To Assess the Quality of Life in Patients with Benign Prostate Hyperplasia (BPH) Based on Urinary Symptoms
Divmehar Kaur1, Harpreet Kaur Massaon2, Harjinder Singh3, Maninder Kaur4
1 MBBS Extern, Department of Urology, Government Medical College, Patiala, Punjab, India.
2 Msc Student, Department of Biochemistry, Government Medical College, Patiala, Punjab, India.
3 Professor and Head, Department of Urology, Government Medical College, Patiala, Punjab, India.
4 Professor and Head, Department of Biochemistry, Government Medical College, Patiala, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Maninder Kaur, House No. 53-B/2, Model Town, Patiala, Punjab, India.
E-mail: mkaur68@yahoo.com
Introduction
Benign Prostatic Hyperplasia (BPH) is a common condition in older men that can often result in Lower Urinary Tract Symptoms (LUTS). BPH is a disease in which the prostate gland enlarges beyond the normal volume of 20-30 mL as part of the ageing process. The severity of LUTS can be estimated by the International Prostate Symptoms Score (IPSS). LUTS associated with BPH can have a significant negative impact on the Quality of Life (QoL) of patients.
Aim
To assess the severity of symptoms and the QoL of patients with BPH based on IPSS Score and QoL Score.
Materials and Methods
The present study is a qualitative study conducted over a period of one month. Hundred patients constituted the study group and 50 age-matched males constituted the control group. The patients were interviewed using close-ended questions as described in the pre-tested and validated questionnaire based on IPSS scoring system.
Results
In the study group, 20 patients of age group 41-50 years, 20 patients of age group 51-60 years, 20 patients of age group 61-70 years, 20 patients of age group 71-80 years and 20 patients of age group 81-90 years. Symptoms with which the patients presented were frequency, nocturia, urgency, straining, weak stream, intermittency and incomplete emptying. Out of which nocturia and incomplete emptying were the predominant symptoms. It was found that the maximum symptoms were observed in the age group more than 50 years. It was observed that with the increase in the age, the severity of the symptoms increased and was statistically significant (p=<0.001). The QoL score of the patients with BPH is maximum in the age group 81-90 years. Maximum patients were dissatisfied with their conditions.
Conclusion
In the present study it was concluded that according to the IPSS Score the main LUTS affecting QoL were nocturia and incomplete emptying of urinary bladder. Maximum severity of symptoms (IPSS Score of more than 18) was observed in patients more than 80 years of age. LUTS associated with BPH have a significant negative impact on the (QoL) of patients. The IPSS Symptom Score and QoL questionnaires help the clinicians to better understand patient’s symptoms and their impact and can aid in assessing the results of treatment. Validated Questionnaires can be extremely useful in clinical practice as well as research.
International prostatic symptom score, Lower urinary tract symptoms, Questionnaire
Introduction
BPH is characterised by the non-malignant overgrowth of prostatic tissue surrounding the urethra, ultimately constricting the urethral opening and giving rise to associated LUTS [1].
The present study was carried out to assess the QoL of patients with BPH on IPSS Score and QoL. BPH can be defined as documentable gross or histologic growth of prostate glandular tissues, stromal tissues, or both. Usually, beginning around the age of 40 years, the prevalence of BPH rises to more than 50% at 50 years of age to as much as 90% at the age of 85 years. As life expectancy increases, BPH will be a significant cause of morbidity. About 50% of men with histologically proven BPH have moderate to severe LUTS that are symptoms related to storage and voiding of urine [2].
LUTS are categorised into three groups voiding symptoms, storage symptoms and post micturition symptoms which become common with age, impacting health related QoL. To elaborate, voiding symptoms includes slow stream, splitting/spraying, intermittency, hesitancy, straining and terminal dribble, storage symptoms includes increased daytime frequency, nocturia, urgency and urinary incontinence and post-micturition symptoms including feeling of incomplete emptying and post-micturition dribble [3,4].
The I-PSS is vital tool for clinical management of patients with LUTS and also as mentioned in verious research studies regarding the medical and surgical treatment of patients with voiding dysfunction. This system as explained contains several questions, based on which LUTS is classified as mild, moderate and severe with score of 0-7, 8-19 and 20 to 35, respectively [5].
In the clinical practice, the guidelines for the diagnosis and treatment of BPH have been issued by the Agency For Health Care Policy And Research (AHCPR) [6], it was recommended that symptoms of BPH be taken into account in making treatment recommendations based on a standard symptom questionnaire known as IPSS and QoL Score [5].
The IPSS is a scoring system used to screen for and diagnose BPH as well as to monitor symptoms and guide decisions about how to manage the disease [7]. It is based on several questions, of which one pertain to quality of life and rest seven pertain to disease symptoms. Further, the answers are scored on scale of 1 to 6 for QoL and 1 to 5 for disease symptoms [8].
One of the most significant contributions of IPSS is to efficiently monitor treatment efficacy. According to the total IPSS Score, the severity of LUTS is usually graded as mild (0-7), moderate (8-19) and severe (20-35). According to these guidelines, patients with mild symptoms do not require treatment or further investigation [8]. IPSS is currently the standard questionnaire for the objective assessment of LUTS throughout the world. The study has been reported by Kamil C, Lowe Franklin C, Nagarathnam M and Latheef S [9-11]. Indications of BPH surgery includes refractory symptoms to medical condition/state which implies the importance of scores accuracy.
Certain limitations have been analysed in the above stated studies. The present study was carried out to assess the QoL of patients with BPH on IPSS Score and QoL. The different parameters were analysed age wise and the prevalence of the parameters assessed in this study lacks in the studies mentioned above.
Materials and Methods
The present cross-sectional study was conducted at Rajindra Hospital, Patiala in Department of Biochemistry in the month of March 2019. Hundred patients of different age groups from 41 to 90 years constituted the study group and 50 age matched males constituted the control group. The patients were interviewed using close-ended questions as described in the pretested and validated questionnaire based on IPSS scoring system. Ethics approval was obtained for the study.
Inclusion Criteria
Male patients >40 years of age with BPH and presenting with LUTS and those who had filled their consent form for the study.
Exclusion Criteria
Patients with UTI, Prostatitis, Stricture urethra, Prostate cancer and those who did not give consent.
Statistical Analysis
The data was analysed using Microsoft Excel Software 2017; SPSS 19.0 version. Chi-Square tests, Mann- Whitney tests and t-test were done to analyse the data.
Results
Patients with BPH presented symptoms such as frequency, nocturia, urgency, straining, weak stream, intermittency, and incomplete emptying. Out of these, nocturia and incomplete emptying were the predominant symptoms [Table/Fig-1].
| Symptom | Not at all | <1 Time in 5 | Less than the time | About half the time | More than half the time | Almost always | Your score |
|---|
| Incomplete emptyingOver the past month, how often have you had a sensation of not emptying your bladder completely after you finished urinating? | 0 | 1 | 2 | 3 | 4 | 5 | |
| FrequencyOver the past month, how often have you had to urinate again <2 hours after you finished urinating? | 0 | 1 | 2 | 3 | 4 | 5 | |
| IntermittencyOver the past month, how often have you found you stopped and started again several times when you urinated? | 0 | 1 | 2 | 3 | 4 | 5 | |
| UrgencyOver the past month, how often have you found it difficult to postpone urination? | 0 | 1 | 2 | 3 | 4 | 5 | |
| Weak streamOver the past month, how often have you had a weak urinary stream? | 0 | 1 | 2 | 3 | 4 | 5 | |
| StrainingOver the past month, how often have you had to push or strain to begin urination? | 0 | 1 | 2 | 3 | 4 | 5 | |
| None | 1 times | 2 times | 3 times | 4 times | ≥5 times | |
| NocturiaOver the past month, how many times did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning? | 0 | 1 | 2 | 3 | 4 | 5 | |
| Total IPPS score | | | | | | | |
| QoL due to urinary symptoms | Delighted | Pleased | Mostly satisfied | Mixed about equally satisfied and dissatisfied | Mostly dissatisfied | Unhappy | Terrible |
| If you were to spend the rest of your life with your urinary condition just the way it is now, how would you feel about that? | 0 | 1 | 2 | 3 | 4 | 5 | 6 |
IPSS: International prostate symptoms score; QoL: Quality of life
There were 20 patients of age groups 41-50 years, 20 patients of age group 51-60 years, 20 patients of age group 61-70 years, 20 patients of age group 71-80 years and 20 patients of age group 81-90 years. It was found that the maximum symptoms were observed in the age group more than 50 years [Table/Fig-2].
Relationship of age with symptoms.
| Symptoms | | |
|---|
| Age (in years) | Incomplete emptying | Intermittency | Weak stream | Straining | Frequency | Urgency | Nocturia | Mean±SD | p-value |
|---|
| 41-50 | 4 | 5 | 1 | 1 | 4 | 1 | 4 | 2.8±1.6 | <0.0001 |
| 51-60 | 4 | 2 | 2 | 4 | 3 | 1 | 4 | 2.8±1.1 |
| 61-70 | 4 | 1 | 1 | 3 | 5 | 2 | 4 | 2.8±1.4 |
| 71-80 | 4 | 1’ | 4 | 4 | 3 | 1 | 3 | 2.8±1.2 |
| 81-90 | 4 | 2 | 2 | 2 | 2 | 3 | 5 | 2.8±1.1 |
| 20 | 11 | 10 | 14 | 17 | 8 | 20 | | |
SD: Standard deviation
The maximum mean value of IPSS Score was 23.3±5.43 in the age group 81-90 years. It was observed that with the increase in age the severity of symptoms increased and was statistically significant. Hence most severe symptoms were observed in patients >80 years of age [Table/Fig-3].
Relationship between age and Ipss score.
| IPSS score | | |
|---|
| Age (in years) | Mild (0-7) | Moderate (8-18) | Severe (>18) | Mean±SD | p-value |
|---|
| 41-50 | 6 | 11 | 5 | 14.4±7.60 | <0.001 |
| 51-60 | 4 | 9 | 7 | 16.0±5.82 |
| 61-70 | 2 | 10 | 12 | 19.5±8.15 |
| 71-80 | 3 | 2 | 13 | 20.8±8.84 |
| 81-90 | 0 | 5 | 11 | 23.3±5.43 |
| Total | 15 | 37 | 48 | | |
IPSS: International prostate symptoms score; SD: Standard deviation
The maximum mean value of QoL Score of patients with BPH was 2.8±4.7 in the age group 81-90 years. And it was observed that maximum patients were dissatisfied with their conditions [Table/Fig-4].
Relationship between age and QoL score.
| QoL Score | | |
|---|
| Age (in years) | 0 Delighted | 1Pleased | 2Mostly satisfied | 3Mixed about equally satisfied and dissatisfied | 4Mostly dissatisfied | 5Unhappy | 6Terrible | Mean±SD | p-value |
|---|
| 41-50 | 0 | 0 | 6 | 4 | 9 | 1 | 0 | 2.8±3.3 | <0.001 |
| 51-60 | 0 | 0 | 3 | 6 | 11 | 0 | 0 | 2.8±3.9 |
| 61-70 | 0 | 0 | 3 | 4 | 12 | 1 | 0 | 2.8±4.0 |
| 71-80 | 0 | 0 | 5 | 3 | 12 | 0 | 0 | 2.8±4.1 |
| 81-90 | 0 | 0 | 3 | 3 | 14 | 0 | 0 | 2.8±4.7 |
| Total | 0 | 0 | 20 | 20 | 58 | 2 | 0 | | |
QoL: Quality of life; SD: Standard deviation
According to socio-demographic analysis the maximum severity of symptoms was observed as follows [Table/Fig-4]:
Area wise: In rural areas
Education Scale: Among the patients who had primary schooling, diploma holders and graduates.
Occupation: In unemployed patients [Table/Fig-5]
IPSS score according to socio-demographic analysis.
| Category | IPSS | Mean±SD | p-value |
|---|
| Mild | Moderate | Severe | | |
|---|
| 1. Area (n=150) | |
| Rural (n=96) | 14 | 30 | 52 | 32.0±19.0 | <0.001 |
| Urban (n=54) | 09 | 22 | 23 | 18.0±7.8 |
| 2.Education (n=150) | |
| Illiterate (n=42) | 10 | 25 | 07 | 14.0±9.6 | <0.001 |
| Literate (n=108) | |
| Primary school (n=10) | 02 | 02 | 06 | 3.3±2.3 | <0.001 |
| Middle school (n=28) | 09 | 10 | 09 | 9.3±1.5 |
| High school (n=15) | 02 | 09 | 04 | 5.0±3.6 |
| Diploma (n=18) | 02 | 05 | 11 | 06±4.5 |
| Graduation (n=16) | 03 | 04 | 09 | 5.3±3.2 |
| Post graduation (n=12) | 08 | 02 | 02 | 4.0±3.4 |
| Profession or Honors (n=09) | 05 | 03 | 01 | 3.0±1.6 |
| 3.Occupation (n=150) | |
| Unemployed (n=50) | 05 | 11 | 34 | 16.6±15.3 | <0.001 |
| Semi skilled (n=42) | 05 | 22 | 15 | 14.0±8.5 |
| Skilled (n=58) | 03 | 23 | 32 | 19.3±14.8 |
| 4.Monthly income (n=150) | |
| Upper class (n=34) | 11 | 14 | 09 | 11.3±2.0 | <0.001 |
| Upper middle class (n=35) | 12 | 14 | 09 | 11.6±2.0 |
| Lower middle class (n=46) | 17 | 10 | 19 | 15.3±3.8 |
| Lower class (n=35) | 10 | 08 | 17 | 11.6±3.8 |
IPSS: International prostate symptoms score; SD: Standard deviation
Economically: In lower middle class and lower class patients.
IPSS score and QoL score in patients with BPH of various ages were compared and shown in [Table/Fig-6]. The results were statistically significant, with p-value <0.001.
Comparison of IPSS score and QoL score in patients with BPH of various age.
| Age (in years) | Mean±SD (IPSS score) | Mean±SD (QoL) | p-value |
|---|
| 41-50 | 14.4±7.60 | 2.8±3.3 | <0.001Highly significant |
| 51-60 | 16.0±5.82 | 2.8±3.9 |
| 61-70 | 19.5±8.15 | 2.8±4.0 |
| 71-80 | 20.8±8.84 | 2.8±4.1 |
| 81-90 | 23.3±5.43 | 2.8±4.7 |
IPSS: International prostate symptoms score; QoL: Quality of life; SD: Standard deviation
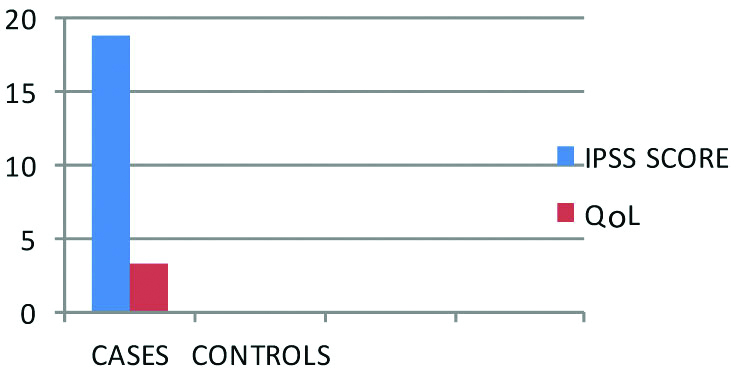
In the above chart it was observed that the healthy controls were not suffering from any of the symptoms and had a delighted QoL as compared to the patients who were suffering from various symptoms like incomplete emptying [Table/Fig-7].
Correlation between the cases and controls on the bases of IPSS score and QoL.
IPSS: International prostate symptoms score; QoL: Quality of life
Discussion
BPH is one of the most common diseases of the ageing men. It is associated with LUTS that affect individual QoL and cause significant economic burden to the society [9]. BPH causes Bladder Outlet Obstruction (BOO) among affected men and the several symptoms of BPH, which include LUTS which can adversely affect QoL [10,11].
In the present study, it was observed that with the increase in age, the severity of symptoms increased and was maximum in 81-90 years of age. This is explained probably by a progressive decrease in serum testosterone levels in males with advancing age. Also the increased severity of symptoms with increasing age may be associated with a history of prostatitis, recurrent urinary tract infections, catheterisations or any surgical interventions causing uretheral strictures. The present study was similar to the studies conducted by Girman CJ et al., Lee E et al., Trueman P et al., Tsukamoto T et al., also found the age was positively correlated to the increase in the severity of the symptoms [Table/Fig-2] [12-15].
BPH can be associated with a number of health-related problems relevant to older men, including increased risk of acute urinary retention, sexual dysfunction, and BPH-related surgery [16,17]. Patients with LUTS experiencing nocturia adversely affects their quality of life in negative manner. Nocturia further act as a higher risk factor of mortality as it is partly associated with injuries and complications resulting from falls at night. Further in day time nocturia may lead to sleepiness which may led to increased risk of accidents while driving and in the workplace [18,19].
LUTS associated with BPH is accompanied by factors as erectile dysfunction or ejaculation related problems. The subjects state that these bladder related incidents limit their freedom and certain bathroom visits with intermittent catheters made them anxious [20]. The severity of LUTS was associated with socio-demographic characteristics. According to socio-demographic analysis, the maximum severity of symptoms was observed as follows [Table/Fig-5]. This study was similar to the study conducted by Jo JK et al., [8]. Incomplete empting of the bladder and nocturia were the most frequent symptoms observed in the present study. Among the patients suffering from Nocturia and the patients complaining of incomplete emptying of their urinary bladder generally were dissatisfied with their urinary conditions. The present study was similar to that of the study conducted by Mark S et al., [18]. The maximum numbers of patients were dissatisfied and unhappy with their QoL [Table/Fig-4]. LUTS associated with BPH have a significant negative impact on patient’s QoL.
In addition to the economic burden of the condition, LUTS secondary to BPH can have a major impact on men and their families, as QoL is greatly impacted, to a greater extent with more severe symptoms, and gets worse over time [18].
Nocturia is the main symptom affected in the age group 81-90 years. This high dependence on age may be caused by several factors. As a result of age-associated problems like renal-concentrating ability, low sodium-absorbing ability, irregular or loss of circadian rhythm of ADH secretion, diminished secretion of renin angiotensin-aldosterone, increased secretion of atrial natriuretic hormone etc, older men have ability to urinate more than younger ones. These factors led to increased night-time urine production in older people. Also, it may be an alteration of sleep pattern with age. This study is similar to the study conducted by Andersson SO et al., [20].
Limitation(s)
Being a cross-sectional study, response-tolerance threshold varies from individual to individual. Smaller sample size also limits the study.
Conclusion(s)
In the present study, it was concluded that according to the IPSS Score, the main LUTS affecting QoL were nocturia and incomplete emptying of urinary bladder, LUTS associated with BPH have a significant negative impact on the QoL of patients. The IPSS and QoL questionnaires help the clinicians to better understand patients’ symptoms and their impact and can aid in assessing the results of treatment. Validated Questionnaires can be extremely useful in clinical practice as well as research. Studies with larger sample size is recommended
IPSS: International prostate symptoms score; QoL: Quality of life
SD: Standard deviation
IPSS: International prostate symptoms score; SD: Standard deviation
QoL: Quality of life; SD: Standard deviation
IPSS: International prostate symptoms score; QoL: Quality of life; SD: Standard deviation
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 03, 2019
Manual Googling: Jan 06, 2020
iThenticate Software: Feb 12, 2020 (19%)
[1]. Kevin T, McVary BPH: Epidemiology and comorbiditiesAmerican Journal of Managed Care 2006 12(5):S122-28. [Google Scholar]
[2]. Wasserman NF, Benign prostatic hyperplasia: A review and ultrasound classificationRadiol Clin North Am 2006 44(5):689-710.10.1016/j.rcl.2006.07.00517030221 [Google Scholar] [CrossRef] [PubMed]
[3]. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, The standardisation of terminology in lower urinary tract function: Report from the Standardisation Sub-committee of the International Continence SocietyUrology 2003 61(1):37-49.10.1016/S0090-4295(02)02243-4 [Google Scholar] [CrossRef]
[4]. Kupelian V, Wei JT, O’Leary MP, Kusek JW, Litman HJ, Link CL, Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample: The Boston Area Community Health (BACH) SurveyArch Intern Med 2006 166(21):2381-87.10.1001/archinte.166.21.238117130393 [Google Scholar] [CrossRef] [PubMed]
[5]. Wein Alan J, Kavoussi Louis R, Novick Andrew C, Partin Alan W, Peters Craig A, Campbell-Walsh Urology9th edition:81-110. [Google Scholar]
[6]. Mohan A, Kumar Gupta A, A review on the clinical utility of PSA in cancer prostateIndian J Surg Oncol 2012 3(2):120-29.10.1007/s13193-012-0142-623730101 [Google Scholar] [CrossRef] [PubMed]
[7]. The International Prostate Symptoms Score (IPSS) by Dr. Ananya Mandal [Google Scholar]
[8]. Jo JK, Kim KS, Nam JW, Choi BY, Moon HS, Sociodemographic Factors Related to Lower Urinary Tract Symptoms in Men: A Korean Community Health SurveyInt Neurourol J 2017 21(2):143-51.10.5213/inj.1732760.38028673065 [Google Scholar] [CrossRef] [PubMed]
[9]. Kamil C, Should international prostate symptom score solely guide the management of benign prostatic hyperplasia?J Urol Ren Dis 2017 2017(6):01-03. [Google Scholar]
[10]. Lowe Franklin C, Treatment of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: Sexual functionBJU International 2005 95(s4):12-18.10.1111/j.1464-410X.2005.05486.x15871731 [Google Scholar] [CrossRef] [PubMed]
[11]. Nagarathnam M, Latheef SAA, Prevalence of lower urinary tract symptoms in patients of benign prostatic hyperplasia attending Tertiary Care Hospital in the State of Andhra PradeshJ NTR Univ Health Sci 2017 6(3):154-57./10.4103/2277-8632.215533 [Google Scholar] [CrossRef]
[12]. Girman CJ, Epstein RS, Jacobsen SJ, Guess HA, Panser LA, Oesterling JE, Natural history of prostatism: Impact of urinary symptoms on quality of life in 2115 randomly selected community menUrology 1994 44(6):825-31.10.1016/S0090-4295(94)80165-7 [Google Scholar] [CrossRef]
[13]. Lee E, Yoo KY, Kim Y, Shin Y, Lee C, Prevalence of lower urinary tract symptoms in Korean men in a community-based studyEur Urol 1998 33(1):17-21.10.1159/0000195299471036 [Google Scholar] [CrossRef] [PubMed]
[14]. Trueman P, Hood SC, Nayak US, Mrazek MF, Prevalence of lower urinary tract symptoms and self-reported diagnosed ‘benign prostatic hyperplasia’, and their effect on quality of life in a community-based survey of men in the UKBJU Int 1999 83(4):410-15.10.1046/j.1464-410x.1999.00966.x10210562 [Google Scholar] [CrossRef] [PubMed]
[15]. Tsukamoto T, Kumamoto Y, Masumori N, Miyake H, Rhodes T, Girman CJ, Prevalence of prostatism in Japanese men in a community-based study with comparison to a similar American studyJ Urol 1995 154(2 Pt 1):391-95.10.1016/S0022-5347(01)67059-9 [Google Scholar] [CrossRef]
[16]. Gacci M, Bartoletti R, Figlioli S, Sarti E, Eisner B, Boddi V, Urinary symptoms, quality of life and sexual function in patients with benign prostatic hypertrophy before and after prostatectomy: A prospective studyBJU Int 2003 91(3):196-200.10.1046/j.1464-410X.2003.04072.x12581003 [Google Scholar] [CrossRef] [PubMed]
[17]. Yoshimura K, Arai Y, Ichioka K, Terada N, Matsuta Y, Okubo K, Symptom-specific quality of life in patients with benign prostatic hyperplasiaInt J Urol 2002 9(9):485-90.10.1046/j.1442-2042.2002.00503.x12410928 [Google Scholar] [CrossRef] [PubMed]
[18]. Mark S, Kirby R, Doyle S, Ioannou C, Burden of male lower urinary tract symptoms (LUTS) suggestive of benign prostatic hyperplasia (BPH)- focus on the UKBJU Int 2015 115(4):508-19.10.1111/bju.1274524656222 [Google Scholar] [CrossRef] [PubMed]
[19]. Ernest A, Shahrad A, The Connected Catheter for management of Chronic Urinary Retention (CUR) in an adult male with neurogenic bladder- Case studyUrol Case Rep 2019 26:01-02.10.1016/j.eucr.2019.10094731297331 [Google Scholar] [CrossRef] [PubMed]
[20]. Andersson SO, Rashidkhani B, Karlberg L, Wolk A, Johansson JE, Prevalence of lower urinary tract symptoms in men aged 45-79 years: A population-based study of 40 000 Swedish menBJU Int 2004 94(3):327-31.10.1111/j.1464-410X.2004.04930.x15291861 [Google Scholar] [CrossRef] [PubMed]