Hypoplastic Bone Marrow Failure in a Patient with Hereditary Persistence of Foetal Haemoglobin (HPFH) Trait
AK Kapoor1, S Maurya2, Geeta3
1 Pathologist, Department of Pathology, Vivekananda Polyclinic and Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
2 Director and Head, Department of Pathology, Vivekananda Polyclinic and Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
3 Technologist, Department of Pathology, Vivekananda Polyclinic and Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. AK Kapoor, Department of Pathology, Vivekananda Polyclinic and Institute of Medical Sciences, Nirala Nagar, Lucknow-226020, Uttar Pradesh, India.
E-mail: drashokkapoor2016@gmail.com
Hereditary Persistence of Foetal Haemoglobin (HPFH) trait is a rare genetic disorder and is caused by a large deletion involving δ and β globin genes. It is characterised by persistence of Foetal Haemoglobin (HbF) even in an adult. HbF level may vary from 2 to 30% in carriers of HPFH. Clinically, HPFH trait is asymptomatic without relevant haematological alterations. Mostly, HPFH trait is detected incidently while screening for other haemoglobinopathies. Herewith, we report a case of HPFH trait in our population. A 10-year-old boy born of non-consanguineous marriage complained of dyspnoea on exertion and dizziness. On examination he had generalised pallor. Earlier, he gave history of exposure to pesticides while spraying on crops. Later, he developed neutropenia (neutrophils 2000/mm3). He was immediately treated with piperacillin and gentamicin. Later, he was found to be severely anaemic (haemoglobin 3.0 gm/dL). His serum ferritin was within normal range. He also had severe thrombocytopenia (Platelets 10×109/L). Subsequently, Haemoglobin High Pressure Liquid Chromatography (Hb HPLC) was done. His chromatogram showed raised HbF concentration (5.8%) and borderline/or reduced HbA2 concentration (3.1%). He was finally diagnosed as a case of HPFH trait. He was given folic acid and 250 mL of the whole blood transfusion during his stay in hospital. Pesticide and/or insecticide might have caused severe hypoplastic anaemia. Moreover, piperacillin and gentamicin might have also contributed to thrombocytopenia. Detection of HPFH trait appeared to be important for its prevention in our region.
Hypoplastic anaemia, Pesticide exposure, Thrombocytopenia
Case Report
A 10-year-old male child complained of dyspnoea, effort intolerance and dizziness. He also had recurrent intermittent fever for last two weeks. The patient was a villager. He gave history of spraying of pesticides on crops, suggesting a case of child labour.
On examination, he had generalised pallor. He had vestibular vertigo probably due to ischemia. His absolute neutrophil count was low (2000 neutrophils/mm3).
Provisionally, he was suspected to have febrile neutropenia. He was treated with piperacillin and gentamicin. He was found to have severe normocytic anaemia. His MCV was 94 fL (normal 77-95 fL), MCH was 27 pg (normal 25-33 pg) and MCHC was 28% (normal 31-37%). However, his haemoglobin was 3.0 gm/dL (normal 11.5-15.5 gm/dL) and total RBC count was 1.17 million/mm3 (normal 4-5.2 million/mm3). Both serum iron (352 μg/dL) and serum transferrin saturation (146%) were raised. However, serum ferritin was within normal reference range (260 ng/dL). Later, in the hospital, total and differential leucocyte counts showed no change. Platelets were severely reduced in number (10×109/L), suggesting thrombocytopenia. Cation-exchange HPLC of different haemoglobins revealed raised HbF concentration (5.8%) and reduced/or borderline HbA2 concentration of 3.1% [Table/Fig-1a].
a) Shows results of haemoglobin HPLC in a patient with Hereditary Persistence of Fetal Haemoglobin (HPFH) trait. Extended mode shows HbF peak at retention time of 0.48 min; b) Chromatogram of uncle of above patient, aged 35 years shows a minor peak of HbF; c) Shows results of Hb chromatogram from a genetically unrelated subject. It showed a minor peak of HbF and reduced concentration of HbA2; d) Shows Hb chromatogram from an healthy subject with normal concentration of different haemoglobins.
x-axis: type of Hb; y-axis: amount of Hb
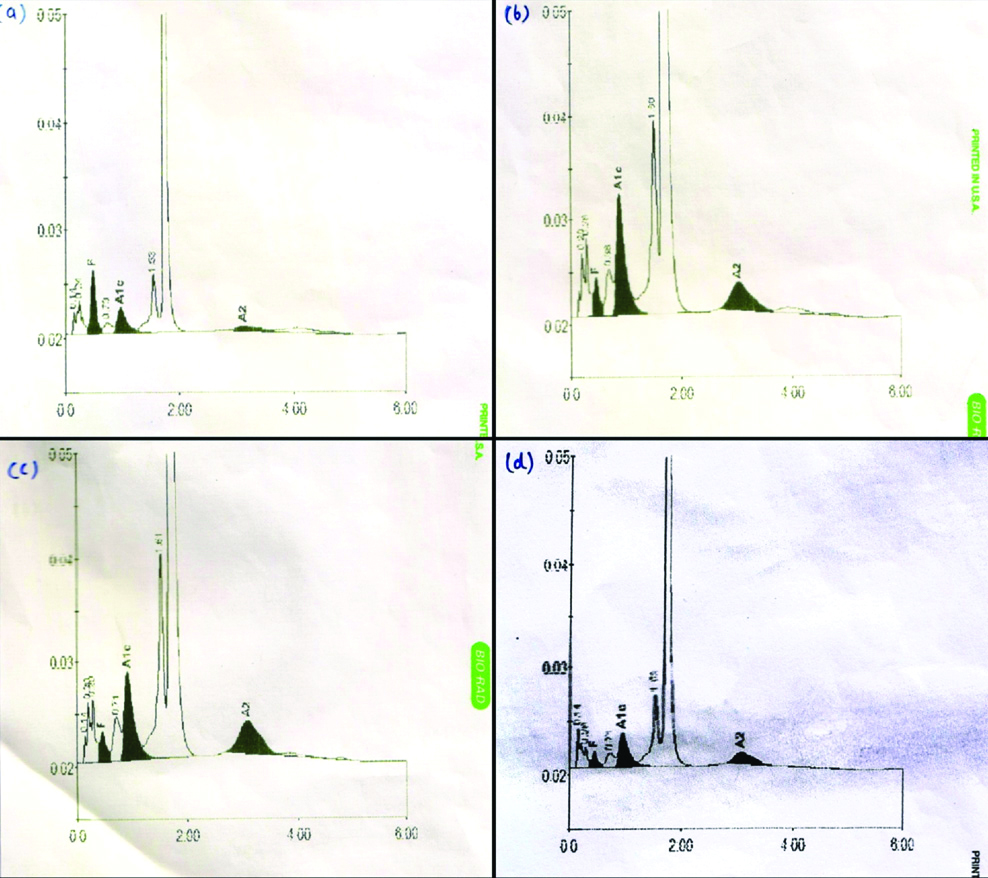
He was diagnosed as a case of HPFH trait. Hb HPLC examination was also done with blood of patient’s paternal uncle, he was aged 35 years and minimal HbF (<0.8%) was detected which appeared to be insignificant [Table/Fig-1b]. Blood samples of both the parents were not available. Therefore, it was decided to collect the blood of patient’s uncle. Later, Hb HPLC examination was done with a genetically unrelated subject with minimal HbF concentration [Table/Fig-1c]. Hb HPLC examination was also done with blood of an healthy subject with normal Hb concentration as a control [Table/Fig-1d]. Current patient was severely anaemic and also had severe thrombocytopenia. These observations suggested aplastic crisis. He was given whole blood transfusion (250 mL) once during his stay in hospital. It was interpreted that abnormal genes were inherited in the patient from one of the parents. The patient could not be followed further.
Discussion
HPFH trait is a rare, asymptomatic [1] genetic disorder where HbF persists even in an adult. It is incidentally discovered [2]. HPFH was first reported in 1955 from Ghana. Earlier, HPFH trait was detected in 5 of 5320 (0.09%) haemoglobinopathy cases in upper Assam region of North Eastern, India [3]. In another study, five cases of HPFH were detected in a family of Western Odisha with high HbF (26±3%) concentration [4]. In another study, four cases of HPFH were detected in a tribal city of Orissa [5].
Moreover, high levels of HbF were influenced by HPFH and Xmnl polymorphism [6]. Present case was suspected to have HPFH trait due to following reasons. First, he was aged 10 years. At this age, he had significant concentration of HbF and borderline/or reduced HbA2 concentration. Second, γ chain production resulted in significant HbF synthesis which almost completely compensated for the deficit of β and δ chains [7]. Third, the diagnosis of current case was further confirmed by Hb HPLC examination of blood of patient’s paternal uncle which showed minimal HbF production.
Hb chromatogram findings of current case were suggestive of a carrier state of HPFH. Severe anaemia and thrombocytopenia in current case suggested hypoplastic bone marrow failure. Aplastic crisis may occur following infection by B19 human parvovirus. The patient gave history of exposure to pesticide prior to present illness. Aplastic anaemia might have been caused by pesticide absorption through bronchial mucosa. However, cause of aplasia of bone marrow could not be ascertained. Long-term inhalation of toxic pesticides may produce severe haematotoxicity, resulting in increased incidence of hypoplastic bone marrow failure. Decreased expression of IL2, IL3 and IL5 receptors in pesticide- exposed marrow suggested suppression of cytokine activity in wistar rats [8]. Moreover, Mortein M may produce congestion, haemorrhage and hypocellularity of bone marrow [9] in wistar rats (Mortein M is a natural insecticide isolated from chrysanthemum).
In another study, significant decrease in in-vitro colony formation of haematopoietic progenitor cells was observed following exposure to pesticides (cypermethrin and mancozeb) [10]. Decrease in WBC and platelets as well as RBC, MCH and MCHC was observed in rats exposed to insecticidal oils from leaves of Cassia occidentalis and Euphorbia milli [11]. Similar decrease in RBC count and MCHC was observed in current patient following exposure to insecticide.
In addition, exposure to micromolar concentration of organophosphate and carbamate pesticides may affect pathophysiology of human bone marrow mesenchymal stem cells [12]. In another study, it was observed that exposure to certain organochlorine pesticides may lead to leucopenia [13]. Initially, current case was also treated with piperacillin and gentamicin; both drugs may cause thrombocytopenia [14,15]. Further, a patient with bone marrow failure may have raised HbF due to stressed haematopoiesis [1]. Moreover, inter-individual HbF variations appeared to be genetically controlled with mutations involving β globin gene complex [16].
Conclusion(s)
Correct diagnosis of a case of HPFH trait is important. In absence of a correct diagnosis, the patient may receive iron-supplements which may increase the iron overload. In present case, serum ferritin was within normal range. Farmers are advised to use mask, gloves and protective shoes prior to the use of pesticides.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 07, 2019
Manual Googling: Jan 22, 2020
iThenticate Software: Feb 12, 2020 (11%)
[1]. Natta CL, Niazi GA, Ford S, Bank A, Balanced globin chain synthesis in hereditary persistence of fetal hemoglobinJ Clin Invest 1974 54(2):433-38.10.1172/JCI1077794847253 [Google Scholar] [CrossRef] [PubMed]
[2]. Shaukat I, Pudal A, Yassin S, HÖti N, Mustafa S, Blessing in disguise: A case of hereditary persistence of fetal hemoglobinJ comm Hosp Intern Med Perspect 2018 8(6):380-81.10.1080/20009666.2018.153624130559951 [Google Scholar] [CrossRef] [PubMed]
[3]. Baruah MK, Saikia M, Baruah A, Pattern of hemoglobinopathies and thalassemias in upper Assam region of North Eastern India. High performance liquid chromatography studies in 9000 patientsInd J Path and Microbiol 2014 57(2):236-43.10.4103/0377-4929.13468024943756 [Google Scholar] [CrossRef] [PubMed]
[4]. Patel S, Dehury S, Purohit P, Meher S, Das K, Inheritance of Hereditary Persistence of Fetal Haemoglobin (HPFH) in a family of Western Odisha, IndiaJ Clin Diag Res 2015 9(9):OD09-10.10.7860/JCDR/2015/12878.654826500940 [Google Scholar] [CrossRef] [PubMed]
[5]. Balgir RS, Hereditary persistence of foetal haemoglobin in a tribal family of Orissa, IndiaNat Med J India 2004 17(3):138-40. [Google Scholar]
[6]. de Souza GC, Carrocini C, Antoniazzo PJZ, Bonini-Domingos CR, What influences Hb fetal production in adulthood?Rev Bras Hematol Hemoter 2011 33(3):231-36.10.5581/1516-8484.2011005923049301 [Google Scholar] [CrossRef] [PubMed]
[7]. Elghentany MT, Banki K, Erythrocyte disordersIn Henry’s clinical diagnosis and management by laboratory methods 2007 21st edSaunders, McPherson et al.:504-44. [Google Scholar]
[8]. Chatterjee S, Basak P, Chaklader M, Das P, Pereira JA, Chadhuri S, Pesticide induced marrow toxicity and effects on marrow cell population and on hematopoietic stromaExpt Toxicol Pathol 2013 65(3):287-95.10.1016/j.etp.2011.09.00222005501 [Google Scholar] [CrossRef] [PubMed]
[9]. Iteire KA, Igbigbi P, Oyibororho O, Toxicological effects of pyrethroids insecticide on the spleen and bone marrow of adult albino ratsNiger J Basic and Appl Sci 2017 25(2):143-50.10.4314/njbas.v25i2.15 [Google Scholar] [CrossRef]
[10]. Mandarapu R, Prakhya BM, In vitro myelotoxic effects of cypermethrin and mancozeb on human hematopoietic progenitor cellsJ Immunotoxicol 2015 12(1):48-55.10.3109/1547691X.2014.88053524499300 [Google Scholar] [CrossRef] [PubMed]
[11]. Okonkwo CO, Ohaeri OC, Atangwho IJ, Haematological changes in rats exposed to insecticidal oils from the leaves of Cassia occidentalis and Euphorbia miliiHeliyon 2019 5(5):eO1746:1-8.10.1016/j.heliyon.2019.e0174631193578 [Google Scholar] [CrossRef] [PubMed]
[12]. Hoogduijn MJ, Rakonczay Z, Genever PG, The effects of anticholinergic insecticides on human mesenchymal stem cellsToxicol Sci 2006 94(2):342-50.10.1093/toxsci/kfl10116960032 [Google Scholar] [CrossRef] [PubMed]
[13]. Picoli C, Cremonese C, Koifman R, Koifman S, Freire C, Occupational exposure to pesticides and hematological alterations; A survey of farm residents in the South of BrazilCiéncia Saude Coletiva 2019 24(6):2325-40.10.1590/1413-81232018246.1314201731269189 [Google Scholar] [CrossRef] [PubMed]
[14]. Konkie B, Disorders of platelets and vessel wallIn ‘Harrison’s principles of Internal medicine 2012 18th edMcGraw Hill medical, Longo et al.:965-73. [Google Scholar]
[15]. Leach MF, Aubuchon JP, Frequency of thrombocytopenia associated with gentamycin therapyImmunohematol 1999 15(4):167-70. [Google Scholar]
[16]. Thein SL, Menzel S, Lathrop M, Garner C, Control of fetal hemoglobin: New insights emerging from genomics and clinical implicationsHum Mol Genet 2009 18(R2):R216-23.10.1093/hmg/ddp40119808799 [Google Scholar] [CrossRef] [PubMed]