Comparison of Efficacy of Slit Skin Smear and Fite Faraco Stain on Histopathology Specimens in Cases of Leprosy
Aishwarya Bhalchandra Patil1, Adarsh Lata Singh2, Bhushan Madke3, Anugandha Ghatge4, Sugat Jawade5, Sudhir Singh6
1 Resident, Department of Dermatology, Venereology and Leprosy, Datta Meghe Institute of Medical Sciences, Sawangi [Meghe], Wardha, Maharashtra, India.
2 Professor, Department of Dermatology, Venereology and Leprosy, Datta Meghe Institute of Medical Sciences, Sawangi [Meghe], Wardha, Maharashtra, India.
3 Professor and Head, Department of Dermatology, Venereology and Leprosy, Datta Meghe Institute of Medical Sciences, Sawangi [Meghe], Wardha, Maharashtra, India.
4 Senior Resident, Department of Dermatology, Venereology and Leprosy, Datta Meghe Institute of Medical Sciences, Sawangi [Meghe], Wardha, Maharashtra, India.
5 Associate Professor, Department of Dermatology, Venereology and Leprosy, Datta Meghe Institute of Medical Sciences, Sawangi [Meghe], Wardha, Maharashtra, India.
6 Assistant Professor, Department of Dermatology, Venereology and Leprosy, Datta Meghe Institute of Medical Sciences, Sawangi [Meghe], Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aishwarya Bhalchandra Patil, Resident, Department of Dermatology, Venereology and Leprosy, Datta Meghe Institute of Medical Sciences, Sawangi [Meghe], Wardha-442004, Maharashtra, India.
E-mail: dradarshlata@yahoo.com
Introduction
Hansen’s disease is an infectious granulomatous disorder with Mycobacterium leprae being the causative agent. Mycobacterium Leprae is an acid-fast bacillus which grows slowly inside host cells mainly neural Schwann cell as well as cutaneous macrophages.
Aim
To study the efficacy of Slit Skin Smear (SSS) and Fite Faraco stain on histopathology for diagnosis in leprosy.
Materials and Methods
The present cross-sectional study carried out on patients clinically diagnosed as Leprosy attending dermatology OPD in AVBRH, Sawangi, Wardha, Maharashtra, India from sepetember 2017 to August 2019. A total of 88 patients who gave informed consent to participate in study and their clinical features were recorded including number, size and location of lesions and loss of sensation. Any contiguous cutaneous nerve or peripheral nerve trunk enlargement was noted and were classified according to the Ridley-Jopling Classification. SSS and Fite Faraco stain on histopathology specimens was done. The quantitative variables were compared using Kruskal Wallis Test and qualitative variables were correlated using Chi-square test/Fisher’s-Exact test.
Results
Out of 88 (n=88) clinically diagnosed leprosy cases enrolled in this study, 2, 17, 15, 6, 20, 25 and 3 cases were diagnosed as indeterminate, Tuberculoid Leprosy (TT), Borderline Tuberculoid Leprosy (BT), Mid Borderline leprosy (BB), Borderline Lepromatous Leprosy (BL), Lepromatous Leprosy (LL) and pure neural leprosy, respectively. Mycobacterium leprae detection by SSS was possible in 21.59% cases while detection by Fite Faraco staining on tissues sections was possible in 11.36% cases. There were 10 (11.36%) cases in which Mycobacterium leprae was detected by SSS but not by Fite Faraco, while in 7 (7.95%) cases. Mycobacterium leprae was detected by Fite Faraco staining but not by slit skin smear microscopy. The difference in detection by the two methods was found statistically significant with p-value 0.002. On comparison-slit skin smear had sensitivity of 26.47% whereas Fite Faraco had 23.53%. The specificity Fite faraco staining was 100% while that of SSS was found to be 95%.
Conclusion
On comparison of efficacy of SSS and Fite faraco staining on tissue sections, SSS had the highest detection rate and sensitivity in diagnosing leprosy whereas Fite Faraco was found to be more specific.
Histopathological stains, Mycobacterium leprae, Ridley-Jopling classification
Introduction
Hansen’s disease is an infectious granulomatous disorder with Mycobacterium leprae being the causative agent. Mycobacterium Leprae is an acid-fast bacilli which grows slowly inside host cells mainly neural Schwann cell as well as cutaneous macrophages [1]. The transmission of the organism occurs through nasal or oral droplets in close contacts of patients with high bacillary load, seen in multibacillary type of leprosy [2]. The Multidrug therapy was introduced globally in 1982 [3]. On introduction of Multidrug therapy, the fall in prevalence rate has been evident but the fall in incidence rate has not been equivalent [4].
Post-elimination, India has a 60% share in freshly diagnosed leprosy patients from all around the world. Few endemic areas continue to remain the source of numerous fresh cases [5]. Maharashtra is one of the endemic states for leprosy in India with a prevalence rate of 0.81/10000 population [6].
Mycobacterium leprae cultivation in vitro has failed after repeated attempts. Hence currently the diagnosis of leprosy at various tertiary centres is done by the means of clinical suspicion followed by confirmation with SSS and/or histopathological examination of cutaneous biopsy samples. Microscopic examination is easy and convenient method for peripheral or referral centre.
SSS is a cyto-diagnostic technique that detects M. Leprae bacilli by making small cuts in the lesional skin followed by smearing the intradermal fluid on a glass slide. It is a safe and easy side laboratory based technique. SSS is one of the three WHO cardinal signs of leprosy. Even though SSS has a very high specificity but this diagnostic modality lacks sensitivity. Ziehl Nelson stain is used to detect acid-fast Mycobacteria in the SSS smear. The sensitivity of SSS was reported to be 10-50% and specificity 100% [2]. Skin biopsy from suspected lesions followed by histopathological examination is currently considered as the gold standard for the diagnosis, particularly in early stages and paucibacillary type of leprosy. The added advantage of histopathological examination is that it throws light on the type of host-immune response mounted against the organism and also predicts the likely course of the disease and response to treatment.
Fite-Faraco (FF) stain detects M leprae due to the acid-fastness of the bacilli due to the presence of mycolic acid in their cell wall. Hence the bacilli retain the primary stain (Carbol fuchsin) whereas the rest are stained by the secondary stain acetified Methylene Blue. The stain is done on the deparaffinised histopathology sections stains [7]. The sensitivity of Fite faraco staining has been found to be 40-70% [8].
In the study by Kumaran SM et al., detection of mycobacterium leprae by Fite Faraco stain on tissue sections was found to be superior to that in slit skin smear [9]. Due to paucity of similar studies done in this area, the current study was undertaken to compare the efficacy of detection of Mycobacterium Leprae by slit skin smear microscopy with Fite Faraco staining done on tissue sections.
Materials and Methods
The present cross-sectional study was carried out on patients clinically diagnosed with Leprosy, attending dermatology OPD in AVBRH, Sawangi, Wardha, India in a period of two years from September 2017 to August 2019, after obtaining Institutional Ethics Committee clearance {DMIMS (DU) IEC /2017-18/6710}.
Sample Size Calculation
Sample size formula for studies with binary test outcome was used.
n=Z2α/2 p(1-p)/d2
where, ‘p’ is predetermined value of sensitivity or specificity as ascertained by previously published data and for α=0.05 Zα/2 is inserted by 1.96.
Total 88 patients who gave informed consent to participate in study were enrolled and their clinical features were recorded including number, size and location of lesions and loss of sensation. All cases diagnosed clinically as leprosy were enrolled in the study whereas patients not willing to participate in the study or investigate the disease were excluded from the study. Any patients with cutaneous manifestations of leprosy or peripheral nerve trunk enlargement were noted in enrolled patients and were further classified according to the Ridley DS and Jopling WH Classification [10].
Slit Skin Smear (SSS)
SSS were taken from six sites (two earlobes, two from forehead just above the medial aspect of eyebrows and two from lesions) from a patient. A 5 mm thick smear was made. After air-drying the smears, they were stained by carbol Fuchsin for 10 minutes followed by wash and decolourising with 1% acid alcohol and then counterstained with Methylene blue [2]. Slit skin smear was interpreted as positive if M. leprae were detected, stained in red in a light blue background and negative if no bacteria were seen on examination of the complete smear.
After performing punch skin biopsy, the samples were fixed in 10% formalin for about 8-12 hours, following which the samples underwent routine processing after which the paraffin embedded sections of 4-5 μm thickness were stained with haematoxylin and eosin for microscopic examination of the morphology and modified Fite Faraco’s staining for identifying Mycobacterium leprae in the tissue.
Fite-Faraco Staining for Tissue Sections
The paraffinized sections were placed in Xylene and peanut oil mixture with two changes for 30 minutes followed by staining with strong commercially available Carbol fuchsin for 25 minutes followed by washing in warm running tap water for 3 minutes. Sections were then decolourised in 5% sulfuric acid in 25% alcohol to changes of 90 seconds each till sections turn into pale pink colour followed by washing in warm running tap water for 5 minutes. Counter-staining was done in working Methylene blue {working methylene blue 5 mL stock (methylene blue 1.4 gm in 100 mL of 95% alcohol) add in 45 mL tap water} by one quick dip till sections turn into pale blue. Sections were then blotted followed by drying in 50-55°C oven for 5 minutes. Once dry, the slides underwent a quick dip in xylene. Then the sections were mounted with permanent mountant. The stained sections with the above modifications were observed under oil immersion using 100X objectives. The entire dermis was observed for acid-fast bacilli which looked bright red and the nuclei and other tissue elements looked pale blue [7].
After studying the histopathological features and noting the bacteriological status, the diagnosis of leprosy was confirmed and classified according to Ridley and Jopling classification and a report was created including diagnosis and AFB status after which clinico-pathological correlation was done.
Statistical Analysis
Statistical analysis was done by Statistical Package for Social Sciences (SPSS) version 21.0. Continuous variables were presented as mean±SD and median. Categorical variables were presented as number and percentage (%). Normality of data was tested by Kolmogorov-Smirnov test.
Results
Eighty eight (n=88) clinically diagnosed leprosy cases were enrolled in this study out of which 2, 17, 15, 6, 20, and 25 cases were diagnosed as indeterminate, TT, BT, BB, BL, and LL, respectively. SSS was done in these patients [Table/Fig-1]. Also, punch biopsies were taken from these patients and processed for histopathological studies [Table/Fig-2,3].
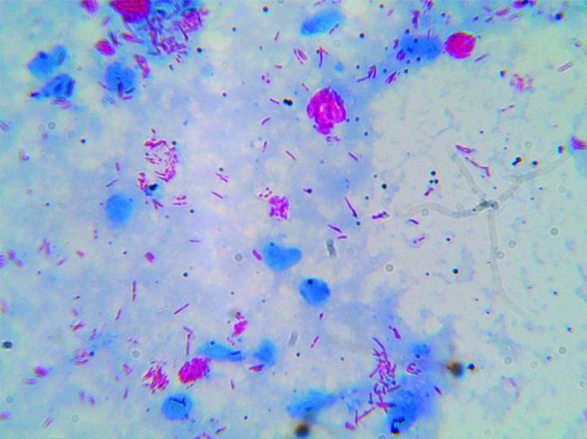
Demonstrating AFB on SSS in clumps/globi (100X).
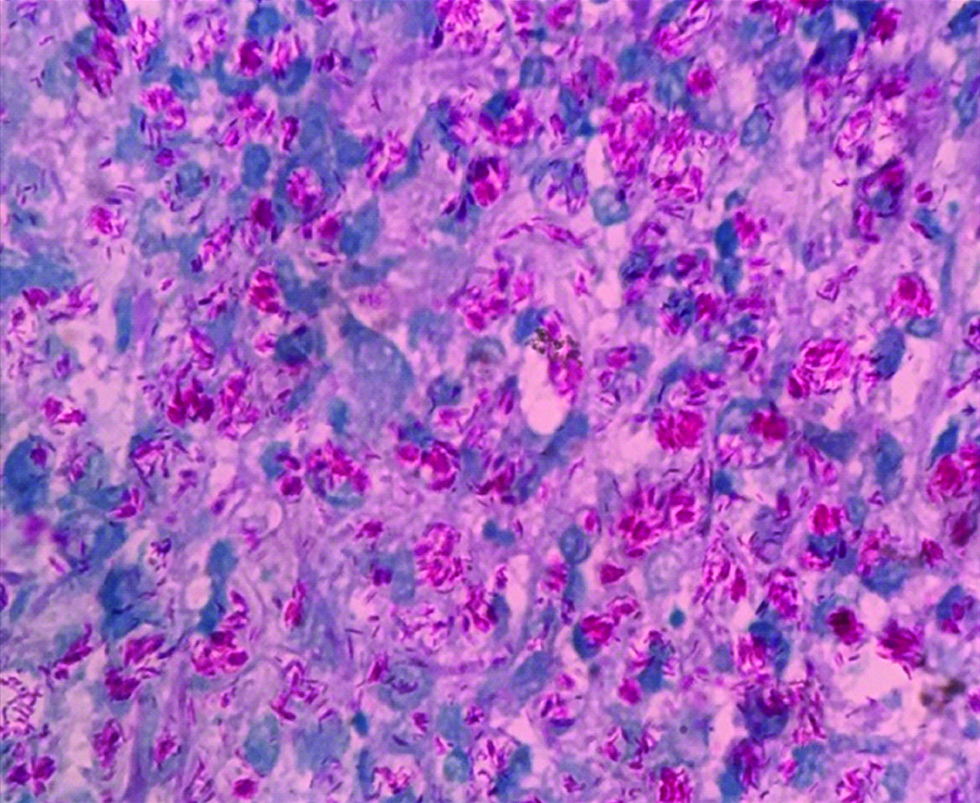
Photomicrograph showing many Virchow cells-laden with plenty of Acid-fast Bacilli arranged in globi. (100X; Fite-Faraco stain).
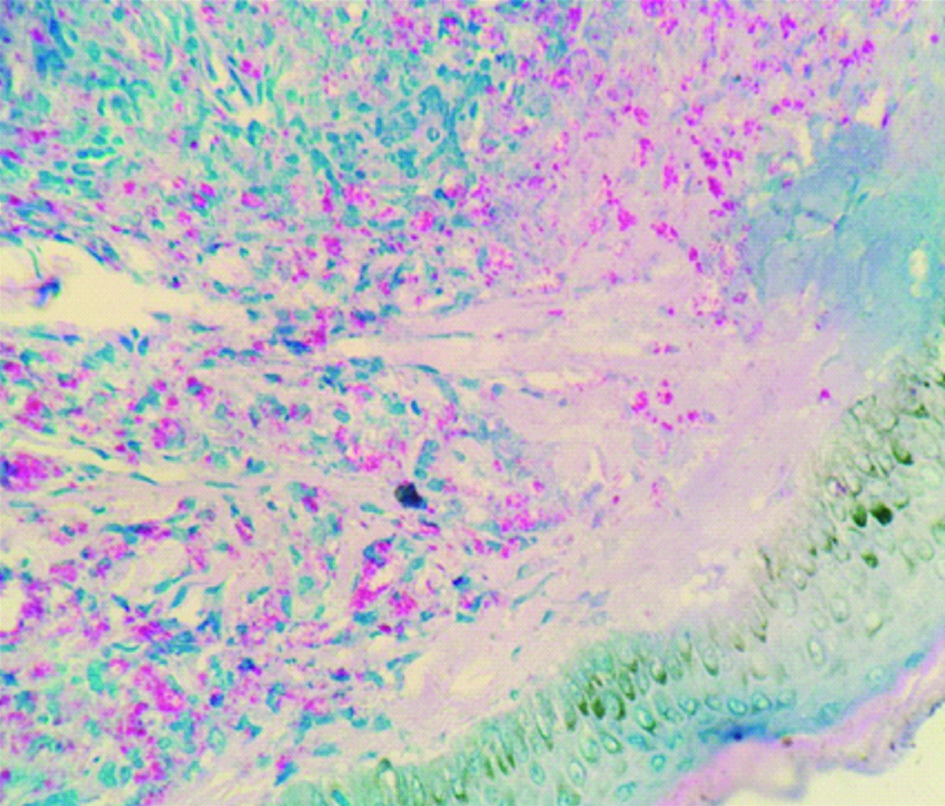
Photomicrograph showing numerous Acid-fast Bacilli. (100X; Fite Faraco stain).
Considering clinical diagnosis as a reference, the concordance of different techniques were as follows: SSS could detect AFB in 19 cases (21.59%), H&E staining suggested 68 cases (77.27%) as positive with an indirect evidence of features suggestive of M. leprae infection [Table/Fig-4]. Fite Faraco (FF) staining showed a total of 10 cases (11.36%) positive for the presence of AFB in the tissue section as shown in [Table/Fig-5]. There were 10 (11.36%) cases in whom AFB were detected by SSS but not by Fite Faraco, while in 7 (7.95%) cases AFB were detected by Fite Faraco but not by SSS. In 9 (10.23%) cases, AFB was detected by both the methods SSS as well as Fite Faraco. The difference in the two methods of detection was found statistically significant as shown in [Table/Fig-5].
Comparison of various diagnostic modalities in diagnosing leprosy.
| No. of cases | SSS | Fite faraco stain in biopsy tissue |
|---|
| +ve | -ve | +ve | -ve |
|---|
| 88 | 19 (21.59%) | 69 (78.41%) | 16 (18.18%) | 72 (81.81%) |
SSS: Slit skin smear
Comparison between detection of AFB stained by Fite Faraco method and SSS.
| Fite faraco | Total | p-value |
|---|
| -ve | +ve |
|---|
| SSS | -ve | 62 (70.45%) | 7 (7.95%) | 69 (78.41%) | 0.002 |
| +ve | 10 (11.36%) | 9 (10.23%) | 19 (21.59% |
| Total | 72 (81.81%) | 16 (18.18%) | 88 (100.00%) |
SSS: Slit skin smear
The “true” diagnostic performance of various techniques is shown in [Table/Fig-6] with histopathology kept as gold standard. A higher sensitivity i.e., 26.47% in SSS and higher specificity i.e., 100% in Fite Faraco staining was observed.
Diagnostic performance of SSS and Fite Faraco [7,8,11].
| SSS [Present study] | SSS Gautam M et al., [11] | Fite faraco [Present study] | Fite farac Cabic E et al., [8] | Fite farac Reja AHH et al., [7] |
|---|
| Sensitivity | 26.47% | 10-50% | 23.53% | 40-70% | 74.6% |
| Specificity | 95% | 100% | 100% | - | - |
Discussion
Early diagnosis is of fundamental importance to all the aspects of Hansen’s disease like epidemiology, management and prevention of deformities. Both SSS followed by Zeihl Nelson (ZN) staining and Fite Faraco staining detect AFB in tissues. SSS detects AFB in smear taken from dermis whereas Fite Faraco method detects AFB in tissue obtained by skin biopsy taken from clinically suspected lesions. In the present study, sensitivity of SSS was found to be 26.47% which was comparable with values mentioned in the study by Gautam M and Jaiswal A but a specificity of 95% was observed in the present study while it was 100% as compared by the same perivious study, which could be explained due to the presence of non-pathogenic AFB positive bacilli in the environment [11]. Sensitivity of Fite faraco was observed lower ie. 23.53% in comparison to other studies by Cabice et al and Reja AHH et al with 40-70% and 74.6% respectively [7,8]. This could be due to undetected dead bacilli. A statistically significant difference was found between the two diagnostic modalities i.e., fite faraco staining and SSS staining, with p-value 0.002. In the study by Kumaran SM et al., done in India, 100% skin biopsy specimens demonstrated AFB in their sections by modified Fite Faraco staining tissue specimens in whom SSS was found positive [9]. The reason for SSS positive cases diagnosed as Fite Faraco negative could be that the bacillary load in the biopsy sample was less as it was taken from a single site whereas SSS smears were taken from multiple sites. In the present study, according to [Table/Fig-4], detection rates in the diagnostic modalities SSS and Fite Faraco stain on tissues were compared with detection rate of 21.59% of SSS while the detection rate by Fite Faraco staining on biopsy tissue with was found to be 18.18%. In a study by Reja AHH et al., detection rate of Fite Faraco was found to be 60% and SSS detected least with 40.6% detection rate [7]. The detection rates in the present study and the study by Reja AHH et al., was not comparable. Low detection of Fite Faraco and SSS could be explained by lack of AFB in tissues either due to effect of treatment or killing mediated by immune responses [7].
Limitation(s)
The bacillary index on slit skin smear and bacillary index of granuloma was not calculated.
Conclusion(s)
It was evident from the findings in the present study that Slit Skin Smear (SSS) is more sensitive diagnostic modality whereas Fite Faraco was more specific. The modalities of diagnosis; SSS and Fite Faraco may have some additive value in diagnosing leprosy but cannot diagnose substantial amount of cases when used alone. Hence, the conclusion that there is a need for elaborate research for feasible, sensitive and specific modalities of diagnosis for leprosy in today’s time.
SSS: Slit skin smear
SSS: Slit skin smear
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 12, 2019
Manual Googling: Nov 11, 2019
iThenticate Software: Feb 12, 2020 (13%)
[1]. Martinez AN, Talhari C, Moraes MO, Talhari S, PCR-Based Techniques for Leprosy Diagnosis: From the Laboratory to the ClinicPLoS Negl Trop Dis [Internet] 2014 8(4)Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3983108/10.1371/journal.pntd.000265524722358 [Google Scholar] [CrossRef] [PubMed]
[2]. Siwakoti S, Rai K, Bhattarai NR, Agarwal S, Khanal B, Evaluation of Polymerase Chain Reaction (PCR) with Slit Skin Smear Examination (SSS) to confirm clinical diagnosis of leprosy in eastern NepalPLOS Negl Trop Dis 2016 10(12):e000522010.1371/journal.pntd.000522028027305 [Google Scholar] [CrossRef] [PubMed]
[3]. Rao PN, Suneetha S, Current situation of leprosy in India and its future implicationsIndian Dermatol Online J 2018 9(2):8310.4103/idoj.IDOJ_282_1729644191 [Google Scholar] [CrossRef] [PubMed]
[4]. Banerjee S, Sarkar K, Gupta S, Mahapatra PS, Gupta S, Guha S, Multiplex PCR technique could be an alternative approach for early detection of leprosy among close contacts- A pilot study from IndiaBMC Infect Dis 2010 10:25210.1186/1471-2334-10-25220735843 [Google Scholar] [CrossRef] [PubMed]
[5]. Naaz F, Katoch K, Mohanty P, Chauhan D, Yadav V, Kumar A, Use of RLEP-PCR as a molecular tool and definitive laboratory test from skin smear scrapings for early diagnosis of leprosy in field situationsIndian Journal of leprosy 2016 88(4):199-207. [Google Scholar]
[6]. NLEP Annual Report 2016-2017 Central Leprosy Division, Directorate General of Health Services, Ministry of Health and Family Welfare Government of India, Nirman Bhavan, New Delhi [Google Scholar]
[7]. Reja AHH, Biswas N, Biswas S, Dasgupta S, Chowdhury IH, Banerjee S, Fite-Faraco staining in combination with multiplex polymerase chain reaction: A new approach to leprosy diagnosisIndian J Dermatol Venereol Leprol 2013 79(5):693-700.10.4103/0378-6323.11674023974586 [Google Scholar] [CrossRef] [PubMed]
[8]. Cabic E, Cabic AG, Esposo SM, Dizon F, Quinones GJ, Guia A, Histopathological detection of mycobacterium tuberculosis and mycobacterium leprae using a modified acid-fast techniquePhilippine J Pathol 2018 3(1):2910.21141/PJP.2018.007 [Google Scholar] [CrossRef]
[9]. Kumaran SM, Bhat IP, Madhukara J, Rout P, Elizabeth J, Comparison of bacillary index on slit skin smear with bacillary index of granuloma in leprosy and its relevance to present therapeutic regimensIndian J Dermatol 2015 60(1):51-54.10.4103/0019-5154.14779125657397 [Google Scholar] [CrossRef] [PubMed]
[10]. Ridley DS, Jopling WH, Classification of leprosy according to immunity. A five-group systemInt J Lepr 1966 34(3):255-73. [Google Scholar]
[11]. Gautam M, Jaiswal A, Forgetting the cardinal sign is a cardinal sin: Slit-skin smearIndian Journal of Paediatric Dermatology 2019 20(4):341-44.10.4103/ijpd.IJPD_74_19 [Google Scholar] [CrossRef]