Case Report
A 50-year-old lady came to the casualty with complaints of pain in left hypochondrium region, since 8 days. There was no history of any chronic illness (diabetes mellitus, hypertension, bronchial asthma) neither she had any similar complaints in the past. There was no history of any similar complaints or chronic illness in the family members.
On examination, tenderness was present in left hypochondrium region along with splenomegaly (2 cm below the left costal margin). Ultrasonography (USG) abdomen-pelvis showed cystic intra-splenic mass lesion, suggestive of abscess of size 12.5 cm × 9 cm × 6.9 cm with a volume of 570 mL. Patient underwent routine blood investigation (Complete Blood Count, Kidney Function Test, Liver Function Test, Random Blood Sugar) which showed raised Whole Blood Count (WBC) (22600 cells/mm3) and raised Random Blood Sugar (RBS) (254 mg%).
Since the USG showed splenic abscess, antibiotics were started-Injection (inj) ceftriaxone 50 mg/kg/body weight Intravenously (I.V) in 2 dividing doses for 7 days, Inj Metronidazole 35 mg/kg/body weight I.V. in 3 dividing doses for 7 days, Inj Amikacin 15 mg/kg body weight once daily for 5 days. Along with antibiotics, she was started on Inj Insulin Regular with 4 hourly Random Blood Sugar charting for 4 days and was then shifted to oral hypoglycaemic drug (tab. Gepride M1 in two dividing doses). USG guided percutaneous drainage of the abscess was done on 2nd day of the admission. Around 520 mL of dark brown colour pus mixed with blood was drained. Pus was sent for culture and sensitivity, which revealed no growth.
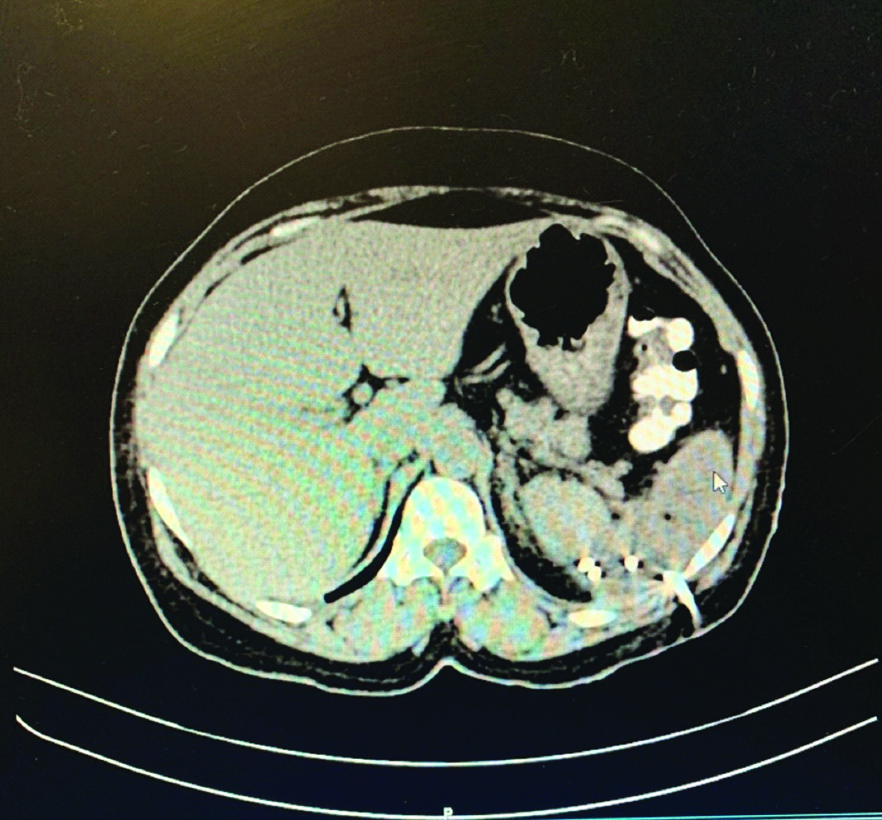
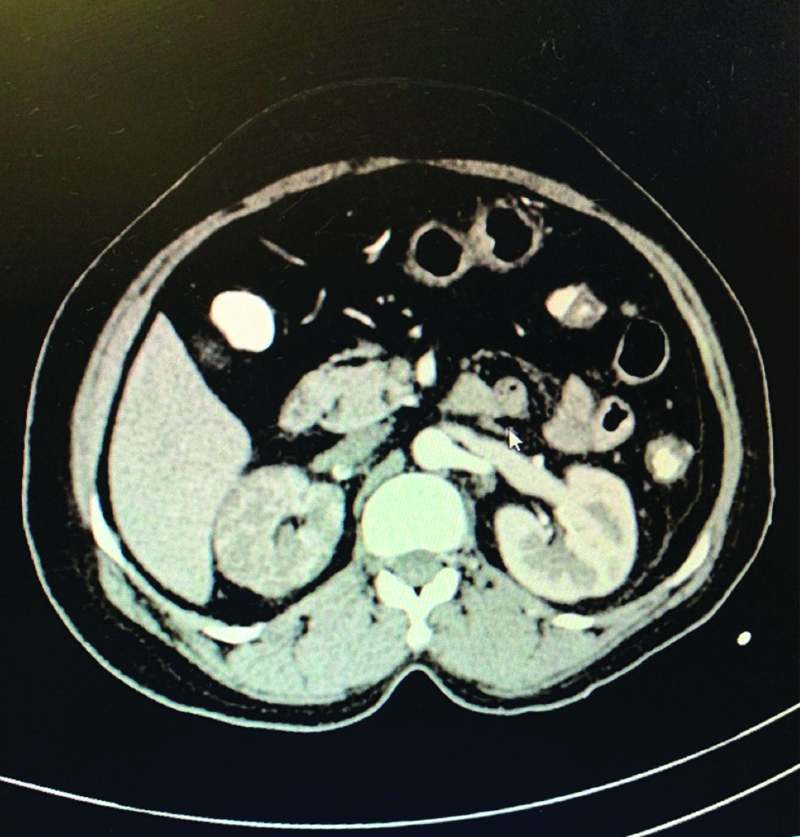
Contrast Enhanced Computed Tomography (CECT) abdomen pelvis was done on the 3rd day of admission, which showed splenic abscess with drainage catheter in-situ along with thrombosis in abdominal aorta involving the right renal artery causing renal infarcts [Table/Fig-1,2].
CE-CT abdomen and pelvis showing splenic abscess with percutaneous drainage in-situ.
Contrast Enhanced Computed Tomography (CECT) abdomen and pelvis showing no blood flow to the right kidney.
The patient was clinically evaluated for peripheral pulsation and was found that there was absent right-sided popliteal artery; anterior tibial artery, posterior tibial artery and dorsalis pedis artery pulsation, but pulsation were present on contr-alateral limb and both upper limbs. Colour Doppler of Bilateral lower limb was done on 3rd day of admission, which was suggestive of acute thrombotic occlusion of right distal femoral artery and popliteal artery. There was no flow in anterior tibial artery, posterior tibial artery and dorsalis pedis artery on the right lower limb. She underwent 2D echocardiography on 3rd day of admission, which showed mild degenerative changes in aortic valve with mild aortic regurgitation. Prothrombin time was done {pt (INR)-12.6 sec (1.01)}.
She was started on Inj heparin 0.6 mg subcutaneously along with tab. Ecosprin 150 mg once daily and tab. Atroin 40 mg at night on 3rd day of admission and was continued for next 2 days. After 2 days, she was shifted on oral anti-coagulant therapy (tab. Acitron 1.5 mg once daily) with alternate day monitoring of Prothrombin Time which was done for next 5 days.
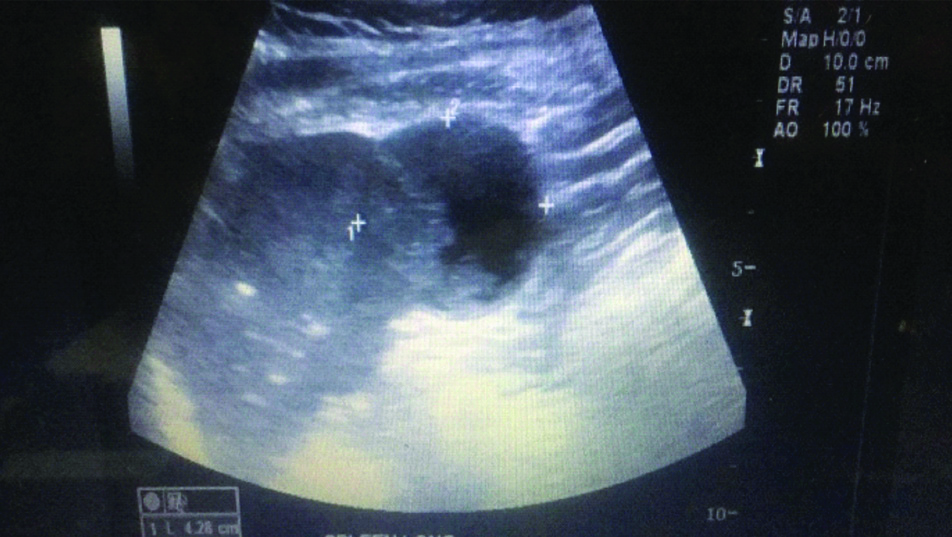
USG Abdomen and Pelvis was repeated on 10th day of admission which revealed minimal residual collection noted in the splenic abscess site [Table/Fig-3], so it was advised to remove percutaneous drainage.
USG abdomen and pelvis showing heterogenous hypoechoic resolving lesion of size 4×3 cm in Spleen.
On 17th day of admission, a repeat USG abdomen and pelvis was advised which was suggestive of healed abscess in spleen. Right kidney showed maintained vascularity and no thrombosis was noted in the aorta.
Patient was discharged on oral antibiotics (tab. cefixime 200 mg in 2 dividing doses for 7 days) and oral anticoagulant therapy (tab. Acitron 1.5 mg once daily to be continued) along with oral hypoglycaemic drugs (tab. Gepride M1 in two dividing doses to be continued) and antiplatelet drugs (tab. Ecosprin 150 mg once daily was continued). After 15 days, patients came for a routine follow-up and had no complaints and were advised to continue with oral hypoglycaemic drugs (tab. Gepride M1 in two dividing doses to be continued).
Discussion
Spleen has a vital role in the immunologic function; hence splenectomised patients have a higher incidence of infections and post-operative morbidity [1].
Splenic abscess is an uncommon entity. The incidence of splenic abscess is estimated to be 0.1-0.7%. Though it is uncommon, has been increasingly diagnosed as the reasons are increased number of immuno-compromised patients and better imaging techniques [2].
Splenic abscess mostly spread through hematogenous route. Risk group includes patients with septic endocarditis, septicaemia, immuno-suppressed individuals (e.g., HIV, malignancy, and diabetes mellitus), trauma, infections with contagious spread etc. [2]. In the present case scenario, splenic abscess was associated with Type 2 diabetes mellitus as a co-morbidity. In a case study done by Chen H et al., a 55-year-old male patient who was diagnosed with case of splenic abscess and was suffering from Type 2 diabetes mellitus. This study was similar to the present study [3].
Ultrasound and CT scan of the abdomen are the major radiological modalities used in the diagnosis. The investigation of choice for splenic abscess is CT scan. CT scans are helpful in revealing loculations of the abscess cavity along with the nature of its contents. It may be used to differentiate splenic abscesses from splenic cysts and haematomas. Ultrasound also has a comparable accuracy in detection of the same. Additionally, the location of abscess, relation of spleen to other visceral structures are delineated which helps in performing percutaneous drainage [4].
Clinical awareness is mandatory to diagnose and treat splenic abscess. Only one half of the patients in one series and 32% of the cases in another series reported the classic findings of fever, chills, tenderness in the left upper quadrant along with splenomegaly. The involvement of spleen occurs by beginning of second week. Varied manifestations of these old classic lesions should not be missed while examining the case. A thorough microbiological examination is necessary in such pyogenic lesions [5].
In the present case, scenario patient had complaint of left hypochondrium pain along with raised count (22600 cells/mm3) and was diagnosed as splenic abscess on ultrasonography of abdomen which showed cystic intra-splenic mass lesion suggestive of abscess of size 12.5 cm × 9 cm × 6.9 cm with a volume of 570 mL.
In a case report done by Chen H et al., a 55-year-old male patient who came with complaint of left epigastric dull pain along with chills and fever and with raised WBC count (17000 cells/mm3) had undergone CECT abdomen which showed splenic abscess with inflammatory exudates and spleen calcification [3]. In a case reported by Gupta S et al., a 42-year-old male patient came with complaint of left hypochondrial dull pain along with chills and fever and with raised WBC count (13400 cells/mm3); had undergone USG Abdomen and pelvis which showed large hypoechoic collection measuring 15 cm × 12 cm in diameter with shaggy borders, suggestive of splenic abscess [6].
Most common organisms obtained from culture of the abscesses are aerobic microbes, in particular, Staphylococci, Streptococci, Salmonella, and Escherichia coli. However, it seems to have geographical variations and population difference. Fungal and protozoal splenic abscesses have been seen in immuno-compromised cases [2]. In the present case scenario, culture was found to be negative because patient was started on antibiotics at the time of admission. In a case report by McOwat L et al., a 78-year-old female was diagnosed with splenic abscess and whose pus culture has growth of Staphylococcus aureus which was sensitive two flucloxacillin, tetracycline and clarithromycin [7].
Intravenous antimicrobial therapy, CT-guided percutaneous aspiration and splenectomy are few treatment modalities followed for treating splenic abscesses. The success rate of antimicrobial therapy in case of splenic abscess is 70.8%-100%. The small and multiple abscesses respond better to intravenous antimicrobial therapy alone [4]. The combination of ceftriaxone with metronidazole is the most common empirical antimicrobial treatment used. Splenectomy has been the most effective and definitive procedure for managing splenic abscesses. In the present case study, splenic abscess was unilocular hence percutaneous drainage was performed. In a case study done by Hai Chen MD et al., a 55-year-old male patient of splenic abscess had multiple divergent pus cavities on CECT abdomen, so was planned for splenectomy [3].
The common complications associated with splenectomy are lung infection, wound infection, septicaemia, paralytic ileus and deep vein thrombosis [4,8]. A significant complication post-splenectomy is an infection by encapsulated organisms like StreptococcusPneumonia, Neisseria meningitidis and Haemophilus Influenzae Type B [8]. The location of the abscess becomes vital as percutaneous drainage may be suited for peripherally situated abscesses, patients who are critically ill or are unfit for general anaesthesia. The drainage is performed with ultrasound or CT guidance using 8-French to 20-French catheters. The insertion of these catheters may be accompanied by spontaneous drainage of the pus. Lack of abdominal spillage, lesser costs, better acceptance and avoidance of the operative risks are few other advantages of drainage procedures. Certain multiple or septated abscesses, anatomically inaccessible abscesses, coagulopathies, ascites or associated diseases requiring surgical procedures are few contra-indications to percutaneous drainage. Poor drainage mandates radiological verification of the tube location and position. Haemorrhage, septicaemia, injury, empyema, pneumothorax and fistula are few complications associated with percutaneous drainage [4,9]. Nandwani A et al., presented a case with membranous nephropathy in remission and with severe abdominal pain [10]. The importance of present case scenario is that the patient was diagnosed with splenic abscess along with thrombosis of abdominal aorta and thrombosis of right renal artery with complete infarction of right kidney. This case is rare because, in spite of meticulous search of various medical portals online (PubMed, Google etc.,) for similar case scenarios, none could be found which matches to this presentation.
Conclusion(s)
Based on the present case of splenic abscess with aortic and right renal artery thrombosis, which was treated by percutaneous drainage along with antibiotics and anticoagulants; the present authors conclude that for unilocular splenic abscess, percutaneous drainage can be considered as an ideal treatment modality. As discussed above, that CT scan is the investigation of choice for splenic abscess, as it can also unveil the other associations with splenic abscess like in the present case, it revealed the presence of aortic thrombosis and right renal artery thrombosis. This helped us in early management of the thrombus in both major arteries thereby helping us prevent its likely consequences. The aortic and renal thrombus were managed conservatively using anticoagulants and antiplatelets. Though being a rare unique presentation with likelihood of deadly consequences, a satisfactory outcome was achieved in the present case with minimal intervention and medical management.
[1]. Princess D, Francisco DM, Trivedi A, O’Loughlin MO, Wu GY, Vascular diseases of spleen: A reviewJCTH 2017 5(2):152-64. [Google Scholar]
[2]. Sreekar H, Saraf V, Pangi AC, Sreehasha H, Reddy R, Kamat G, A retrospective study of 75 cases of splenic abscessIndian J Surg 2011 73(6):398-402.10.1007/s12262-011-0370-y23204694 [Google Scholar] [CrossRef] [PubMed]
[3]. Chen H, Hu ZQ, Fang Y, Lu XX, Li LD, Li YL, A case report: Splenic abscess caused by Burkholderia pseudomalleiMedicine (baltimore) 2018 97(26):e1120810.1097/MD.000000000001120829952975 [Google Scholar] [CrossRef] [PubMed]
[4]. Lee M-C, Lee C-M, Splenic Abscess: An uncommon entity with potentially life threatening evolutionCan J Infect Dis Med Microbiol 2018 2018:8610657:1-6.10.1155/2018/861065729666665 [Google Scholar] [CrossRef] [PubMed]
[5]. Bhongle NN, Nagdeo NV, Thombare VR, A splenic abscess which was caused by salmonella typhi in a non sickler patient: A rare case findingJ Clin Diagn Res 2013 7(3):537-38.10.7860/JCDR/2013/4563.281623634415 [Google Scholar] [CrossRef] [PubMed]
[6]. Gupta S, Singh O, Hastir A, Shukla S, Mathur RK, Splenic Abscesses: Reports of two cases with review of literatureAnn Trop Med Public Health 2012 5(3):273-77.10.4103/1755-6783.98638 [Google Scholar] [CrossRef]
[7]. McOwat L, Wong KF, Varughese GI, Nayak AU, Splenic abscess as a potential initial manifestation of quiescent infective endocarditis in a patient with bronchopneumoniaBMJ Case Rep 2015 2015:bcr201420679410.1136/bcr-2014-20679425564586 [Google Scholar] [CrossRef] [PubMed]
[8]. Cadili A, de Gara C, Complications of SplenectomyAm J Med 2008 121(5):371-75.10.1016/j.amjmed.2008.02.01418456028 [Google Scholar] [CrossRef] [PubMed]
[9]. Ferraioli G, Brunetti E, Gulizia R, Mariani G, Marone P, Filice C, Management of splenic abscess: Report on 16 cases from a single centerInt J Infect Dis 2009 13(4):524-30.10.1016/j.ijid.2008.08.02419070526 [Google Scholar] [CrossRef] [PubMed]
[10]. Nandwani A, Pathania D, Jha PK, Kher V, Renal artery thrombosis with renal infarction: A rare cause of acute abdomenIndian J Nephrol 2017 27(4):313-15.10.4103/0971-4065.18358128761235 [Google Scholar] [CrossRef] [PubMed]