Pyonephrosis Drainage Failure with Two Ureteric Stents in a Paediatric Patient
Gautamram Choudhary1, Pritesh Jain2, Prateek Gupta3, Likhiteswar Pallagani4
1 Associate Professor, Department of Urology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
2 Senior Resident, Department of Urology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
3 Senior Resident, Department of Urology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
4 Senior Resident, Department of Urology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prateek Gupta, Senior Resident, Department of Urology, All India Institute of Medical Sciences, Jodhpur-342005, Rajasthan, India.
E-mail: prateekgupta8@gmail.com
For obstructed uropathy causing pyonephrosis, immediate decompression by urinary diversion is the temporary mode of treatment. The type of procedure should be individualised depending on the size and position of stone, the degree of obstruction and the definite treatment planned for the obstruction in the near future. Percutaneous Nephrostomy (PCN) and retrograde Double J (DJ) stenting are the most widely used methods. According to currently available literature, there is no significant difference between these procedures with regards to availability, technical success, percentage of complications and the effect on quality of life of patients. Here, the authors present a case of a six-year-old male where internal drainage with two DJ stents did not drain the pyonephrosis. He had a right flank pain and fever on evaluation; was found to have right renal pelvic calculus with pyonephrosis. Even after putting two double J stent of size 3.6 French (Fr) the pyonephrosis could not be drained, eventually, right PCN of 6 Fr was placed, symptoms relieved and later on stone cleared with percutaneous nephrolithotomy.
Nephrolithotomy, Percutaneous nephrostomy, Pyonephrosis, Urinary diversion
Case Report
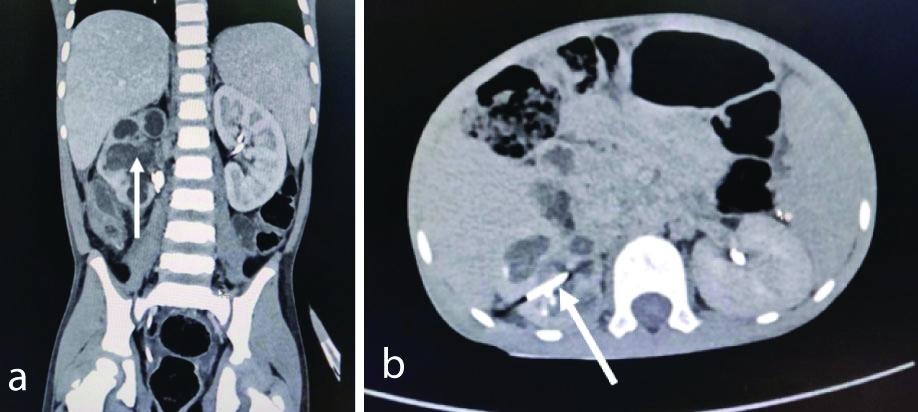
A six-year-old male presented with complaints of pain in abdomen, fever and oliguria for one month. No significant history of similar complaint, family history or drug history was noted. Physical examination showed no abnormality. The laboratory findings revealed total leucocytes count to be 13,100/mm3 and urine microscopy showed 60-70 pus cells and bacteria. Ultrasonography (USG) of the abdomen stated moderate to gross hydronephrosis in the right kidney with internal echoes and a 13.9 mm calculus in the renal pelvis, 4.1 mm in the middle calyx and 3.1 mm in the lower calyx. As per norms of department, a written informed consent was taken thus patient was planned for further intervention. For urinary diversion, a right PCN insertion was attempted by the radiologist but the procedure failed. Hence, a 3.6 Fr Double J (DJ) stent was placed for diversion and relief of symptoms. On reviewing one week after DJ stent insertion, fever and pain persisted and USG revealed a 6 cm × 1.8 cm perinephric collection (probably formed post-PCN attempt), 13 mm calculi and pyonephrosis. After a week, another 3.6 Fr DJ stent was placed on same side with aspiration of around 40 mL of perinephric fluid. In spite of two DJ stents draining the kidney, patient still had a fever with persistently increasing leucocyte count. He was on antibiotics according to culture report and also received antipyretics. Computed Tomography (CT) urography revealed right 10 mm × 5 mm calculus at the pelvic ureteric junction with pyonephrosis and a perinephric collection of 6 cm × 3.4 cm [Table/Fig-1a,b]. Kidney was excreting contrast, hence considered functional. A week later, right-sided USG guided 6 Fr PCN was placed under fluoroscopy guidance by a posterior middle calyx puncture [Table/Fig-2]. Pus was drained and the symptoms subsided within 48-hours. PCN output per day varied from 800-1200 mL/day with a calculated GFR of right kidney ~45 mL/minute which was normal. After a month, right Percutaneous Nephrolithotomy (PCNL) was done and a single 1 cm impacted stone at the PUJ was removed after dilating the tract with 24 Fr. Thus, a complete endoscopic and fluoroscopic clearance was ensured and we could salvage the kidney.
Computed Tomography (CT) urography showing calculus at the pelviureteric junction with pyonephrosis.
Anteroposterior view of X-ray Abdomen Kidney Ureter Bladder (KUB)- showing two DJ stents and one PCN tube in situ.

Discussion
Obstructive uropathy is the major cause for developing pyonephrosis and can pose to be a major life-threatening situation and is temporarily managed via DJ stenting or PCN or open drainage of the kidneys [1]. There are no specific guidelines regarding the ideal diversion method. DJ stenting and PCN are the most widely used [2]. Both have different success and failure rates, have their share of complications like DJ stents are related to irritative bladder symptoms and septicemia; while PCN is known to cause perforation, bleeding and blockage and have different impacts on quality of life and financial burden [3]. According to the available published studies, there is mixed evidence and sometimes no significant difference between these two techniques was reported, to prove which should be termed as better over other [3-5]. Contrary to this, the index case showed failure of DJ stent in relieving pyonephrosis for which later PCN was required.
Obstructive uropathy can be a life-threatening condition if not relieved immediately as it may cause temporary or permanent loss of renal function. In pyonephrosis, there is suppurative destruction of the renal parenchyma due to the infected hydronephrosis as a result of obstruction to urine flow. However, it is not clear as to which method is better as primary management for pyonephrosis. Pearle MS et al., had reported one such study on 42 patients. But no significant difference was seen in the time for complete drainage, clinical parameters such as leucocyte count and fever returning to normal range or the duration of hospital stay (4.5 days in PCN and 3.2 days in the ureteric catheter). The only significant difference was in the cost of the procedure since ureteric catheterisation required general anaesthesia it was double the cost of PCN [3]. In another study done by Mokhmalji H et al., on 40 patients requiring decompression for hydronephrosis, there were no cases of failure to access in PCN group whereas 4 cases failed in DJ stent group. The main study outcome was to access the quality of life; it was observed that patients in stent group required more analgesics while 75% of cases required intravenous antibiotics as compared to stent group (66%). Hence proposing that PCN is better than stent insertion based mainly on pain and more discomfort in stented group [6].
Yoshimura K et al., conducted a retrospective study to determine the outcome in patients requiring treatment for infective hydronephrosis along with upper ureteric calculi. As per the outcome parameters, there was no significant difference between the PCN and stent group on the basis of the systemic inflammatory response. However, it was observed that stones were significantly larger (9.7 mm) in PCN group as compared to the stent group (2.6 mm) [7]. In a study reported by Rammohan T et al., there was no statistically significant difference in time to clinical improvement but he concluded that the choice of selecting the procedure is differed as per the individual case, and it depends on the size and location of the stone. He also stated that if PCNL would be required for the stones, those cases must be best managed with PCN. Whereas, if ureteral stones require shock wave lithotripsy, then they can be better managed with stent insertion [8].
Mechanism of drainage by DJ stent is intraluminal and periluminal and after putting 2 DJ periluminal drainage must have improved; however, this did not happen maybe because of thick pus or stone compressing tube so DJ stents may not have worked. When a 6 Fr PCN was inserted an adequate drain was achieved which relieved the symptoms. Later a right PCNL complete clearance was achieved.
Thus, managing each case is different and requires treatment specific to it. The decision to choose the procedure for temporary decompressing the obstruction should be based on the degree and site of obstruction and the final intervention that would be provided in the near future.
Conclusion(s)
This case report concludes that percutaneous nephrostomy is a better method for temporary decompression of the pyonephrosis caused due to obstructive uropathy and also facilitated PCNL later. But since our findings are based on a single case, it is not a definitive hypothesis. The choice of the procedure should be based on the size and location of the stone and the degree of obstruction.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 28, 2019
Manual Googling: Jan 25, 2019
iThenticate Software: Jan 29, 2020 (5%)
[1]. Ahmad I, Pansota MS, Tareq M, Saleem MS, Tabssum SA, Hussain A, Comparison between Double J (DJ) ureteral stenting and Percutaneous Nephrostomy (PCN) in obstructive uropathyPJMS 2013 29(3):725-29.10.12669/pjms.293.356324353616 [Google Scholar] [CrossRef] [PubMed]
[2]. Naeem M, Jan MA, Ullah A, Ali L, Khan S, Haq AU, Percutaneous nephrostomy for therelief of upper urinary tract obstruction: An experience with 200 casesJPMI 2010 24(2):147-52. [Google Scholar]
[3]. Pearle MS, Pierce HL, Miller GL, Summa JA, Mutz JM, Petty BA, Optimal method of urgent decompression of the collecting system for obstruction and infection due to ureteral calculiJ Urol 1998 160(4):1260-64.10.1016/S0022-5347(01)62511-4 [Google Scholar] [CrossRef]
[4]. Goldsmith ZG, Oredein-McCoy O, Gerber L, Bañez LL, Sopko DR, Miller MJ, Emergent ureteric stent vs percutaneous nephrostomy for obstructive urolithiasis with sepsis: Patterns of use and outcomes from a 15-year experienceBJU Int 2013 112(2):E122-28.10.1111/bju.1216123795789 [Google Scholar] [CrossRef] [PubMed]
[5]. Shoshany O, Erlich T, Golan S, Kleinmann N, Baniel J, Rosenzweig B, Ureteric stent versus percutaneous nephrostomy for acute ureteral obstruction-clinical outcome and quality of life: A bi-center prospective studyBMC Urol 2019 19(1):7910.1186/s12894-019-0510-431455309 [Google Scholar] [CrossRef] [PubMed]
[6]. Mokhmalji H, Braun PM, Portillo FJM, Siegsmund M, Alken P, Kohrmann KU, Percutaneous nephrostomy versus ureteral stents for diversion of hydronephrosis caused by stones: A prospective, randomised clinical trialJ Urol 2001 165(4):1088-92.10.1016/S0022-5347(05)66434-8 [Google Scholar] [CrossRef]
[7]. Yoshimura K, Utsunomiya N, Ichioka K, Ueda N, Matsui Y, Terai A, Emergency drainage for urosepsis associated with upper urinary tract calculiJ Urol 2005 173(2):458-62.10.1097/01.ju.0000150512.40102.bb15643207 [Google Scholar] [CrossRef] [PubMed]
[8]. Rammohan T, Pandurang RK, Prasad DVS, Srinivas S, Santhosh B, Sudharshan G, A comparative study of percutaneous nephrostomy versus DJ stenting in infective hydronephrosis in calculous diseaseJEMDS 2015 4(18):3143-53.10.14260/jemds/2015/455 [Google Scholar] [CrossRef]