was repeated after 30 minutes. Children were re-evaluated for pupillary reaction and dilatation. Cycloplegia considered to be complete if the pupillary dilation was more than 6 mm with no pupillary light reflex. Retinoscopy was then performed by self illuminating streak retinoscope. All children diagnosed to have refractive errors were documented, and different patterns of refractive errors were noted. Refractive error was classified according to the following definitions:
Myopia: Error of at least -0.50D, Hypermetropia of at least +0.50D and Astigmatism ≥0.50 D was considered as visually significant and Visual Impairment was determined based on ICD 10
MVI: moderate visual impairment (<6/18-6/60)
SVI: Severe Visual impairment (<6/60-3/60) [17]
Statistical Analysis
The Statistical analysis was performed by using “descriptive and inferential statistics” using “chi-square test” and software used in the analysis were “SPSS 24.0 version” and “GraphPad Prism 7.0 version” and the p-value of <0.05 was considered as significant.
Results
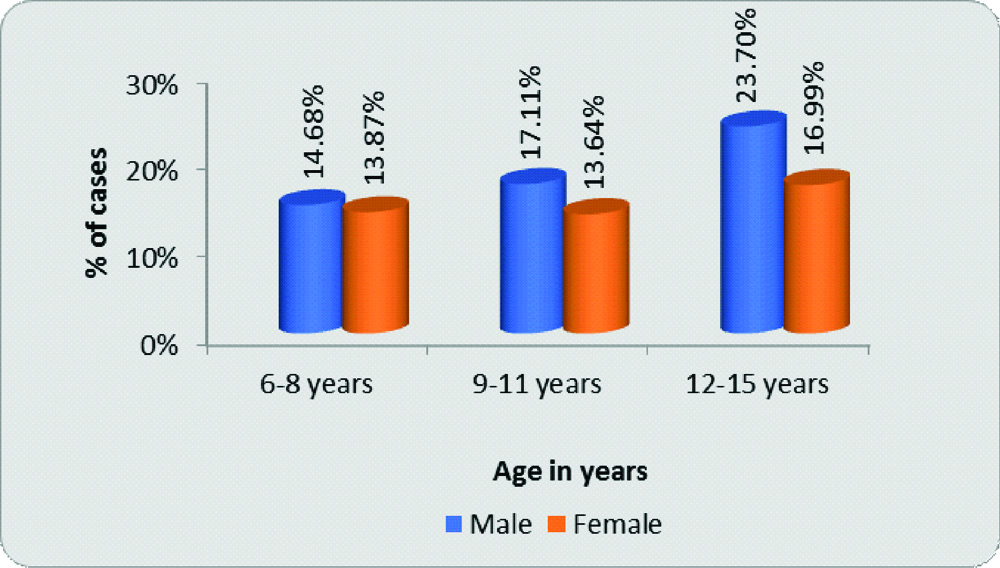
The prevalence of refractive error was reported to be 18.61% and the colour blindness as 1.62%. In 6-8 years, 127 (14.68%) were males, 120 (13.87%) were females; 9-11 years group had 148 (17.11%) males and 118(13.64%) females and among 12-15 years children, 205 (23.70%) males and 147 (16.99%) females. Mean age group of population under study was 10.53±2.85 years, males being 10.63±2.84 years and females 10.39±2.87 years [Table/Fig-1].
Age and gender-wise distribution of population screened.
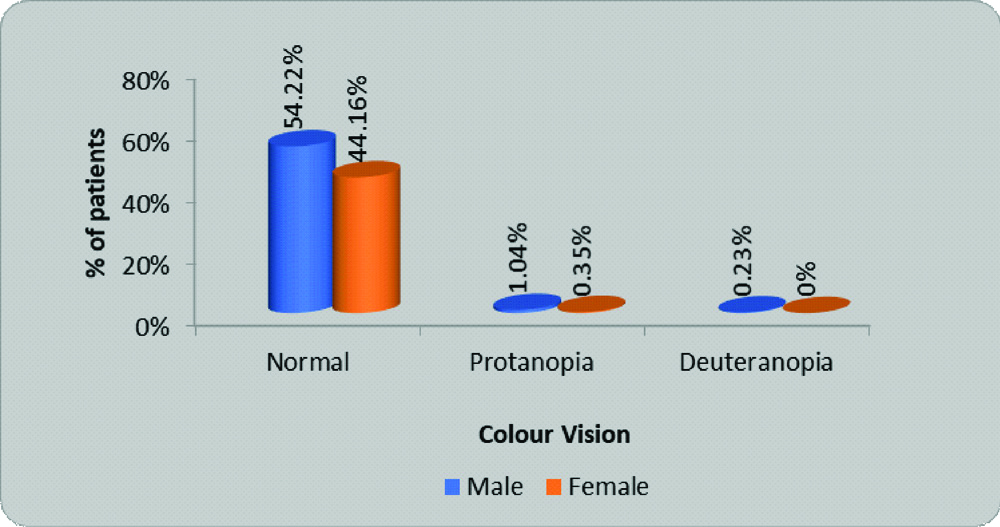
The prevalence of colour blindness in present study was 1.62% and among protans, 1.045% were male, and 0.35% were females. Among deutans 0.23% were male children [Table/Fig-2].
Distribution of colour vision among cases.
Out of the total of 865 students screened, 704 (81.39%) had Emmetropia, and 161 (18.61%) had Ametropia. Maximum students (88.67%) belonged to class I according to Modified Prasad scale [18], followed by class II (8.21%) and then class I (3.12%). In our study, out of 161 patients who had a refractive error, 95 (59.01%) children had Myopia, 43 (26.71%) children had Astigmatism and 23 (14.29%) children had Hypermetropia [Table/Fig-3].
Age and refractive errors.
| Refractive errors | 6-8 years | 9-11 years | 12-15 years | Total |
|---|
| Myopia | 6 | 19 | 70 | 95 (59.01%) |
| Hypermetropia | 6 | 9 | 8 | 23 (14.29%) |
| Astigmatism | 6 | 13 | 24 | 43 (26.71%) |
| Total | 18 (11.18%) | 41 (25.47%) | 102 (63.35%) | 161 (100%) |
Value of χ2: 29.49; p-value: 0.0001; Significant
The number of cases of refractive errors increased with advancing age. Myopia was the most predominant type of refractive error in all the age groups and the results were statistically significant [Table/Fig-3].
There was no significant association between gender and refractive error [Table/Fig-4].
Gender and refractive errors.
| Refractive errors | Male | Female | Total |
|---|
| Myopia | 51 | 44 | 95 (59.01%) |
| Hypermetropia | 16 | 7 | 23 (14.29%) |
| Astigmatism | 23 | 20 | 43 (26.71%) |
| Total | 90 (55.90%) | 71 (44.10%) | 161 (100%) |
Value of χ2: 4.07; p-value: 0.13; Not Significant
Majority of children diagnosed to have refractive errors were categorised as having no visual impairment and 2.48% of children were categorised as blind (<3/60) [Table/Fig-5].
Distribution of cases of refractive errors according to visual impairment.
| Visual impairment | No. of Cases | Percentage |
|---|
| 6/6-6/18 (Normal) | 86 | 53.42 |
| <6/18-6/60 (MVI) | 51 | 31.68 |
| <6/60-3/60 (SVI) | 20 | 12.42 |
| <3/60 (Blind) | 4 | 2.48 |
| Total | 161 | 100 |
Majority of children with refractive errors complained of blurring of vision. By applying the chi-square test of the difference between two proportions, the proportion of cases with the blurring of vision was found to be significantly higher than other symptoms (p<0.01) [Table/Fig-6].
Distribution of cases of refractive error as per symptoms.
| Symptoms | No. of patients | Percentage |
|---|
| Blurring of vision | 98 | 60.87 |
| Headache | 46 | 28.57 |
| Eyestrain | 3 | 1.86 |
| Pain in/around the eye | 7 | 4.35 |
| Diplopia/Polyopia | 1 | 0.62 |
| Watering | 6 | 3.73 |
It was observed that only 17 children with myopia, 1 with hypermetropia and 5 with astigmatism were using spectacle, i.e., total 23(14.29%) were using spectacle [Table/Fig-7].
Refractive errors and history of (H/O) wearing spectacles.
| Refractive errors | H/O wearing spectacles | No. H/O wearing spectacles | Total |
|---|
| Myopia | 17 | 78 | 95 (59.01%) |
| Hypermetropia | 1 | 22 | 23 (14.29%) |
| Astigmatism | 5 | 38 | 43 (26.71%) |
| Total | 23 (14.29%) | 138 (85.71%) | 161 (100%) |
| χ2-value | 6.22, p-value=0.044, Significant |
Discussion
There is a massive ice berg of refractive errors and colourblindness in present study population. Most of the children in the study group were in the range of twelve to fifteen years (40.69%). This is similar to study by Saha M et al., [19]. Among all the study participants, maximum patients did not have a refractive error. Only 18.61% of children had a refractive error. Seema S et al., conducted a study in Haryana where prevalence of refractive error in 6-15-year-old was 13.65% and Singh V et al., in West Uttar Pradesh observed 17.36% prevalence the results of which were similar to the current study [20,21]. Among a total of 161 children diagnosed with refractive error, maximum children had myopia (59.01%) followed by astigmatism (26.71%), and the least number of children had hypermetropia (14.29%). Studies which shows the different pattern of refractive errors is tabulated in [Table/Fig-8] [22-28].
Comparison of pattern of refractive errors in various studies [22-28].
| Name of the study | Myopia | Hypermetropia | Astigmatism |
|---|
| Present study | 59.01% | 14.29% | 26.71% |
| Sarma KD et al., [22] | 81.92% | 3.91%). | 14.89% |
| Pavithra MB et al., [23] | 62.9% | 14.4% | 22.7% |
| Sethi S and Kartha GP [24] | 63.5% | 11.2% | 20.4% |
| Ali ABM et al., [25] | 53% | 9.3% | 22.9% |
| Warad C et al., [26] | 82.67% | 9.3%, | 7.9% |
| Kawuma M and Mayeku R [27] | 11% | 37% | 52% |
| Chatterjee S et al., [28] | 58.2 | 17.7% | 16.3% |
| Samant PL et al., [29] | 78.57% | 21.43% | - |
The number of cases of refractive errors increased with advancing age. Myopia was the most predominant type of refractive error in all the age groups. Patil M et al., reported that maximum refractive error was in age group of 10-12 years [30]. Singh H, found it most commonly in the age group of 8-10 years [31] and Padhye AS et al., found them in 9-12 years [32]. Sun JT et al., found in their study that the prevalence of myopia in children increased with increasing age and that girls were no more likely to suffer from myopia than boys [33]. Theophanous C et al., concluded that the prevalence of myopia increased with age [34]. These results are comparable to present study.
There was no significant association between gender and refractive error according to present study. In a study by Patil M et al., also no significant association was found between refractive errors and sex, also it was found that 94% of children had no visual impairment [30]. In a similar study in central India by Singh H, 28.78% of children had Visual aquity between 6/24 to 6/60 and 5.67% had <6/60 [31]. The results of these studies are in agrrement with the current study. Majority of the children with refractive errors in current study were not wearing spectacles (85.71%). Sarma KD and Krishantreya M, observed 75.53 % of cases of ammetropia were detected during the study, out of which only 24.47% were already wearing spectacles [22]. Prema N in the study noted that only 7% of students with poor vision used eyeglasses [35].
It was observed in present study that 1.62% of children had colour blindness. Among protans, 1.045 % were male, and 0.35% were females. Among deutans 0.23 % were male children. Reddy AV et al., conducted a study in Guntur, Andhra Pradesh and concluded that the prevalence of colour blindness was 1.9% out of which 1.71% were males and 0.184% females. Among them, 90.3% were protanopes, 9.7% were deuteranopes, and none were tritanope [36]. According to Agrawal S and Bansod N, 2.02% were colour blind which includes 11 boys (3.16%) and 1 girl (0.40%) and out of them 2.87% of boys had deuteranomaly, and one boy (0.29%) showed protanomaly [37]. These results are similar to present study.
Limitation(s)
In present study right, and left eyes are not being compared separately. Present study is a cross-sectional one, hence determination of temporal associations among various variables in the study was not done. Only protanopes and deuteranopes was identified by Ishihara chart. Amblyopia and squint can be associated with refractive error, but these are not included in the study. It is a school-based survey and only six schools were surveyed. Hence study should also be undertaken on a larger scale in future.
Conclusion(s)
It was concluded that inspite of being an urban area with good literacy rate and maximum population belonging to class I socioeconomic status, 61% of students with refractive error out of which 85.71% were not using spectacles and 2.48% were even categorised as blind. This is alarming as refractive error is a treatable cause of blindness. This can be accounted on the lack of awareness regarding symptoms of refractive error and importance of early diagnosis and treatment.
Value of χ2: 29.49; p-value: 0.0001; Significant
Value of χ2: 4.07; p-value: 0.13; Not Significant