Renal Vein Thrombosis in Idiopathic Thrombocytopenic Purpura
Subodh Kumar Das1, Debashis Routray2, Pradeep Narayan Sahoo3, Sukanto Kishore Das4, Sambit K Mohanty5
1 Surgeon, Department of Transplant and Renal Sciences, AMRI Hospitals, Bhubaneswar, Odisha, India.
2 Associate Consultant, Department of Urology and Renal Transplant, AMRI Hospitals, Bhubaneswar, Odisha, India.
3 Senior Consultant, Department of Medicine, AMRI Hospitals, Bhubaneswar, Odisha, India.
4 Senior Consultant, Department of Nephrology and Renal Transplant, AMRI Hospitals, Bhubaneswar, Odisha, India.
5 Senior Consultant, Department of Pathology, AMRI Hospitals, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Subodh Kumar Das, Director, Transplant and Renal Sciences, AMRI Hospitals, Bhubaneswar, Odisha, India.
E-mail: skdas_1_2000@yahoo.com
Renal Vein Thrombosis (RVT) is thrombotic occlusion of one or both main renal veins, resulting in acute or chronic kidney disease. The clinical presentation of RVT depends on the degree of venous occlusion. Of the various causes of RVT, Idiopathic Thrombocytic Purpura (ITP) is a rare occurrence. Use of thrombopoietin receptor agonists, corticosteroids, or splenectomy for the management of ITP may result in thromboembolism. Here, the present authors report a 23-year-old female with ITP who was on medication for the same (prednisolone 20 mg daily), presented with complaints of severe flank pain; ultrasonogram and CT scan revealed RVT. She was started with anticoagulant therapy but had no improvement, hence, she was planned for nephrectomy. The vein was ligated and divided with removal of the left kidney. Thus, while managing patients with ITP, it is important to consider the risk of thromboembolism.
Anticoagulant therapy, Corticosteroids, Thromboembolism
Case Report
A 23-year-old female presented in the emergency room with complaints of severe left flank pain with difficulty in breathing for three days and multiple episodes of nausea and vomiting. She had a history of Idiopathic Thrombocytopenic Purpura (ITP) for which she was receiving prednisolone 20 mg once a day, for one year. Family history was not relevant. Clinical examination did not reveal any significant positive findings.
On admission, the platelet count was low (62×103/μL), hence she was transfused with one-unit random donor platelets. She did not have proteinuria. The presence of Anti-Nuclear Anti-body (ANA), anti-double-stranded DNA (anti-dsDNA) was tested and was found negative. The patient was also tested for anti-phospholipid and anti-cardiolipin antibodies {both IgM (8.5 mg/dL) and IgG (7.4 mg/dL)}.
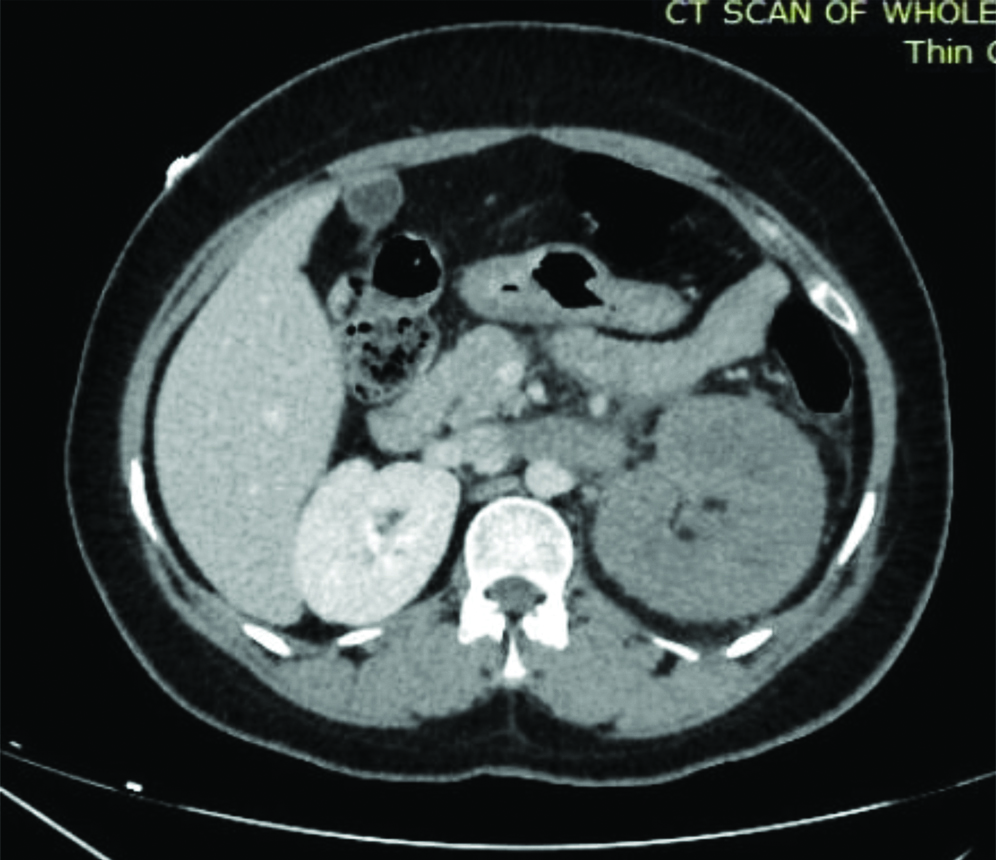
Chest X-ray was found to be normal. Ultrasound (USG) and Contrast-Enhanced Computed Tomography (CECT) were done on day one. USG revealed left main renal vein thrombosis. CT scan of the abdomen showed thrombosed renal vein with severe venous congestion of left kidney [Table/Fig-1]. After confirming renal vein thrombosis in both the reports, immediate anticoagulation therapy was started with heparin (5000 units of intravenous immediately followed by 5000 units 6-hourly) on Day 1. However, even after heparin infusion, patient complained of severe abdominal pain but there was no haematuria. She was given IV fluids, analgesics (tramadol), proton pump inhibitors, other than the anticoagulation therapy.
Computed tomography abdomen showing thrombus in the left renal vein.
On Day 3, USG KUB with renal doppler was advised, which showed a non-visualisation of left main renal vein and partial visualisation of intrarenal segmental vein. Partial recanalisation of thrombus in the intrarenal segmental veins was observed.
Thus, observing the progress of the disease in spite of heparin administration, a left side nephrectomy was planned on 4th day. Nephrectomy was done through a left sub-costal incision and transperitoneal approach. Kidney was found grossly enlarged and congested with dense adhesions all around. The renal vein was distended and completely occluded by the thrombus, filling the entire lumen and extending just short of the insertion of the vein into the Inferior Vena Cava (IVC). After ligating and dividing the artery, the vein was ligated and divided just close to its junction with the IVC. Rest of the procedure was performed subsequently and the kidney was removed.
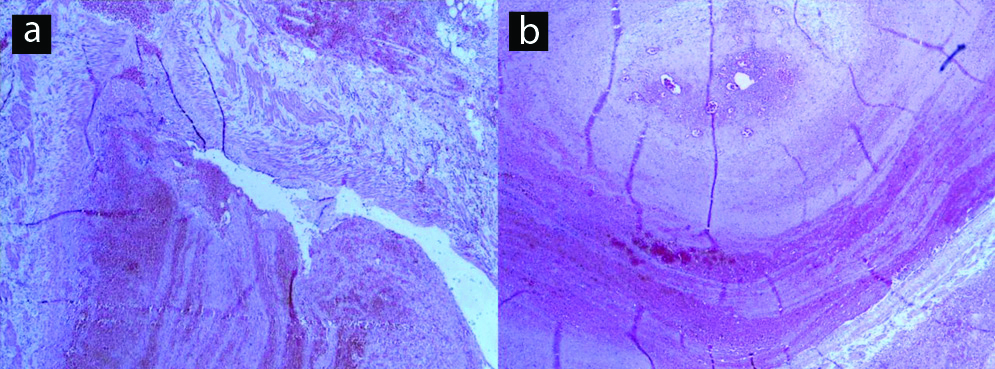
On post-operative Day 1, the platelet count was 100,000/mm3 and serum creatinine was 0.6 mg/dL. Post-surgical recovery was good and patient was clinically stable on subsequent follow-ups. Patient was on regular oral anticoagulants in the post-operative period. Histopathological examination confirmed recanalisation of thrombus in the renal vein [Table/Fig-2].
Recanalising thrombus in the renal vein (a) 4x HE and (b) 10x HE.
Discussion
Idiopathic Thrombocytopenic Purpura (ITP) is a hematologic disorder, characterised by thrombocytopenia without any known cause. The overall incidence of ITP has been reported to be around 5-10/1,00,000/year [1]. The major causes of excess platelet depletion include immune thrombocytopenia, decreased bone marrow production and increased splenic sequestration. Clinically, ITP may have an acute manifestation presenting with severe bleeding or could develop gradually with mild or no symptoms [2].
Use of thrombopoietin receptor agonists, corticosteroids, or splenectomy for the management of ITP may result in thrombo-embolism [3]. Around 8% of patients with ITP have thromboembolic events [4]. Renal Vein Thrombosis (RVT) is presence of thrombus in the major renal veins or their tributaries, which often starts in small intrarenal veins and subsequently extends to the major renal veins and occasionally to the IVC causing pulmonary embolism [5]. Thus, it is important to consider the risk of thromboembolic events while managing ITP. Here, the present authors presented a case of RVT caused probably due to ITP management which required left sided nephrectomy.
This report demonstrates the risk of thromboembolism in patients with ITP. There are few reports of thromboembolism in ITP patients. One such report was by Aledort LM et al., in which a total of 186 adult patients with ITP were reviewed and 81 (44%) patients were receiving ITP treatment and reported having 18 thrombotic/ischaemic events in 10 patients and two patients had pulmonary embolism [6]. In a study by Girolami A et al., 19 out of the 26 patients were on cortisone therapy for ITP during the occurrence of thrombotic events [7]. In this study, nine patients had venous thrombosis in which 7 were on cortisone therapy. In another study by Bussel JB et al., out of the 40 thromboembolic complications, 20 were in patients on cortisone therapy [8]. Though majority were deep vein or pulmonary thrombosis. Overall, oral corticosteroid use was associated with greater risk of venous thrombosis.
The most common causes of RVT are nephrotic syndrome, coagulatory disorders, renal tumours, infections or trauma [9,10]. No evidence of tumours or haematoma around kidney was observed on USG or CT abdomen. Since the index patient was a known cause of ITP with a low platelet count (62×103/μL) on admission the possibility of ITP being the cause for RVT was confirmed.
This patient was receiving prednisolone for ITP, which could have precipitated the renal thrombus formation. Another theory suggests that slow flow in the post-glomerular circulation increases the risk of thrombosis [11]. Hence, considering both the possibilities, development of RVT can be considered. The clinical presentation of RVT depends on the degree of venous occlusion.
Even in the index case, CT scan revealed thrombosis of the renal vein causing severe venous congestion of the left kidney. While performing nephrectomy, the renal vein was found to be distended and completely occluded by the thrombus filling the entire lumen. Since the occlusion was more, the severity was acute and needed surgical intervention for its management.
Management of renal vein thrombosis includes medical and surgical interventions. Medical management includes intravenous and oral anticoagulants in the form of heparin and warfarin. Few cases show inadequate or no response to anticoagulation therapy, for such cases mechanical or chemical thrombectomy is advised [12,13]. Commonly streptokinase or urokinase is the choice of thrombolytic agents which are percutaneously administered with the help of the catheter [14,15].
Conclusion(s)
This case highlights adequate monitoring during the treatment of Idiopathic Thrombocytopenic Purpura (ITP), as it might progress into thromboembolic changes, which may affect the brain, kidneys or lungs causing reversible changes.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 25, 2019
Manual Googling: Jan 24, 2020
iThenticate Software: Feb 11, 2020 (11%)
[1]. Cines DB, Bussel JB, How I treat idiopathic thrombocytopenic purpura (ITP)Blood 2005 106(7):2244-51.10.1182/blood-2004-12-459815941913 [Google Scholar] [CrossRef] [PubMed]
[2]. Kayal L, Jayachandran S, Singh K, Idiopathic thrombocytopenic purpuraContemp Clin Dent 2014 5(3):410-14.10.4103/0976-237X.13797625191085 [Google Scholar] [CrossRef] [PubMed]
[3]. Takagi S, Suzuki I, Watanabe S, Risk of thromboembolism in patients with immune thrombocytopeniaJ Hematol Thrombo Dis 2015 3(1):185 [Google Scholar]
[4]. Doobaree IU, Nandigam R, Bennett D, Newland A, Provan D, Thromboembolism in adults with primary immune thrombocytopenia: A systematic literature review and meta-analysisEur J Haematol 2016 97(4):321-30.10.1111/ejh.1277727199203 [Google Scholar] [CrossRef] [PubMed]
[5]. Wang Y, Chen S, Wang W, Liu J, Jin B, Renal vein thrombosis mimicking urinary calculus: A dilemma of diagnosisBMC Urol 2015 15:6110.1186/s12894-015-0054-126133978 [Google Scholar] [CrossRef] [PubMed]
[6]. Aledort LM, Hayward CPM, Chen MG, Nichol JL, Bussel J, ITP Study GroupProspective screening of 205 patients with ITP, including diagnosis, serological markers, and the relationship between platelet counts, endogenous thrombopoietin, and circulating antithrombopoietin antibodiesAm J Hematol 2004 76(3):205-13.10.1002/ajh.2010415224353 [Google Scholar] [CrossRef] [PubMed]
[7]. Girolami A, Berti de Marinis G, Bonamigo E, Treleani M, Vettore S, Arterial and venous thromboses in patients with idiopathic (immunological) thrombocytopenia: A possible contributing role of cortisone-induced hypercoagulable stateClin Appl Thromb Hemost 2013 19(6):613-18.10.1177/107602961245211410.1177/107602961245211422790661 [Google Scholar] [CrossRef] [CrossRef] [PubMed]
[8]. Bussel JB, Kuter DJ, Pullarkat V, Lyons RM, Guo M, Nichol JL, Safety and efficacy of long-term treatment with romiplostim in thrombocytopenic patients with chronic ITPBlood 2009 113(10):2161-71.10.1182/blood-2008-04-15007818981291 [Google Scholar] [CrossRef] [PubMed]
[9]. Singhal R, Brimble KS, Thromboembolic complications in the nephrotic syndrome: Pathophysiology and clinical managementThromb Res 2006 118(3):397-407.10.1016/j.thromres.2005.03.03015990160 [Google Scholar] [CrossRef] [PubMed]
[10]. Llach F, Papper S, Massry SG, The clinical spectrum of renal vein thrombosis: Acute and chronicAm J Med 1980 69(6):819-27.10.1016/S0002-9343(80)80006-4 [Google Scholar] [CrossRef]
[11]. Zubarev AV, Ultrasound of renal vesselsEur Radiol 2001 11(10):1902-15.10.1007/s00330010101211702122 [Google Scholar] [CrossRef] [PubMed]
[12]. Chen C, Li X, Huang L, Zhang J, Chen S, Ye H, Mechanical thrombectomy with intraoperative local thrombolysis versus mechanical thrombectomy with continuous thrombolysis for treatment of cerebral venous sinus thrombosis: A systematic review of 82 casesWorld Neurosurg 2019 125:489-97.e14.10.1016/j.wneu.2018.12.19330659973 [Google Scholar] [CrossRef] [PubMed]
[13]. Narayan SK, Elavarasi A, Endovascular interventional management of cerebral venous sinus thrombosisJ Stroke Med 2018 1(1):28-33.10.1177/2516608518774211 [Google Scholar] [CrossRef]
[14]. Rowe JM, Rasmussen RL, Mader SL, Dimarco PL, Cockett AT, Marder VJ, Successful thrombolytic therapy in two patients with renal vein thrombosisAm J Med 1984 77(6):1111-14.10.1016/0002-9343(84)90198-0 [Google Scholar] [CrossRef]
[15]. Salam TA, Lumsden AB, Martin LG, Local infusion of fibrinolytic agents for acute renal artery thromboembolism: Report of ten casesAnn Vasc Surg 1993 7(1):21-26.10.1007/BF020426558518115 [Google Scholar] [CrossRef] [PubMed]