Materials and Methods
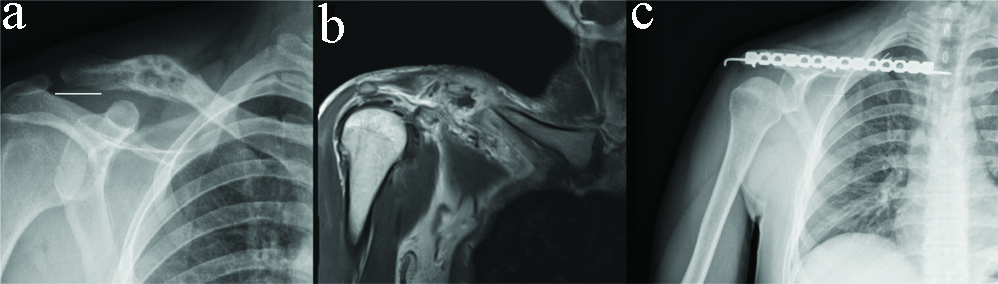
A retrospective study was conducted from January 2002 to December 2017 in a tertiary care hospital in which 15 patients with primary clavicular malignancy underwent claviculectomy with or without reconstruction were included. Local medical expertise and education board approved of the study protocol (meeting no: 85, meeting and decision date: 31.12.2019, retrospective). Exclusion criterion is being a patient with primary clavicular malignancy but not undergoing surgery (inoperable patients, patients who refused surgical treatment). The demographics and functional scores of the patients were obtained retrospectively from the patient archive files of hospital. There were nine males and six females with an average age of 44.8±24.1 years (range 2-87 year). The left clavicle was affected in 10 patients and right in 5 patients. Lesions were located in the lateral third of clavicle in 4 patients, in the middle third in 7, in the middle and lateral third in 3 and were global involvement in 1. The most common complaint was swelling. One patient presented with pathological fracture [Table/Fig-1]. All patients were initially investigated with plain radiographs and magnetic resonance imaging. As a result of radiological imaging, none of the patients had neurovascular involvement. All the biopsies were done by the open incisional technique. The average amount of tumour resection was 7.1±3.0 cm (range 2 to 14 cm) by considering the safe surgical margin. Twelve patients underwent partial clavicle resection and 1 patient underwent total clavicle resection. Two patients underwent reconstruction with allograft fibula after partial clavicle resection [Table/Fig-2]. The graft was prepared appropriately to reconstruct defect after resection of the tumour. Reconstruction plates and k-wires were used for graft stabilisation [Table/Fig-3]. Claviculectomy was performed over the subcutaneous surface of the clavicle and it included the biopsy incision. In all patients, the operated side was immobilised for 3 weeks with arm sling. All the patients were followed with two directional shoulder X-rays and physical examination once in the first 6 months and after that once in each 3 months.
A 63-year-old male patient with plasmacytoma. Anteroposterior radiograph of the patient presented with pathological fracture.

| Characteristic | Total n=15 |
|---|
| Age (year) |
| Mean±SD | 44.8±24.1 |
| Median (min-max) | 51.0 (2.0-87.0) |
| Sex | n (%)* |
| Female | 6 (40.0) |
| Male | 9 (60.0) |
| Location | n (%) |
| Middle | 7 (46.7) |
| Lateral | 4 (26.7) |
| Middle and lateral | 3 (20.0) |
| Global | 1 (6.7) |
| Histological findings | n (%) |
| Ewingsarcoma | 6 (40.0) |
| Plasmactyotama | 4 (26.7) |
| Malignant mesencymal tumour | 2 (13.3) |
| MultipleMyeloma | 2 (13.3) |
| Non Hodking lymphoma | 1 (6.7) |
| Clinical findings | n (%) |
| Swelling | 5 (33.3) |
| Pain | 4 (26.7) |
| Swelling+pain | 5 (33.3) |
| Swelling+pain+PathologicFracture | 1 (6.7) |
| Treatment | n (%) |
| Partial claviculectomy | 12 (80.0) |
| Total claviculectomy | 1 (6,7) |
| Partial claviculectomy+Fibuarallogreft | 2 (13.3) |
| Complication | n (%) |
| No | 11 (73.3) |
| Mild pain | 3 (20.0) |
| Wound problem | 1(6.7) |
| Resection amount (cm) |
| Mean±SD | 7.1±3,0 |
| Median (min-max) | 6.5 (3.0-14.0) |
| Exitus |
| No | 7 (46.7) |
| Yes | 8 (53.3) |
| Cure |
| No | 12 (80.0) |
| Yes | 3 (20.0) |
| Postoperative MSTS score (%) |
| Mean±SD | 63.1±14.1 |
| Median (min-max) | 67.0 (33.0-80.0) |
| Postoperative Constant-Murleyscore (%) |
| Mean±SD | 57.8±13.7 |
| Median (min-max) | 60.0 (30.0-74.0) |
| Postoperative UCLA score |
| Mean±SD | 20.8±6.8 |
| Median (min-max) | 21.0 (8.0-31.0) |
*Column percentage; SD: Standard deviation; MSTS: Musculoskeletal tumour society; UCLA: University of California-Los Angeles
a) Anteroposterior radiographs of 14-year-old male patient with Ewing’s sarcoma; b) Cortical destruction of bone with soft tissue component surrounding clavicle in magnetic resonance imaging; c) Reconstruction plates and k-wires were used for graft stabilisation after tumour resection.
The functional result of the upper limb was assessed with the Constant-Murley scores, International Society of Limb Salvage-MSTS evaluation system and the UCLA shoulder rating scale [7,8]. The functional status of patients was assessed at 6 months after surgery.
Statistical Analysis
Statistical analysis was performed by SPSS 22.0 (Chicago IL) computer program In statistical analysis, categorical variables were given as numbers and percentages, and continuous variables were presented with mean±standard deviation (SD) and median (min-max value) for descriptive analyses. The conformity of continuous variables to normal distribution was evaluated using visual (histogram and probability graphs) and analytical methods (Kolmogorov-Smirnov/Shapiro-Wilk tests). Normality analysis revealed that all data sets were not distributed normal distribution. Mann Whitney u test was used for comparison of data sets which were not normally distributed for the variables. Spearman correlation was used to test the association between resection amount and patient’s scale scores Correlation coefficient (rho) is the absolute value r≤0.30, it means there is a weak correlation, if r ranges from 0.30 to 0.50, it means there is a moderate correlation and if r≥0.50, it means there is a strong correlation [9]. Linear regression analyses were carried out to evaluate the association of resection amount with patients’ scale scores. These data are presented as ‘B Coefficients’. ≤0.05 was considered statistically significant.
Results
There were six Ewing’s sarcomas, four plasmocytomas, two multiple myelomas, two malignant mesenchymal tumours and one lymphoma. The mean follow-up period was 41 months (range 14 to 68 months). The clinical characteristics, treatment and outcomes of patients are summarised in [Table/Fig-2]. Five patients with lung metastasis died with disease and 3 patients died of disease on follow-up period. During the follow-up, non-union and infection developed the patient who reconstructed with allograft. Debridement was performed. While adjuvant chemotherapy protocol continuing, as the infection did not regress, implant and allograft extraction surgery was planned. However, the patient died of pulmonary metastasis and chemotherapy complications 1 year after surgery. Postoperatively, none of the patients had any neurological deficit. All patients except one older patient with a malignant mesenchymal tumour were enrolled in the adjuvant chemotherapy protocol. No local relapse occurred in the follow-up. In present study, the mean postoperative MSTS score was 63.1±14.1 (range, 33-80), the mean Constant-Murley score was 57.8±13.7 (range, 30-74) and the mean UCLA score was 20.8±6.8 (range, 8-31). In all series, as the amount of clavicle resection increased, the function scores were lower [Table/Fig-4]. A statistically significant and perfect negative correlation was found between resection amount and MSTS score (r=-0.907, p<0.001), Constant-Murley score (r=-0.910, p<0.001) UCLA score (r=-0.975, p<0.001). When the relationship between scores and the patient ages was evaluated, it was found that there was a bicorrelation only with Constant-Murley score. According to this, it was observed that as the age increased, so did the Constant-Murley score (r=0.515, p=0.050). It has been found that resection amount was significantly higher in the patients with complication than in the patients without complication (p=0.005), and MSTS score (p=0.014), Constant-Murley score (p=0.026) UCLA score (p=0.007) were significantly lower [Table/Fig-5].
Relationship between resection amount, age and scores.
| Resection amount | Age |
|---|
| N=14 | rs (p) | rs (p) |
|---|
| MSTS score | -0.907 (<0.001) | 0.400 (0.140) |
| Constant-Murley score | -0.910 (<0.001) | 0.515 (0.050) |
| UCLA score | -0.975 (<0.001) | 0.383 (0.159) |
rs: Spearman correlation of resection; MSTS: Musculoskeletal Tumour Society; UCLA: University of California-Los Angeles; rs: Spearman correlation of age
Evaluation of scores according to complication status.
| Complication No (n=11) | Complication Yes (n=4) | p-value |
|---|
| Age, year | | | 0.8441 |
| Median (min-max) | 54.0 (2.0-87.0) | 41.5 (20.0-75.0) | |
| Resection amount (cm) | | | 0.005 |
| Median (min-max) | 6.0 (3.0-7.5) | 11.0 (7.5-14.0) | |
| Postoperative MSTS score, % | | | 0.014 |
| Median (min-max) | 67.0 (53.0-80.0) | 43.0 (3.0-67.0) | |
| Postoperative Constant-Murley score, % | | | 0.026 |
| Median (min-max) | 62.0 (56.0-74.0) | 36.0 (30.0-61.0) | |
| Postoperative UCLA score | | | 0.007 |
| Median (min-max) | 23.0 (18.0-31.0) | 12.0 (8.0-19.0) | |
1Mann-Whitney U test; MSTS: Musculoskeletal tumour society; UCLA: University of California-Los Angeles
The relationship of all three scores with resection amount was evaluated with linear regression analysis in [Table/Fig-6] adjusted to age, sex, and complication state. Resection amount was associated with lower MSTS Score (B Coefficient=-4.40; p<0.001), Constant-Murley Score (B Coefficient=-4.39; p<0.001), and UCLA Score (B Coefficient=-2.94; p<0,.001). According to this, one unit increase in resection amount results in 4.4 units decrease in MSTS score, 4.4 units decrease in Constant-Murley score and 2.94 unit decrease in UCLA score, respectively.
Investigation of the effect of resection amount on scores by using linear regresion analyses.
| MSTS score | Constant-Murley score | UCLA score |
|---|
| B* coefficient | Adjusted R2 | p-value | B* coefficient | Adjusted R2 | p-value | B* coefficient | Adjusted R2 | p-value |
|---|
| Resection amount | -4.40 | 0.889 | <0.001 | -4.39 | 0.947 | <0.001 | -2.94 | 0.959 | <0.001 |
*Linear regression analyses adjusted for sex, age and complication for exploring the relation between resection amount and patients’ scale scores; MSTS: Musculoskeletal tumour society; UCLA: University of California-Los Angeles
Discussion
In contrast to other long bones, the clavicle is not formed by enchondral ossification; it ossifies from intramembranous ossification, such as the skull and facial bones. Also, clavicle contains scanty red marrow and it’s vascularisation is poor, so it’s a unique bone that is considered to be flat bone [1,10]. The clavicle is an uncommon location of bone tumours, and the incidence of the clavicular tumours has been reported less than 1% of all bone tumours [10-12].
In the literature, there are a very limited number of articles about primary malignant tumours of clavicle. Also, there is no study reporting the incidence of primary malignant tumours [12-15]. Cleeman E et al., reported that clavicle involvement constituted only 6% of cases in their study of primary tumours of the shoulder girdle only [16]. Myeloma and osteosarcoma are the most common primary malignant tumours [12,16]. Suresh S and Saifuddin A reported that they had no malignant lesion in any of the patients under 20 years of age in a series of 59 patients with clavicular tumoral and non-tumoral lesions [10]. They reported that inflammatory lesions (81.4%) and benign tumours (18.6%) were frequent in this age group and they said that all malignant tumours were 50 years or older. They reported that the medial third of clavicle was the most involved site in all patients (59%) and that they did not have any malignant lesions in this region. They stated that malignant lesions were most commonly located in the lateral third of the clavicle. Gersovich EO et al., also reported that primary solitary malignant tumours such as osteosarcoma, Ewing’s sarcoma and plasmocytoma were most commonly located in the lateral clavicle (41%) [3]. Kapoor S et al., in their series of 12 patients with benign and malignant tumours, they reported they had equal distribution in each region of the bone. They said diaphyseal involvement of clavicular tumours was rare in the literature [2]. In this series, none of the primary malignant lesions had medial clavicle involvement. The most common primary malignant tumour was Ewing’s sarcoma (40%). Contrary to the literature, the most common mid clavicle (46.6%) and later lateral clavicle (26.6%) were involved. The middle and lateral clavicle were affected in 20% of the patients. In this series, there were 6 patients aged 50 and under (40%). The number of patients with primary malignant tumours under 20 years of age was 4 (26.6%).
Post-traumatic conditions, Brown tumour and rare benign lesions may have the same clinical appearance as malignant clavicular lesions [1,17]. Approximately, 10% of the shoulder girdle tumours can be seen with no palpable mass and normal radiographic findings [1,18-20]. Clinical presentations of symptomatic patients can be non-specific, ranging from progressive swelling to painful shoulder movement restriction (like frozen shoulder). However, malignant tumours of clavicle generally appears with rapid progression, invasive growth and a bigger tumour size from the first development [4]. The most common complaint in this series was swelling. Five patients with both swelling and pain, 1 patient with only pain, and 1 patient with both swelling and pathological fracture were presented to our clinic.
Although several case reports have been published in the treatment of neoplastic lesions of the clavicle, the treatment of malignant primary tumours and level of claviculectomy are controversial [21-23]. Claviculectomy is a rare surgical procedure for various indications such as tumours, fracture nonunion, infection, and severe pain [11,14,24]. In 1986, Wood VE reported that the clavicle was an accessory bone and resection had minimal or no dysfunction [25].
Kapoor S et al., performed claviculectomy in 7 patients (3 total, 4 partial resection) without reconstruction in 12 patient series consisting of 4 benign and 8 malignant tumours [2]. They evaluated their functional scores according to the MSTS scoring system and reported a mean MSTS score of 70.5 and all patients were satisfied with the outcome. Although some authors stated that partial claviculectomy had not got any effect or had a very little effect on postoperative functional results, there are some authors reporting that clavicle resection was related with functional loss [10,14,15]. The amount of clavicle resection were measured in this study on the contrary of other studies. The relationship between clavicle resection with functional scores and complication occurrence was statistically evaluated. Patients with more clavicle resection had lower functional scores and this relationship was found to be statistically significant. It has been found that resection amount was significantly higher in the patients with complication than in the patients without complication. When similar studies in literature were analysed, no studies making statistical deduction was found [10,14,15]. Li J et al., performed claviculectomy in 5 patients in 11 primary and secondary clavicle malignancy series, and they reported that partial or total claviculectomy without reconstruction is rarely associated with the clinically loss of function of the clavicle [11]. Lewis MM et al., reported that patients who underwent radical resection in the clavicle may have limitations in shoulder abduction and flexion, but that these functions could be insignificant in the patient’s daily activities [14].
Many complications such as shoulder dropping, postoperative pain, limited motion of the shoulder joint, reduction of muscular strength, neurologic function deficit, and restriction of daily activities have been reported in the patients for which no reconstruction was made after resection of clavicle in the literature [4]. Rodriguez MJ et al., reported 5 patients with Ewing’s sarcoma managed by different surgical methods [15]. They concluded that good shoulder functions could be achieved without reconstruction after total claviculectomy. Wessel RN and Schaap GR did not reach a definitive conclusion due to the heterogeneity of their patients and the low number of patients [21]. However, in chronic cases of osteitis and malignancy, they obtained good results after claviculectomy in six patients. Krishnan SG et al., reported the results of has reported the results of the 6 patients who they performed total claviclectomy. They reported that a questionnaire study conducted by Rockwood had reported that claviclectomy was not a benign procedure and clavicle should be spared if possible. Moreover, they reported that functional results after total claviclectomy were acceptable however it was related to high rates of complications after claviclectomy in their cases [24].
Li J et al., in the series of 11 patients, 6 patients underwent reconstruction with allograft after claviculectomy [11]. Two of these patients had wound problems, 1 had allograft infection and 2 had non-union complications. They reported that the use of massive allografts in reconstructions after tumour resection had advantages in the protection of the neurovascular structures and cosmetic advantages, and suggested the use of allograft in especially low-grade tumours.
In present series, 2 patients underwent reconstruction after claviculectomy. One of the patients had wound site problem, infection and non-union [Table/Fig-7]. The worse results of this patient than that of the rest of the series may show that allograft usage in claviclectomy reconstruction in malignant tumours is not advantageous. The other 13 patients in the series underwent claviculectomy without reconstruction. Worse functional results than those in the literature were obtained as the size of the tumour and the amount of the clavicle resected increase. When the resection amount and functional outcome scores of patients included in the study were compared, an inverse correlation was observed between these two parameters. Therefore, early diagnosis and early surgery may provide better functional results by decreasing the amount of clavicle resection in patients with primary malignant tumours in clavicle.
A 32-year-old male patient with Ewing’s sarcoma. Shoulder functions of the patient that had reconstruction with allograft.

Limitation(s)
There were some limitations of this study. First of all, it was a retrospective analysis and the number of cases was small due to the rarity of the localisation for the tumour. For those reasons, the confidence of the results was not high. Studies with a high number of patients and with more centers are needed.
Conclusion(s)
Primary clavicular malignancies are extremely rare tumours with a poor prognosis. Also, because of the insidious onset, a high index suspicion is necessary to avoid misdiagnosis. On the contrary to the articles, it has been found that resection amount of the clavicle had affected shoulder functions according to the results of this study. Even though the shoulder functional scores were found to be low, patient’s daily activities were affected insignificantly. So, because of complications such as wound problems, infection and considering the cost-efficiency, it is not appropriate to use allograft reconstructions in this type of malignant tumours. This study confirmed that reconstruction after claviculectomy is unnecessary.
Contribution(s)
IBA: writing the paper, literature review; SY: data collection and references; AY: data collection and statistical analysis; GT: editing, analysis of the data; CU: study concept, interpretation of the data; YK: critical review.
*Column percentage; SD: Standard deviation; MSTS: Musculoskeletal tumour society; UCLA: University of California-Los Angeles
rs: Spearman correlation of resection; MSTS: Musculoskeletal Tumour Society; UCLA: University of California-Los Angeles; rs: Spearman correlation of age
1Mann-Whitney U test; MSTS: Musculoskeletal tumour society; UCLA: University of California-Los Angeles
*Linear regression analyses adjusted for sex, age and complication for exploring the relation between resection amount and patients’ scale scores; MSTS: Musculoskeletal tumour society; UCLA: University of California-Los Angeles