Pancreatic Plasmacytoma Misdiagnosed as Neuroendocrine Tumour: A Pathologist’s Dilemma
Sakthisankari Shanmugasundaram1, Umamaheswari Gurusamy2, Prasanna N Kumar3, Biku Joseph John4
1 Assistant Professor, Department of Pathology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
2 Associate Professor, Department of Pathology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
3 Professor, Department of Pathology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
4 Professor, Department of Hepatobiliary and Pancreatic Surgery, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sakthisankari Shanmugasundaram, Peelamedu, Coimbatore, Tamil Nadu, India.
E-mail: sakthissankari@gmail.com
Extramedullary plasmacytomas are rare, constituting to about 5% of plasma cell neoplasms. Pancreatic involvement is uncommon constituting to about 2.3%. Localised solitary plasmacytomas has a good response to radiation. When they are associated with pre-existing multiple myeloma, their prognosis is poor. A case of plasmacytoma of pancreas presenting with obstructive jaundice preceding plasma cell leukaemia is presented here. The lesion was misdiagnosed by fine needle aspiration cytology as neuroendocrine neoplasm. The patient did not present with symptoms of myeloma initially. The present case highlights the significance of considering other causes of pancreatic mass than primary carcinomas.
Extramedullary plasmacytoma, Pancreatic neoplasm, Plasma cell leukaemia
Case Report
A 62-year-old female patient presented with complaints on and off fever from past 15 days. A vague, non-radiating, intermittent paraumbilical pain in right upper quadrant, and vomiting from past five days. There was no history of gastrointestinal bleed, loss of weight and loss of appetite. She was a known hypertensive and diabetic for five years and was on treatment with oral hypoglycemics and antihypertensives. Her vitals were within normal limits and there was no organomegaly.
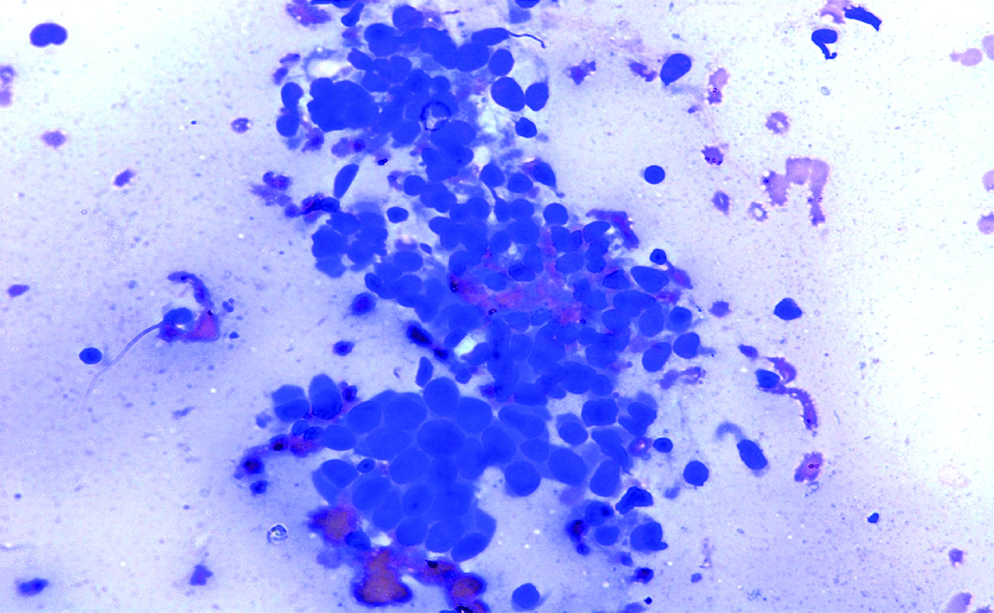
Ultrasound abdomen showed a hypoechoic mass in the pancreatic head dilating the main pancreatic duct. Computed Tomography (CT) revealed an isodense mass lesion with well defined borders in the head of pancreas measuring 4.8×5.5 cm [Table/Fig-1]. Acoustic Radiation Force Impulse (ARFI) elastography showed mean shear velocity of 3.6. The provisional diagnosis included primary pancreatic tumour. Endoscopic Ultrasound Guided Fine Needle Aspiration Cytology (EUS-FNAC) was planned for the evaluation of the pancreatic mass. EUS showed a 3×3.1 cm iso and hypoechoic mass in the head of pancreas with dilated common bile duct measuring 9 mm in the suprapancreatic portion. Dilated main pancreatic duct (6.5 mm) distal to the mass in the pancreas was identified. Visualised tail of pancreas and portal vein appeared normal. Cytological examination of the mass showed sheets and scattered plasmacytoid cells suspicious of a neuroendocrine neoplasm [Table/Fig-2].
CT scan showing isodense lesion in head of pancreas.

Cytology smears showing plasmacytoid cells (40x).
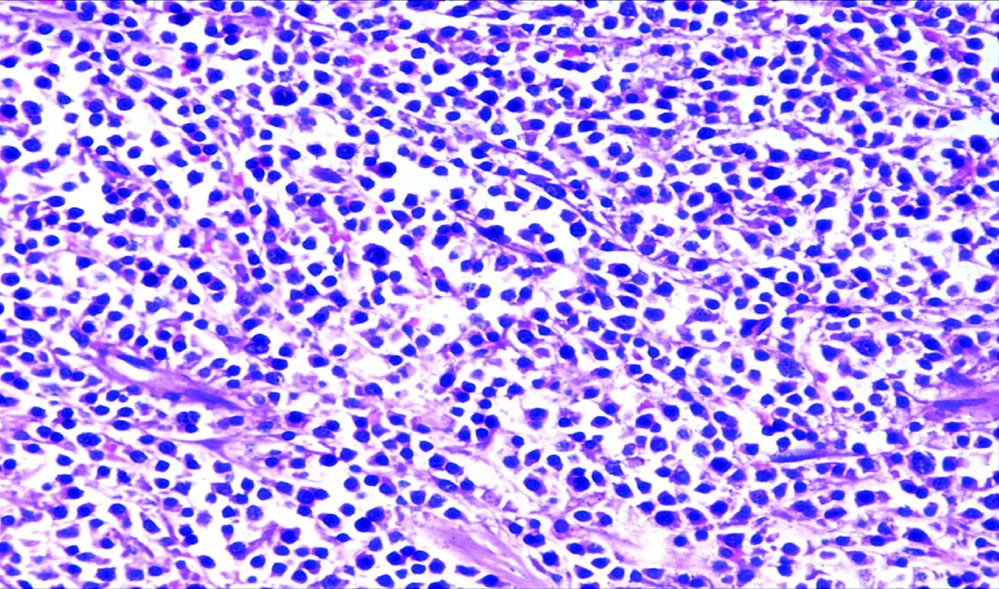
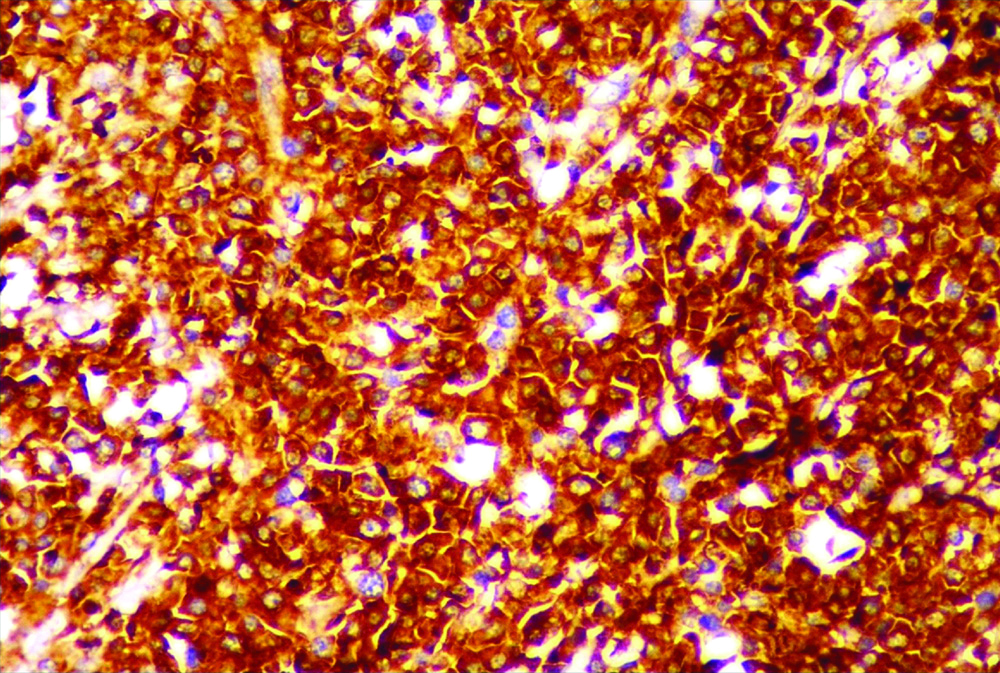
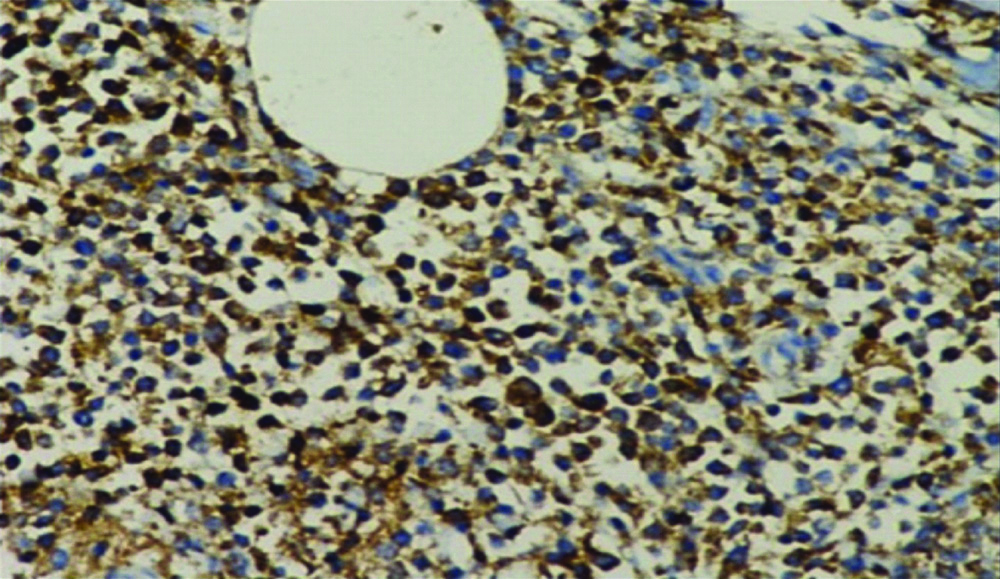
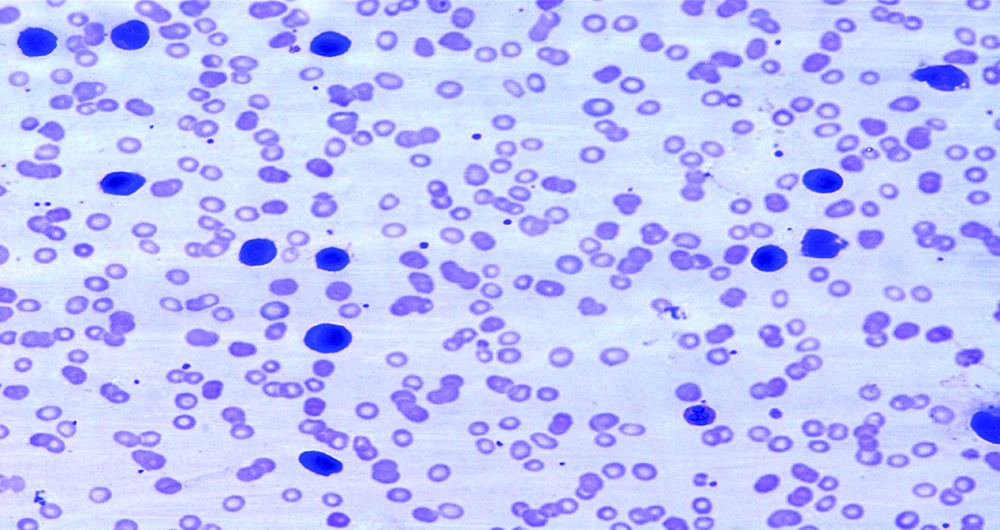
Whipple resection was done with a clinical and cytological diagnosis of a pancreatic neuroendocrine tumour. Pancreas showed an ill-defined mass occupying the head [Table/Fig-3]. Haematoxylin & Eosin (H&E) sections of the mass showed a diffusely infiltrating neoplasm composed of monotonous, plasmacytoid cells infiltrating the acini and ducts [Table/Fig-4]. Few binucleate and multinucleate plasma cells and lymphocytes were present. Morphological differential diagnosis included plasmacytoma and lymphoplasmacytic lymphoma. Immunohistochemical staining was done for confirmation of diagnosis. The tumour cells showed strong membranous positivity for CD138 [Table/Fig-5], CD45 and selective Kappa staining [Table/Fig-6]. They were negative for CD20 and Lambda immunostains. A diagnosis of Plasmacytoma was made and radiological and biochemical workup for multiple myeloma was suggested. Protein electrophoresis was normal. Urine was negative for Bence Jones Protein. Serum calcium and renal parameters were normal. CT spine survey did not reveal any osteolytic lesions. The case was treated as a solitary extramedullary plasmacytoma and follow-up was suggested. A month later, the patient developed severe anaemia (Hb-6.8 g/dL). Total count was elevated and peripheral smear showed 40% plasma cells suggestive of plasma cell leukaemia [Table/Fig-7]. Reviewing the patient’s peripheral smear and complete haemogram taken a month back, there was normocytic normochromic anaemia and no demonstrable plasma cells in peripheral smear. ESR was elevated (93 mm/hr). Bone marrow aspiration done showed infiltration by sheets of immature and mature plasma cells. On immunohistochemistry, these cells showed kappa restriction. A diagnosis of plasma cell leukaemia was made. Investigations done at presentation and a month later are tabulated [Table/Fig-8]. The patient was referred to higher centre for further treatment.
Whipple’s specimen showing ill-defined lesion in pancreas.

Diffuse infiltration by plasma cells (H&E, 40x).
Strong membranous expression of CD138 by tumour cells (IHC, 40x).
Neoplastic cells with kappa expression (IHC, 40x).
Peripheral smear with plasma cell leukaemia (40X).
Biochemical and haematological investigations.
| Parameters | At initial presentation | A month later |
|---|
| Serum urea | 42 mg/dL | 81 mg/dL |
| Serum creatinine | 1.06 mg/dL | 3.82 mg/dL |
| Direct bilirubin | 3.3 mg/dL | 1.8 mg/dL |
| Haemoglobin | 9.5 g/dl | 6.8 g/dL |
| Total WBC count | 4.3×103/μL | 30.5×103/μL |
| Peripheral smear | Normocytic anaemia | Plasma cell leukaemia |
| Serum calcium | 1.116 mmol/L | 1.178 mmol/L |
Discussion
Plasma cell neoplasms include Plasma Cell Myeloma (PCM) which includes smouldering myeloma, non-secretory myeloma, plasma cell leukaemia and plasmacytoma which includes solitary bone and extraosseous plasmacytoma. In majority of the patients with PCM, features of end organ damage in the form of one or more of the following, hypercalcaemia, Renal insufficiency, Anaemia, and Bone lesions (CRAB) are present. The clonal proliferation usually begins in bone marrow. Renal failure occurs due to tubular damage caused by excessive synthesis of monoclonal immunoglobulins [1]. It constitutes 10 to 15% of haematological malignancies. Median age at diagnosis is 66 years [2]. The clinical spectrum varies from asymptomatic to highly aggressive.
Extramedullary Plasmacytomas (EMPs) are localised proliferation of monoclonal plasma cells forming solitary lesions outside the bone marrow. EMPs can be a manifestation of advanced multiple myeloma or can represent a solitary plasmacytoma without involving the bone marrow [3]. EMPs are uncommon and represent 5% of all plasma cell tumours. The most frequent site of involvement being upper respiratory tract followed by gastrointestinal tract and reticuloendothelial system [2].
Primary pancreatic plasmacytoma is rare constituting 2.3% of EMPs. Majority of the reported pancreatic plasmacytoma are secondary [3]. EMPs have the median age of presentation at 55 years (A decade younger than patients with multiple myeloma) and the majority (three-fourths) are males [4].
Most of these lesions are located in the pancreatic head. Diffuse enlargement and presenting as mass in body (4 cases) [5] and tail of the pancreas have also been reported. The typical presenting symptoms include abdominal pain and obstructive jaundice from bile duct compression when there is involvement of head. Diffuse lesions are picked up rather late as they tend to be asymptomatic [6]. The case presented here also had obstructive jaundice raising a concern for primary pancreatic carcinomas [7].
Radiologically plasmacytoma is characterised by a homogenously enhancing multilobular, solid mass on CT, which is non-specific and resemble that of neuroendocrine tumours or carcinoma [6]. The case described presented as an isodense lesion in the pancreatic head. Differentiating plasmacytomas radiologically from other pancreatic tumours is challenging.
Endoscopic Ultrasound (EUS) is a well recognised technique for confirmation of pancreatic masses by histology. EUS- FNAs are reported to have an accuracy of 78-95% in the diagnosis of pancreatic masses. Neuroendocrine tumour presents as a, homogeneous, isoechoic or hypoechoic mass on EUS while plasmacytoma shows heterogenecity with uneven margins. NETs are hypervascular [5,8].
When FNA was done, the lesion was morphologically misdiagnosed as neuroendocrine neoplasm since both share plasmacytoid morphology. In a rare site, one would be more likely to suspect a primary lesion with plasmacytoid features, particularly endocrine neoplasm. Islet cell tumours have been reported to be a great mimic of plasmacytoma with regards to clinical, cytological and radiological appearance [9]. EUS guided core biopsy from the lesion and immunophenotyping with cytokeratin for carcinoma and CD138, kappa and lambda for identifying monoclonality of plasma cells would have helped in arriving at the diagnosis. EUS guided FNA also serves as a platform for obtaining material for flow cytometry.
The patient described here did not present with any symptoms pertaining to myeloma prior to surgery. The patient progressed to plasma cell leukaemia within a short time (one month) which is evident from the investigations [Table/Fig-8]. Plasma cell leukaemias are primary in 60-70% of cases and secondary to multiple myeloma in 30-40 % cases [10,11].
To our knowledge, this is the first case of plasmacytoma of pancreas being the initial manifestation of a plasma cell leukaemia. Two other cases of plasma cell leukaemia have been reported in association with gastric plasmacytoma. One case reported also had a normal WBC and platelet count with normocytic normochromic anaemia three weeks prior to the diagnosis of gastric plasmacytoma. The authors had hypothesised that secondary plasma cell leukaemia would have occurred as a result of rapid transformation of possibly underdiagnosed light chain multiple myeloma. The present case could also represent a similar rapid transformation from a non-secretory myeloma presenting with an extramedullary plasmacytoma [12].
From the previous reports it is clear that in any mass lesion of a solid organ in a patient with multiple myeloma the possibility of secondary plasmacytoma is to be considered [3,4,7]. Present case in addition highlights the fact that plasmacytoma is to be considered when plasmacytoid cells are identified in EUS-FNAs even when previous diagnosis of myeloma or symptoms pertaining to myeloma is not there at presentation. Immunocytochemistry can be used as an ancillary technique to diagnose with certainty in such cases. Presurgical diagnosis is essential as the management varies between primary pancreatic carcinoma and plasmacytoma.
Conclusion(s)
This case highlights the importance of considering other causes of pancreatic head mass than a primary carcinoma in a patient with obstructive jaundice. It also emphasises the fact that pathologists must be aware of the existence of pancreatic plasmacytoma as initial manifestation of myeloma despite its rarity, a high index of suspicion being essential.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 22, 2019
Manual Googling: Jan 10, 2020
iThenticate Software: Jan 27, 2020 (5%)
[1]. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (Revised 4th edition) 2017 LyonIARC [Google Scholar]
[2]. Pallavi R, Ravella PM, Popescu MA, An unusual pancreatic mass: A case report and literature reviewTransl Gastrointest Cancer 2014 3:106-10. [Google Scholar]
[3]. Hue SSS, Azhar K, Plasmacytoma of the pancreas: An unusual manifestation of multiple myelomaSingapore Med J 2013 54:105-07.10.11622/smedj.201306623716161 [Google Scholar] [CrossRef] [PubMed]
[4]. Padda MS, Milles T, Adeniran AJ, Mahootic S, Aslaniana HR, Pancreatic and gastric plasmacytoma presenting with obstructive jaundice, diagnosed with endoscopic ultrasound-guided fine needle aspirationCase Rep Gastroenterol 2010 4:410-15.10.1159/00032105021060710 [Google Scholar] [CrossRef] [PubMed]
[5]. Lu T, Pu H, Zhao G, Primary pancreatic plasmacytoma: A rare case reportBMC Gastroenterol 2017 17:16710.1186/s12876-017-0729-z29262780 [Google Scholar] [CrossRef] [PubMed]
[6]. Smith A, Hal H, Frauenhoffer E, Extramedullary plasmacytoma of the pancreas: A rare entityCase Reports in Radiology 2012 2012:79826410.1155/2012/79826422720182 [Google Scholar] [CrossRef] [PubMed]
[7]. Williet N, Dumas O, Rinaldi L, Difficult endoscopic diagnosis of a pancreatic plasmacytoma: Case report and review of literatureWorld Journal of Clin Oncolog 2017 8:91-95.10.5306/wjco.v8.i1.9128246589 [Google Scholar] [CrossRef] [PubMed]
[8]. Kim JH, Paik WH, Joo M, Kim JG, Kim JW, Bae WK, Extramedullary plasmacytoma mimicking pancreatic cancer: A case report and literature reviewEndosc Ultrasound 2017 6:269-72.10.4103/2303-9027.19092328663530 [Google Scholar] [CrossRef] [PubMed]
[9]. Dodd LG, Evans DB, Symmans F, Katz RL, Fine-needle aspiration of pancreatic extramedullary plasmacytoma: Possible confusion with islet cell tumourDiagn Cytopathol 1994 10:371-75.10.1002/dc.28401004177924813 [Google Scholar] [CrossRef] [PubMed]
[10]. Singh S, Rath A, Yadav S, Primary plasma cell leukaemia-Case report and review of the literatureSultan Qaboos University Med J 2018 18(3):397-401.10.18295/squmj.2018.18.03.02430607287 [Google Scholar] [CrossRef] [PubMed]
[11]. Jain AG, Faisal-Uddin M, Khan AK, Wazir M, Shen Q, Manoucheri M, Plasma cell leukaemia-one in a million: A case reportWorld J Clin Oncol 2019 10(3):161-65.10.5306/wjco.v10.i3.16130949445 [Google Scholar] [CrossRef] [PubMed]
[12]. Puria A, Laua M, Zhaoa X, Chana K, Badera K, A rare case of a minimally secretory pasma cell leukaemia with a haemorrhagic gastric plasmacytomaLeukaemia Research Reports 2018 9:23-27.10.1016/j.lrr.2018.01.00129892544 [Google Scholar] [CrossRef] [PubMed]