Laterally Closed Tunnel Approach with A-PRF for Isolated Miller’s Class II Gingival Recession: A Case Report
Mary Jose Nisha1, Nalina Kumari Burnice2, Kumar S Ashok3, Mahendra Jaideep4, Rajaram Vijayalakshmi5
1 Postgraduate Student, Department of Periodontology, Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
2 Assistant Professor, Department of Periodontology, Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
3 Associate Professor, Department of Periodontology, Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
4 Professor, Department of Periodontology, Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
5 Associate Professor, Department of Periodontology, Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Nalina Kumari Burnice, Department of Periodontology, Faculty of Dentistry, Meenakshi Ammal Dental College, Meenakshi Academy of Higher Education and Research, Chennai, Tamil Nadu, India.
E-mail: dr_burnice@yahoo.co.in
The displacement of the gingival margin below the level of Cementoenamel Junction (CEJ) is referred to as gingival recession. The main indication to treat isolated gingival recession is to increase soft tissue thickness and stability to facilitate plaque control, improve the patient aesthetics and prevent further periodontal breakdown. Though various root coverage techniques are available with numerous regenerative materials, autologous material such as Advanced Plasma Rich Fibrin (A-PRF) along with latest approach by Laterally Closed Tunnel (LCT) technique has been used in present case report as a predictable approach for the treatment of isolated gingival recessions.
Advanced plasma rich fibrin, Periodontal regeneration, Root coverage
Case Report
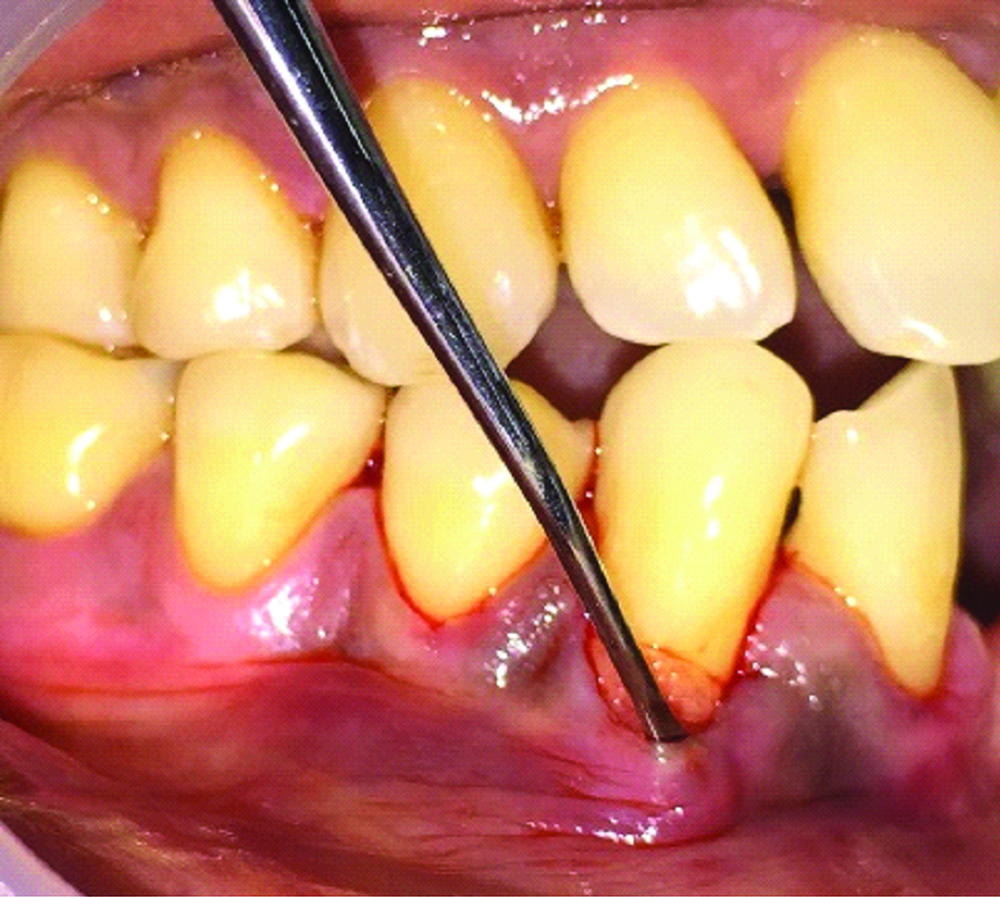
A 47-year-old healthy male patient reported to the department of Periodontology, with the chief complaint of sensitivity in his lower right front tooth region for past one month [Table/Fig-1a]. On clinical examination, gingival recession was noticed in relation to 43. Diagnosis was made as Miller’s class II gingival recession. Following which treatment plan was explained to the patient. Written informed consent was obtained from the patient before starting the surgical root coverage procedure.
a) Preoperative photograph of 43 Presurgical Protocol; b) Recession depth in relation to 43; c)Recession width in relation to 43.

At baseline all clinical parameters such as Oral Hygiene Index (OHI), Plaque Index (PI), Recession Width (RW), Recession Depth (RD), thickness of keratinised Gingiva (KGT), Probing Pocket Depth (PPD), Clinical Attachment Loss (CAL) were recorded. OHI and PI score was 1.8 and 1.2 respectively which was considered to be fair. Measurements of RD, RW, KGT, PPD, and CAL were 4 mm, 5 mm, 1 mm, 1 mm and 5 mm, respectively [Table/Fig-1b,c]. Radiographic examination revealed no bone loss [Table/Fig-2]. The nonsurgical therapy such as scaling and root planing was done, oral hygiene instructions were given to the patient. After three weeks patient was recalled, and thorough clinical examination was done. The gingiva in the region of 43 was found to be healthy without any inflammation.
Preoperative radiograph of 43.
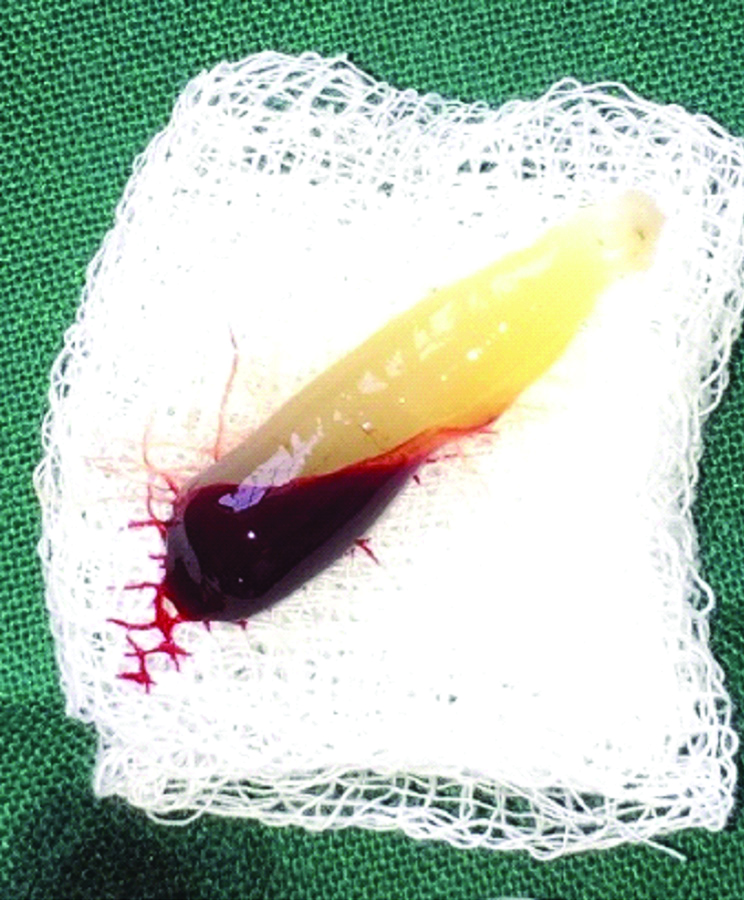
Preparation of A-PRF
The presurgical preparation was done where 10 mL intravenous blood was taken from the patient and centrifuged at 1500 RPM for 14 min at 18°C to prepare A-PRF [Table/Fig-3]. After centrifugation the test tube was examined. The test tube contained a buffy coat or a fibrin clot in the test tube after centrifugation was removed, A-PRF membrane was prepared by using PRF box and rest of the contents was discarded [1].
Surgical Procedure
Proper isolation of the surgical field was done and the surgical site (43) was administered with local anaesthesia by local infiltration of 1:80,000 lidocaine with adrenaline. Initially, a beveled intrasulcular incision was given through the gingival margin of the teeth in relation to 43 with gingival recession using a No. 15 blade [Table/Fig-4] and care was taken not to involve the tip of the interdental papilla. A mucoperiosteal pouch was created using tunneling instrument which extended beyond the mucogingival junction so as to reduce the tension of the flap and to approximate the lateral flaps over the denuded root surface [Table/Fig-5,6]. The A-PRF membrane is stabilised in position with mattress suture fixed mesially and distally using 4-0 non-absorbable surgical suture (Mersilk). The graft was adapted to the level of CEJ by means of sling suture and finally the lateral flaps were pulled together over the graft and sutured with simple interrupted sutures [Table/Fig-7]. Periodontal dressing was placed finally over the surgical site.
Sulcular incision given at surgical site 43.

Tunnel prepared in relation to mesial and distal papilla of 43.

A-PRF membrane is placed inside the prepared tunnel in relation to 43.
Lateral flaps sutured using simple interrupted sutures.

Postoperative Care
The patient was given proper postoperative instructions. Analgesic paracetamol 500 mg was given thrice a day to reduce post-operative pain and antibiotic amoxicillin 500 mg was also given thrice a day for 5 days. The patient was advised to use 0.2% chlorhexidine mouth rinse twice daily for 2 weeks. Patient was instructed to avoid pulling the lips and forceful brushing in the surgical area. The patient was asked to report back after 14 days for removal of periodontal dressing and suture. Review was done, healing was satisfactory, patient had no discomfort and pain. Complete root coverage was achieved with excellent tissue colour and contour. Patient recalled after 6 months and satisfactory results were obtained [Table/Fig-8].
Six months postoperative photograph of 43.

Discussion
The gingival recession is the apical displacement of gingival margin from the cemento-enamel junction. The aetiology can be multi-factorial, such as tooth malposition, thin gingival biotype, inadequate keratinised gingiva, aberrant frenum and few precipitating factors such as aggressive tooth brushing, orthodontic tooth movement, subgingival restorations and habits such as smoking are the few risk factors to gingival recession [2]. The exposure of the root surface due to gingival recession can lead to various problems such as hypersensitivity, root caries, compromised aesthetics, and impaired oral hygiene [3]. Hence the management of gingival recession, depends on proper diagnosis, evaluation of etiological factors and treatment plan. There are various therapeutic measures to treat gingival recession which include both nonsurgical and surgical management. Nonsurgical management include identifying and relieving the aetiology including the iatrogenic factors. Likewise, there are several surgical techniques for root coverage which include the pedicle graft procedures, free gingival or connective tissue graft and guided tissue regeneration using resorbable and non-resorbable membranes [3]. Over the years the conventional techniques have been modified by various clinicians for better aesthetic improvement and adequate root coverage.
In the present case report, Laterally Closed Tunnel (LCT) along with the use of A-PRF was introduced for treating the deep isolated gingival recession. An important aspect in the laterally closed tunnel is the wide mesiodistal and apical migration of the flap which enables tension free lateral movement of the flap margins that helps in root coverage [4]. The platelet concentrates such as A-PRF releases higher concentration of growth factors which improves collagen matrix synthesis and recruitment of progenitor cells helpful in regeneration.
The main goal of treating gingival recession is to achieve Complete Root Coverage (CRC) and maintain the aesthetic and stability of soft tissues over time [5]. Various studies in the past have suggested different methods to treat root coverage out of which pedicle graft was much used and gained its importance as it has got its own blood supply and potential to promote regeneration of periodontal tissues [6]. Among which Coronally Advanced Flap (CAF) combined with Subepithelial Connective Tissue Graft (SCTG) is the most commonly used and regarded as one of the predictable techniques for Miller class I or II gingival recession defects. However, their effect on wide and deep gingival recession remains inconclusive [7].
Zucchelli G et al., introduced laterally moved coronally-advanced surgical approach for treating isolated gingival recession and resulted in 96% mean root coverage. But the disadvantage with this technique is that limited amount of keratinised tissue lateral to the recession defect can result in gingival recession of donor site [8].
Sculean A and Allen EP, described a modified technique such as the laterally closed tunnel to treat the deep isolated gingival recessions [4]. The important aspect of this technique was the wide mesiodistal and apical mobilisation of the tunnel which would result in tension free movements of the lateral flap margins without disturbing the interdental papilla to cover the root surface completely which is advantageous in treating the deep isolated gingival recessions. The author used SCTG as the material for root coverage [4]. His result showed mean root coverage of 96.11% from the initial recession depth. However, limitations with the use of SCTG is that even though being a gold standard, the need for second surgical site, prolonged chair side time and donor site morbidity. Hence the concept of utilising platelet concentrate was brought into consideration. The platelet concentrate is an autologous material containing growth factors which are capable of supporting angiogenesis and tissue ingrowth. A-PRF is a third generation platelet concentrate which has the potential of sustained release of various growth factors which will aid in proper periodontal regeneration. Ghanaati S et al., detected more platelets on the distal part of clot in A-PRF with enhanced presence of neutrophilic granulocytes which could influence the differentiation of host macrophages and macrophages within the clot after implantation. Therefore, A-PRF might influence bone and soft tissue regeneration, especially through the presence of monocytes/macrophages and their growth factors [9].
The surgical procedure in the present study was performed with laterally closed tunnel technique described by Sculean A and Allen EP, [4]. We used A-PRF to cover the exposed root surfaces. Dohan DM et al., stated that three-dimensional organisation of PRF give great elasticity to the fibrin matrix in the PRF membrane and entrapment of cytokines will result in the initiation of angiogenesis [10]. Patient was reviewed after two weeks, three months and six months. At the end of 6 months, the recession coverage was amounted to be 89% and the RD and RW were reduced to 2 mm and 1 mm, respectively with KGT measuring 2 mm.
The newer technique of laterally closed tunnel was performed with A-PRF for better regeneration, reduction in the chair side time and donor site morbidity from that of using SCTG. This technique is a predictable approach for the treatment of deep isolated recessions using A-PRF. Further trials had to be done to evaluate the efficacy of this technique.
Conclusion(s)
The present study result indicates that laterally closed tunnel technique with the use of A-PRF can be an alternative for the conventional techniques for root coverage procedures. As the technique is very simple and effective with the use of A-PRF which is an autologous material that releases growth factors essential for periodontal regeneration.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 27, 2019
Manual Googling: Jan 17, 2020
iThenticate Software: Jan 28, 2020 (16%)
[1]. Steller D, Herbst N, Pries R, Juhl D, Hakim SG, Impact of incubation method on the release of growth factors in non Ca2+ activated PRP, Ca2+ activated PRP, PRF and A-PRFJ CranioMaxill Surg 2019 47(2):365-72.10.1016/j.jcms.2018.10.01730578012 [Google Scholar] [CrossRef] [PubMed]
[2]. Pradeep K, Rajababu P, Satyanarayana D, Sagar V, Gingival recession: Review and strategies in treatment of recessionCase Rep Dent 2012 2012:01-06.10.1155/2012/56342123082256 [Google Scholar] [CrossRef] [PubMed]
[3]. Kassab MM, Badawi H, Dentino AR, Treatment of gingival recessionDent Clin N Am 2010 54(1):129-40.10.1016/j.cden.2009.08.00920103476 [Google Scholar] [CrossRef] [PubMed]
[4]. Sculean A, Allen EP, The laterally closed tunnel for the treatment of deep isolated mandibular recessions: Surgical technique and a report of 24 casesInt J Periodont Rest 2018 38(4):479-87.10.11607/prd.368029889911 [Google Scholar] [CrossRef] [PubMed]
[5]. Garcia Dela Fuente AM, Aguirre Zorzano LA, Estefania Fresco R, RoigOdena L, Aguirre Urizar JM, Histologic and clinical study of gingival recession treated with subepithelial connective tissue graft: A case reportInt J Periodont Rest 2017 37(1):89-97.10.11607/prd.2638 [Google Scholar] [CrossRef]
[6]. Shah MP, Patel AP, Shah KM, Periosteal pedicle graft: A novel root coverage approachJ Indian Soc Periodontol 2015 19(1):9910.4103/0972-124X.14582825810603 [Google Scholar] [CrossRef] [PubMed]
[7]. Cairo F, Nieri M, Pagliaro U, Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions: A systematic reviewJ Clin Periodontol 2014 41(5):44-62.10.1111/jcpe.1218224641000 [Google Scholar] [CrossRef] [PubMed]
[8]. Zucchelli G, Cesari C, Amore C, Montebugnoli L, De Sanctis M, Laterally moved, coronally advanced flap: A modified surgical approach for isolated recession-type defectsJ Periodontol 2004 75:1734-41.10.1902/jop.2004.75.12.173415732880 [Google Scholar] [CrossRef] [PubMed]
[9]. Ghanaati S, Booms P, Orlowska A, Kubesch A, Lorenz J, Rutkowski J, Advanced platelet-rich fibrin: A new concept for cell-based tissue engineering by means of inflammatory cellsJ Oral Implantol 2014 40(6):679-89.10.1563/aaid-joi-D-14-0013824945603 [Google Scholar] [CrossRef] [PubMed]
[10]. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Platelet rich fibrin (PRF): A second generation platelet concentrate. Part I: technological concepts and evolutionOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101(3):3710.1016/j.tripleo.2005.07.00816504849 [Google Scholar] [CrossRef] [PubMed]