Uretero-pelvic Junction Obstruction and Posterior Urethral Valve Diagnosed with Contra Lateral Multicystic Dysplastic Kidney: Association Unveiled
Amit Kumar Sinha1, Amit Kumar2, Rashi3, Bindey Kumar4, Prem Kumar5
1 Assistant Professor, Department of Paediatric Surgery, All India Institute of Medical Sciences, Patna, Bihar, India.
2 Senior Resident, Department of Paediatric Surgery, All India Institute of Medical Sciences, Patna, Bihar, India.
3 Senior Resident, Department of Paediatric Surgery, All India Institute of Medical Sciences, Patna, Bihar, India.
4 Professor and Head, Department of Paediatric Surgery, All India Institute of Medical Sciences, Patna, Bihar, India.
5 Professor and Head, Department of Radiology, All India Institute of Medical Sciences, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Amit Kumar Sinha, Department of Paediatric Surgery, AIIMS Patna, Patna, Bihar, India.
E-mail: dr_amits@yahoo.com
Paediatric obstructive uropathy is defined as any congenital obstruction in the urinary tract severing renal function to any extent. More frequent causes in male counterpart include posterior urethral valve and uretero-pelvic junction obstruction. Multicystic dysplasia of kidney, on the other hand, is an enlarged kidney almost completely replaced by multiple non-communicating cysts. The association of these three entities in the same child could prove fatal and very rare. The article is on the clinical trajectory of a four-year-old male child reporting with these three conditions and the stepwise protocol followed in the management.
Cystic disease of kidney, Hydronephrosis, Obstructive uropathy, Paediatric
Case Report
A four-year-old boy reported to the Paediatric medicine outdoor with hematuria and peri-orbital swelling, for 2 months. On the day of OPD visit, patient had urinary retention and hence furthered for evaluation by Paediatric surgeon.
On Paediatric surgery evaluation, patient had gross abdominal distension with mild suprapubic tenderness. He was admitted and catheterised per urethrally and urine output was @1.8 mL/kg/hr, to start with. Routine blood sampling suggested metabolic acidosis, hyperkalemia and anaemia. Necessary corrections for metabolic acidosis and hyperkalemia were done with sodium bicarbonate, nebulisation with beta-2 agonist, calcium supplements and chelating agents. ACE inhibitors and uroprophylaxis were also started.
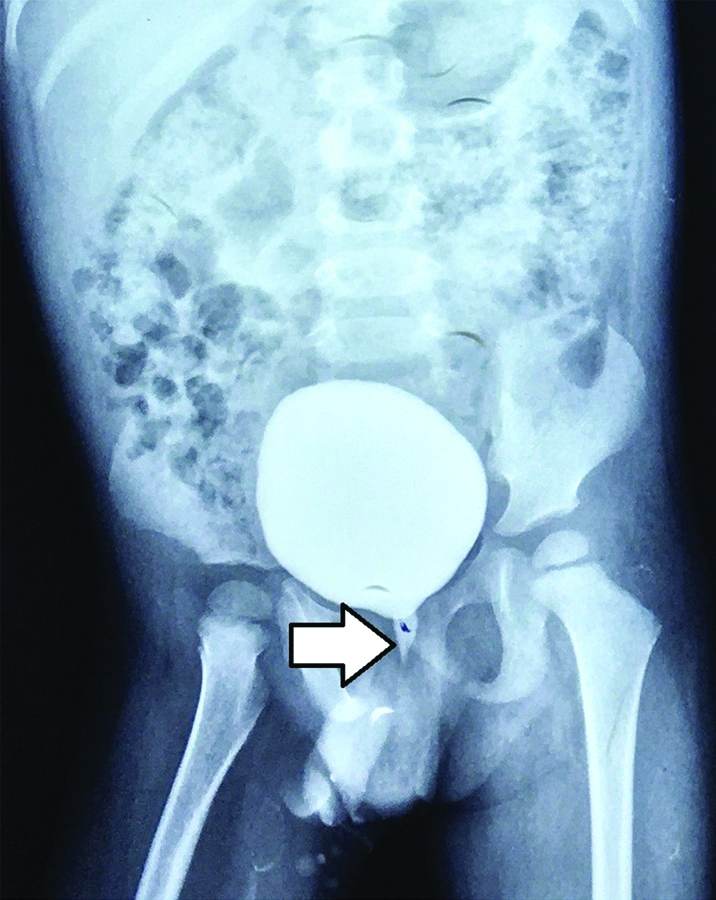
Patient stabilised gradually, but with urine output @4.5 mL/kg/hr and remained polyphagic too. Blood urea/creatinine fell from 130/3.48 (mg/dL) to 92/1.87 (mg/dL) after catheterisation. Initial ultrasonic scans suggested bilateral gross hydronephrosis. Voiding Cystourethrogram (VCUG) revealed dilated posterior urethra [Table/Fig-1]. Cystoscopy confirmed posterior urethral valve at 12’o clock position and fulguration was performed.
Voiding cystourethrogram (VCUG) showing dilated posterior urethra).
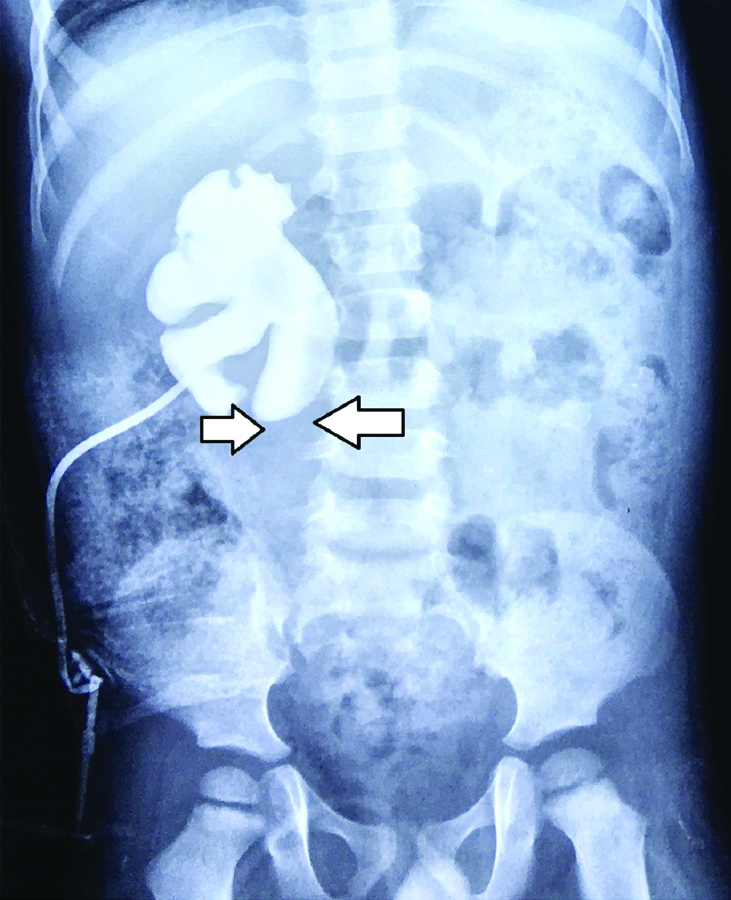
Post-fulguration, patient passed urine in normal stream. After 15 days, he again developed increasing abdominal distention and dysuria. Review Ultrasound suggested right side uretero-pelvic junction obstruction and left side multicystic dysplastic kidney. Owing to the static blood urea/creatinine levels, a right-sided percutaneous nephrostomy was planned and a nephrogram through the catheter, thus, further confirmed the obstruction [Table/Fig-2].
Percutaneous nephrostogram showing obstructed drainage at Uretero-pelvic junction.
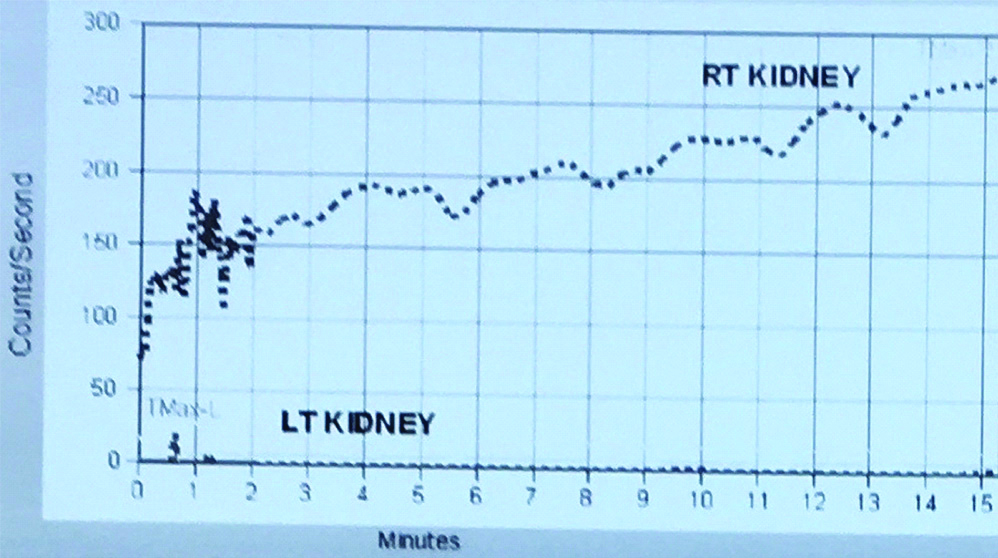
Gradually, on conservative management, anaemia settled but blood urea/creatinine levels did not decrease below 65/1.28(mg/dL). Dimercaptosuccinic Acid (DMSA) scan showed non-visualised non-functioning left kidney and normal cortical function of right kidney with no evidence of focal pyelonephritis or scar. Diethylene Triamine Pentacetic Acid (DTPA) scan suggested non-functioning left kidney with 0% differential function and right side hydronephrotic kidney with pelviureteric junction obstruction [Table/Fig-3]. Glomerular filtration rate of right kidney reduced to 65.5 mL/min and for that decision of open-modified Anderson Hyne’s pyeloplasty was taken, with J-J stent and percutaneous pigtail catheter and per-urethral catheter, put in-situ. Non-functioning multicystic dysplastic left kidney as planned for conservative follow-up.
DTPA scan suggesting non-functioning left kidney and right-sided uretero-pelvic junction obstruction).
Postoperatively, after sequential antigravity drainage from percutaneous catheter and ensuring forward flow from perurethral catheter, pigtail catheter was removed on day 7, followed by perurethral catheter on day 8. Patient was discharged in sound condition. Histopathology of the specimen confirmed features of uretero-pelvic junction obstruction. Double J stent was removed cystoscopically after 4 weeks. Patient discharged in stable condition and kept on regular 3 monthly follow-up.
Discussion
Obstructive uropathy includes lesions of the urinary system impeding urinary flow to a magnitude, causing renal impairment [1]. Among Paediatric males, common causes are posterior urethral valve and uretero-pelvic junction obstruction. Posterior urethral valves are a common anomaly, affecting males predominantly and can lead to poor urinary stream and refluxing ureters, causing back pressure changes on bladder, kidneys and ureters. These valves get best delineated on voiding cystourethrogram [2]. Uretero-pelvic junction obstruction is the most common cause of antenatal hydronephrosis, affecting mostly the males and that too, on the left side [3].
Technetium-99m L, L- ethylene dicysteine isotope scan or diethylene triamine penta acetic acid scan most definitely diagnoses the condition, till date [4]. Following the definitive indication for surgery, Transurethral cystoscopic fulguration of valves or pyeloplasty for the latter condition is the standard treatment. The clinical course gets entangled by the compromised contralateral renal function, if any.
Congenital conditions leading to obstructive uropathy are due to malformations during development of urogenitals. Human kidneys, proximal tubule, loop of Henle and convoluted tubule evolve from metanephric blastema. While Wolffian duct gives rise to collecting tubules, till ureter. Urinary bladder develops from vesico-urethral canal as well as cranial part of uro-genital sinus. Male urethra is derived from caudal part of urogenital sinus and a part from endodermal cells of the urethral plate. Aberrations in genetic, epigenetic or environmental signals may influence the events, at any stage [5-7].
The uretero-pelvic junction is the last to recanalise amongst the upper urinary tract and its hindrance leads to congenital variety of uretero-pelvic junction obstruction. Another significant event during embryogenesis is the presence of one way valves at the level of verumontanum, since 7 weeks of gestation and is thought to be a vestige of the Mullerian duct. On the other hand, renal dysplasia is featured by malformation of tissue elements with or without cysts. Multicystic dysplastic kidney is the most severe, in the group, characterised by large, cystic, non-functional mass in the renal fossa [8].
Conclusion(s)
After searching and reviewing the literature, we found that the association of uretero-pelvic obstruction, posterior urethral valve and multicystic dysplastic kidney in a single patient is not reported till date. Knowing the association between different uro-genital disorders and a deep knowledge of the pathogenesis would definitely help in better and timely intervention. In the index case, we found a fatal association of three conditions with a quite sound clinical recovery.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? NA
Was informed consent obtained from the subjects involved in the study? Yes (from parents)
For any images presented appropriate consent has been obtained from the subjects. Yes (from parents)
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 02, 2019
Manual Googling: Jan 22, 2020
iThenticate Software: Feb 17, 2020 (11%)
[1]. Liu DB, Armstrong 3rd WR, Maizels M, Hydronephrosis: Prenatal and postnatal evaluation and managementClin Perinatol 2014 41(3):661-78.10.1016/j.clp.2014.05.01325155734 [Google Scholar] [CrossRef] [PubMed]
[2]. Heikkila J, Holmberg C, Kyllonen L, Rintala R, Taskinen S, Long-term risk of end stage renal disease in patients with posterior urethral valvesJ Urol 2011 186(6):2392-96.10.1016/j.juro.2011.07.10922014822 [Google Scholar] [CrossRef] [PubMed]
[3]. Sahay M, Congenital anomalies of kidney and urinary tractClinical Queries: Nephrology 2013 2(4):156-65.10.1016/j.cqn.2013.11.005 [Google Scholar] [CrossRef]
[4]. Gordon I, Piepsz A, Sixt R, Guidelines for standard and diuretic renogram in childrenEur J Nucl Med Mol Imaging 2011 38(6):1175-88.10.1007/s00259-011-1811-321503762 [Google Scholar] [CrossRef] [PubMed]
[5]. Pradhan M, Singh N, Singh AK, Kumari N, Rare association of fetal posterior urethral valve with ureteric strictureJ Prenat Med 2012 6(1):01-03. [Google Scholar]
[6]. Chowdhary SK, Obstructive uropathy in newbornsApollo Medicine 2007 4(2):98-102.10.1016/S0976-0016(11)60115-4 [Google Scholar] [CrossRef]
[7]. Langstaff CHF, Mallik M, Antenatally detected urinary tract abnormalities (AUTA)Paediatrics and Child Health 2014 24(7):303-10.10.1016/j.paed.2014.01.010 [Google Scholar] [CrossRef]
[8]. Hains DS, Bates CM, Ingraham S, Schwaderer AL, Management and etiology of the unilateral multicystic dysplastic kidney: A reviewPediatr Nephrol 2009 24(2):233-41.10.1007/s00467-008-0828-818481111 [Google Scholar] [CrossRef] [PubMed]