An Intriguing Case of Infrarenal Aortic Hypoplasia
Dilip Vincent1, Rohini Avantsa2, Kabekkodu Venkata Tejaswi3
1 Junior Resident, Department of Radiodiagnosis, K S Hegde Medical Academy, Mangalore, Karnataka, India.
2 Associate Professor, Department of Radiodiagnosis, K S Hegde Medical Academy, Mangalore, Karnataka, India.
3 Senior Resident, Department of Radiodiagnosis, K S Hegde Medical Academy, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dilip Vincent, K S Hegde Medical Academy, Mangalore-575018, Karnataka, India.
E-mail: dilip.vincent007@gmail.com
Infrarenal aortic hypoplasia is a very rare anomaly of the vascular tree characterised by diffuse stenosis of the infrarenal abdominal aorta. The pathogenesis of this condition seems to be unclear despite the advancements of vascular surgery. In general, the most common presenting symptom is claudication occurring in 3rd to 4th decade of life. Here, a rare and interesting case of infrarenal aortic hypoplasia is reported in a 32 year-old female patient who presented with a history of low backache and bilateral intermittent lower extremity claudication. Using Doppler ultrasonography and computed tomographic angiography, we could demonstrate the abrupt termination of the infrarenal aorta with collateral reformation.
Abdominal aortic hypoplasia, Aortic coarctation, Intermittent claudication
Case Report
A 32-year-old woman presented with a long standing history (13 years) of lower backache and intermittent claudication of bilateral lower limbs which aggravated on walking and while performing strenuous activities. She was not diagnosed of any congenital anomalies at the time of birth. The patient was asymptomatic till 19 years of age. Then gradually she developed the above mentioned symptoms. There has been no significant progression in these symptoms ever since its onset. Therefore, she was symptomatically managed for the past 13 years.
On examination, both the lower limbs were of normal length, the blood pressure on the lower limbs were reduced with an Ankle-brachial index of 0.5. Bilateral dorsalis pedis, anterior tibial and posterior tibial arteries demonstrated feeble pulses. The renal function tests were normal. There was no demonstrable bruit/ murmurs in the chest and abdomen. There was no evidence of any dilated tortuous veins over the skin of her abdomen. The patient was referred to the radiology department for further evaluation. Ultrasonography of abdomen and pelvis followed by CT angiography were performed.
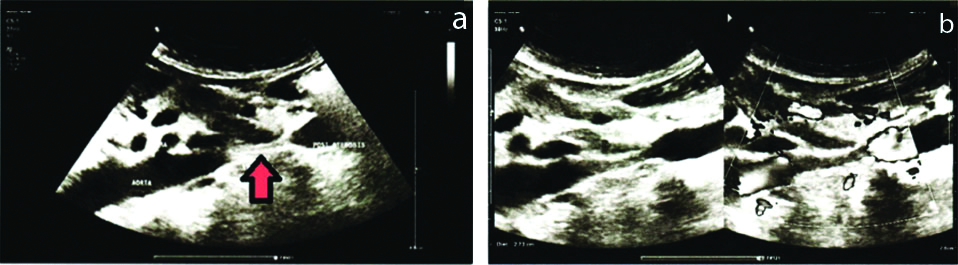
Ultrasonography revealed near-total obstruction in the infrarenal segment of abdominal aorta for a length of 27 mm with post- stenotic segment showing recanalised flow [Table/Fig-1]. The maximum transverse diameters of the pre-stenotic and post-stenotic segments were 10 mm and 12 mm, respectively. The recanalised post-stenotic segment showed increased velocity of blood flow. Both the kidneys showed normal size, echotexture and vascularity. Celiac trunk, superior mesenteric arteries and bilateral iliac arteries showed normal calibre and vascularity on Doppler evaluation.
(a) Ultrasound image in the midsagittal section shows the level of luminal stenosis (arrow) and the area of hypoplasia. (b) Colour Doppler image showing no colour uptake at the level of stenosis.
On CT angiography, there was a short segment (2.8 cm) non -opacification of the infra-renal aorta at the level of L2 vertebral body [Table/Fig-2]. The distal segment was reformed by several collaterals arteries, such as superior mesenteric and inferior mesenteric artery anastomoses, prominent marginal artery of Drummond. Both the renal arteries were intact. The peripheral angiography showed normal course and opacification of the distal arteries.
(a) Computed tomographic angiography revealed abrupt occlusion of a short segment of infrarenal aorta (white arrow) and the distal reformed aorta (red arrow). Bilateral renal arteries were normal and intact. (b) The flow to the distal segment was reformed by several collaterals arteries. (c,d) MPR reconstructed images showing the site of occlusion of abdominal aorta, the normal lumen is replaced by thin hypodense fibrotic band (red arrow).

As there was no progression in symptoms and there was no radiological evidence of renal artery involvement or progression of the disease in the follow-up scans, surgery was not advised. She was treated conservatively by symptomatic management (Aspirin to relieve pain and other anti-claudication medication) and routine follow-ups were done for the past 13 years.
Discussion
Coarctation of the abdominal aorta is an extremely rare condition of unknown aetiology. The most likely causes may be infections such as congenital Rubella syndrome, autoimmune pancreatitis, anomalous development and fibromuscular dysplasias. Since this case presented at a younger age we considered congenital developmental anomalies as the most likely cause. The abdominal aorta is formed by the fusion of the paired primitive dorsal aortas during the first month of foetal life [1]. This process will be interrupted if there is an infection or inflammation in the prenatal life resulting in kinking and permanent constriction of the aorta. One of the most common prenatal infections for abdominal aortic stenosis include congenital Rubella infection. Alagille syndrome is an autosomal dominant disorder associated with congenital pulmonary artery stenosis has also been related to abdominal aortic coarctation [2]. Most common acquired causes of coarctation of the abdominal aorta include Takayasu’s arteritis, fibromuscular dysplasia and Behcet’s disease [1]. Blood studies did not show any signs of inflammation. Congenital aortic hypoplasia was considered as the most probable cause for the total absence of an aortic segment since there was no evidence of any inflammatory reaction.
Claudication is usually seen when there is infrarenal aortic hypoplasia. Visceral arteries are usually involved in about 20% of the cases. Mesenteric arterial ischemia is comparatively rare in such occasions because of sufficient collateral formation. Many patients present with a history of uncontrolled malignant hypertension, if there is associated renal artery stenosis [3]. Aortic coarctation is divided into four types based on its location. In type I, there is suprarenal coarctation and stenosis of the renal arteries; type II disease shows infrarenal coarctation with stenosis of renal artery; in type III there is only suprarenal aortic coarctation without any renal artery involvement; type IV, as in present case shows infrarenal coarctation of aorta without involving the renal artery [4]. The imaging modality of choice in delineating the level and extent of the disease is arteriography. Endovascular repair could not be performed in patient of the present study due to complete replacement of the vascular lumen with fibrotic band. So surgical management was only the available option. The usual surgical intervention for type IV coarctation is reconstruction of the abdominal aorta/grafting angioplasty.
Different terminologies used for occlusion of abdominal aorta are aortic stenosis, hypoplasia, coarctation and middle aortic syndrome. Coarctation is usually a congenital entity; the term “hypoplasia” is used when there is long-segment coarctation. If there is only narrowing of the aorta and various visceral arteries, then the term “Middle aortic syndrome” is used [1]. Present case showed complete absence of infrarenal aorta for a length of 2.8 cm, so it was described as hypoplasia.
Abdominal aortic hypoplasia usually presents based on the extent of stenosis, the branches that are involved (such as the renal and mesenteric arteries) and the amount of collateral reformations. If there is renal artery involvement there will be uncontrolled hypertension which was absent in the present case. Here the patient had a history of long-standing low backache and claudication of the lower extremities due to infrarenal aortic hypoplasia with insufficient collaterals. The imaging modalities used for assessing the location and extent of the disease are abdominal aortic angiography, ultrasound, CT or MRI. The average life expectancy of untreated patients is less [4]. By medical treatment, only symptomatic relief (claudication, pain) is attained. This patient did not have any progression of the disease, she was symptomatically treated for the past 13 years with aspirin and few other medications to relieve lower limb claudication.
Conclusion(s)
Hypoplastic infrarenal aorta is a very rare vascular anomaly with unknown aetiology. These patients usually present with minor symptoms since renal arteries are not involved. Even when there is no renal arterial involvement, hypertension might occur due to secondary atherosclerosis. Hence according to current day knowledge, surgical revascularisation is the best-known treatment regardless of the presumed aetiology.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 16, 2019
Manual Googling: Jan 10, 2020
iThenticate Software: Feb 12, 2020 (2%)
[1]. Sung SA, Hwang YH, Lee SY, Cho YK, Kwon TW, An infrarenal aortic hypoplasia presented with claudicationJ Korean Med Sci 2010 25(6):950-52.10.3346/jkms.2010.25.6.95020514320 [Google Scholar] [CrossRef] [PubMed]
[2]. Raas-Rothschild A, Shteyer E, Lerer I, Nir A, Granot E, Rein AJ, Jagged1 gene mutation for abdominal coarctation of the aorta in Alagille syndromeAm J Med Genet 2002 112(1):75-78.10.1002/ajmg.1065212239725 [Google Scholar] [CrossRef] [PubMed]
[3]. Stanley JC, Zelenock GB, Messina LM, Wakefield TW, Pediatric renovascular hypertension: A thirty-year experience of operative treatmentJ Vasc Surg 1995 21(2):212-26.10.1016/S0741-5214(95)70263-6 [Google Scholar] [CrossRef]
[4]. Fitzpatrick CM, Clouse WD, Eliason JL, Gage K, Podberesky DJ, Bush DM, Infrarenal aortic coarctation in a 15-year-old with claudicationJ Vasc Surg 2006 44(5):111710.1016/j.jvs.2005.07.04417098554 [Google Scholar] [CrossRef] [PubMed]