Magnetic Resonance Diagnosis of Anomalous Infraoptic Course of Anterior Cerebral Artery
Shibani Mehra1, Rushil Jain2
1 Professor, Department of Radiodiagnosis, RML Hospital ABVIMS, Delhi, India.
2 Senior Resident, Department of Radiodiagnosis, RML Hospital ABVIMS, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Shibani Mehra, C1/36, SDA, New Delhi, India.
E-mail: shibani.mehra@yahoo.in
Variations of the anterior cerebral artery and anterior communicating artery complex are common. However, an infraoptic course of A1 segment of Anterior Cerebral Artery (ACA) is a rare anatomic variation, detection of which is critical due to its association with formation of aneurysms in the anterior circulation. The diagnosis is purely radiological and MRI, Magnetic Resonance Angiography (MRA), and Computed Tomography angiography (CT angiography) have emerged as the modalities of choice because of their ability to depict the intracranial vessels accurately. Both CT and MR angiography are preferred over catheter angiography because of their non-invasive nature. Time of flight MR angiography is an MR angiography technique which demonstrates intracranial vessels without administering gadolinium based MR contrast medium and is therefore safe for all age groups and all patient categories. Here, authors present the MR findings that lead to the radiological diagnosis of anomalous infraoptic anterior cerebral artery in a patient presenting with an episode of transient ischaemic attack.
Anomalous vessel course, Magnetic resonance angiography, Time of flight angiography, Transient ischaemic attack
Case Report
A 50-year-old woman presented to Emergency Department with single episode of Transient Ischaemic Attack (TIA). The patient was conscious and well-oriented. The neurological examination was normal with normal tone power and sensation in upper and lower limbs. There was no history of diabetes or hypertension although a family history of hypertension and ischaemic heart disease was elicited. The blood glucose level, serum electrolytes, lipid profile and coagulation profile were normal. The Electrocardiography (ECG) and Echocardiography examination were normal. The carotid Doppler examination did not reveal any plaque.
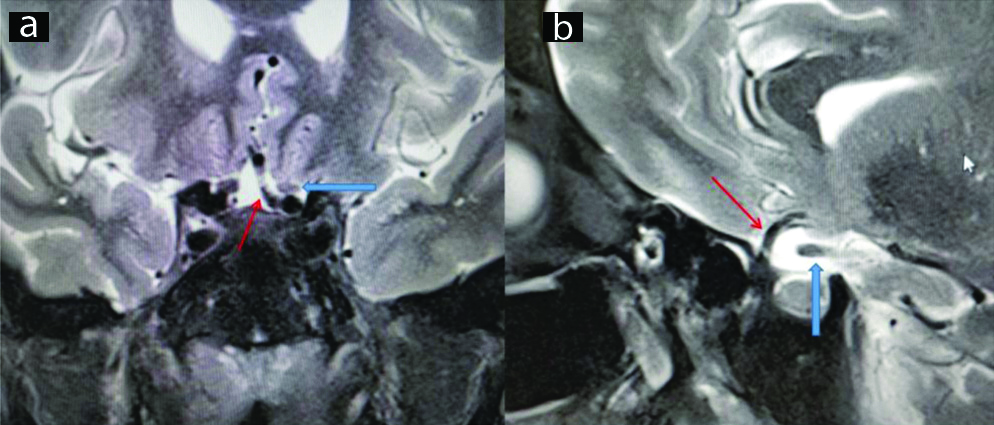
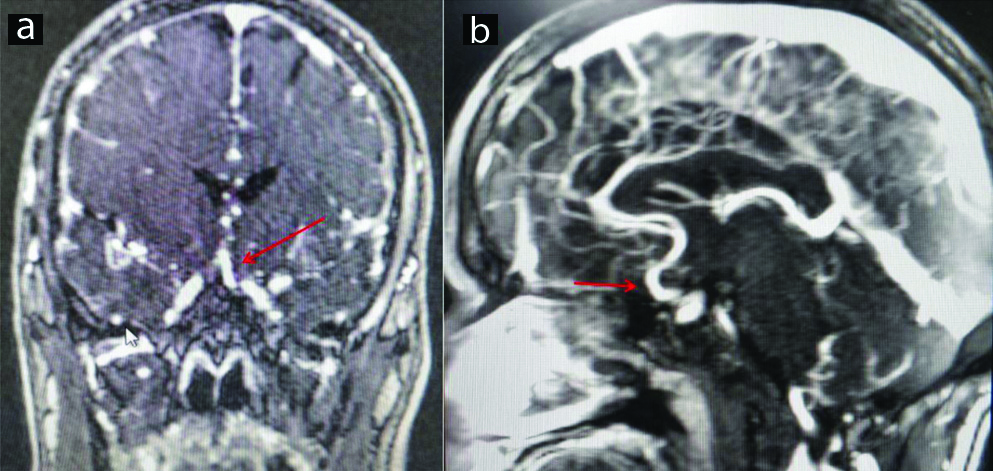
The patient was referred to the Department of Radiology for MRI Brain to rule out cerebral infarct. Axial T2 MR Images revealed normal signal intensity of brain parenchyma with no infarct. However, the left ACA was seen arising from the supraclinoid Internal Carotid Artery (ICA) and had an abnormal course below the optic nerve and chiasm [Table/Fig-1a,b]. Time of Flight (ToF) MR Angiography sequence confirmed that the A1 segment of left ACA originated from ipsilateral Internal carotid artery, inferior to the optic nerve and was then coursing superiorly with normal communication with the anterior communicating artery [Table/Fig-2a,b]. The vessels of the anterior circulation were otherwise normal in calibre with no evidence of aneurysmal dilatation.
a) Low bifurcation of the left ICA is seen with left ACA arising from intradural ICA near origin of ophthalmic artery. A1 segment of ACA (Red thin arrow) passes medially below the ipsilateral optic nerve (Double blue arrow); b) The A1 segment of ACA (Red thin arrow) turns superiorly anterior to optic chiasm (Double blue arrow).
a) The A1 segment of left ACA (Red thin arrow) is seen to originate from ICA inferior to optic nerve and course superiorly; b) The A1 segment of left ACA (Red thin arrow) is seen to join the normally positioned anterior communicating artery.
The patient was discharged after advising regular follow-up neurology OPD visits at 3 months intervals. The patient has been visiting the OPD regularly for the past 10 months and has not developed any further episode of transient ischaemic attack. The finding of anomalous vessel course was incidental; the anomalous anterior cerebral artery was not seen stenosed or attenuated in calibre at any point. The TIA was therefore not related to stenosis, yet, since aneurysms have been commonly reported at the point where anomalous coursing anterior cerebral artery joins the anterior communicating artery, it can be assumed that transient compression can similarly occur at this very site. This was the intention of keeping the patient on follow-up with neurologist.
Discussion
The anterior circulation to the brain parenchyma is through the ICA which divides into the ACA, the Middle Cerebral Artery (MCA) and the anterior choroidal artery, each vessel supplying distinct anatomic territories of the brain. ACA vascular supply is to the anterior three fourth of the medial surface of the cerebral cortex, the frontal pole with anterior portion of the corpus callosum, the anterior limb of internal capsule, inferior portion of the head of caudate nucleus and to anterior globus pallidus. The normal ACA commences at the medial aspect of Sylvain fissure as one of the terminal branches of the ICA and passes anterior and medial to the optic nerve in close relation to the ACA of the opposite side. The vessel has a rostral course into the longitudinal fissure between the cerebral hemispheres in the midsagittal plane. The ACA is anatomically classified and divided into A1 (pre-communicating), A2 (post-communicating), A3 (pre-callosal), A4 (supracallosal) and A5 (post-callosal) segments. The orbital and frontopolar branches are the last branches to arise from the rostral and ventral portion of the ACA before it terminates as the callosal marginal and pericallosal arteries that sweep caudally along the medial surface of cerebral hemisphere [1]. The anterior communicating artery (A com) is a small branch of the ACA which connects it to the contralateral artery.
The Anterior cerebral artery-anterior communicating artery (ACA-A Com) complex comprising bilateral A1 segments and the anterior communicating artery is normally situated just above the optic apparatus. Variations of the ACA-A Com complex can be present. However, an infraoptic course of A1 segment of ACA is a rare anatomic variation of intracranial vasculature with only 54 cases reported so far [2]. This aberrant course of ACA results from a low bifurcation of the ICA, where from the proximal segment of the anterior cerebral artery heads horizontally and medially, passing under the ipsilateral optic nerve before turning upwards. The origin of the ACA becomes therefore intradural. The anterior communicating artery is not affected and seen normally positioned [3]. One or both anterior cerebral arteries may demonstrate an infraoptic course [4]. When unilateral, the anomalous coursing ACA is usually right sided. The embryological basis of this condition is persistence of the anatomic loop between the primitive dorsal and ventral ophthalmic arteries which is normally found in utero. This is also the reason for using the term carotid-anterior cerebral artery anastomosis to describe the infraoptic coursing ACA [5]. The components of this anastomosis are ACA originating at or near the origin of ophthalmic artery from the ICA, and therefore lying intradural, and then seen coursing ventral to the optic nerve, anterior to the optic chiasm. The infraoptic coursing segment is the proximal A1 segment of the ACA. However in some patients, a normally positioned smaller A1 segment may coexist, thus an accessory A1 segment may be an accompaniment of the infraoptic ACA.
The advantage of MR in neuroimaging cannot be understated and routine MR imaging has the ability to identify any anomaly in position or course of intracranial and anterior circulation vessels [6]. Traditionally, catheter angiography was used for diagnosis of aberrant intracranial vessels. However, with the advent of high resolution CT and MR angiography, pre-operative detection of anomalous intracranial vessel course has become possible noninvasively. MR angiography can be performed without any intravenous contrast administration using the phase contrast or time of flight techniques. Time of flight MR Angiography demonstrates in-flowing blood in the imaged volume as high signal intensity and bright compared with signal from stationary tissue of the brain parenchyma which has been magnetically saturated by application of multiple repetitive Radio Frequency (RF) pulses that reduce the magnetisation level of stationary tissues. The Maximum Intensity Projection (MIP) images obtained after processing TOF MR Angiogram, demonstrate the vessels as bright due to this principle of flow related enhancement, the fresh flowing blood in the imaged volume having been exempted from the saturation effect of RF pulses. The diagnostic feature for infraoptic course of ACA on catheter angiography, CT or MR angiography is identification of low bifurcation of Internal carotid artery, such that the anterior cerebral artery is visualised at the level of the optic nerve. TOF, phase contrast or gadolinium enhanced MR angiography, have similar diagnostic accuracy as catheter angiography for depicting the infraoptic course of ACA. MRA is therefore preferred as the modality of choice for depiction of intracranial vascular anatomy [7]. MR angiography further scores over catheter angiography in providing important information about the relationship of the ACA to the optic tract and optic chiasm. This is important because in its infraoptic course, the ACA can ascend either anterior to the chiasm between the optic nerves; or can even pierce the ipsilateral optic chiasm and visual field defects can result from this vicinity of neural and arterial structures.
Variant ACA anatomy is known to be an exceedingly frequent cause of A Com aneurysms and thus a known complication associated with infraoptic course of ACA is the high incidence of occurrence of berry aneurysms. These aneurysms can rupture and lead to subarachnoid haemorrhage which may be the first clue to presence of this aberration [8]. Aneurysm formation can be attributed to the tortuosity of the proximal A1 segment. It is also interesting to note that aneurysms can develop in other vessels of anterior circulation, namely the MCA and not be confined to the ACA alone. Pre-operative demonstration of aberrant vessel course allows optimal surgical planning and pre-empts intra-operative problems. Another complication of infraoptic ACA is development of cerebral arterio-venous malformations. The spectrum of vascular aberrations associated with an infraoptic coursing, ACA can be myriad and include a hypoplastic A1 segment, a fenestrated A Com segment, an accessory A Com, accessory A2 segment, an azygos ACA vessel or bi-hemispheric infraoptic ACA [2]. MR has the ability to demonstrate these coexisting vascular anomalies in a patient with infraoptic ACA with ease and accuracy. Infraoptic ACA may also coexist with a carotid-basilar artery anastomosis, agenesis of contralateral ICA and development of Moyamoya disease or coarctation of aorta [9]. The origin of MCA may be seen from the basilar artery instead of the ICA.
A complication of greater interest to the surgeon in this setting of anomalous coursing ACA is common origin of the ophthalmic artery with the infraoptic A1 segment of the aberrant ACA. This common origin of ophthalmic artery and ACA results from failure of caudal migration of primitive ventral ophthalmic artery as well as failure of regression of primitive dorsal ophthalmic artery [5]. The radiologist must be able to identify and report this finding on MR angiography. When dealing with aneurysm repair, knowledge of the aberrant course of ACA is crucial for the surgeon, since a modification of the surgical approach will be needed in order to gain proximal control of the aneurysm. Moreover, because the optic nerve and chiasm are located immediately above and anterior to aberrant coursing ACA, failure to identify the infraoptic course of ACA pre-operatively leads to a definite chance of damaging the optic apparatus during aneurysm repair surgery [10]. The anomalous course of ACA is also important when operating sellar or pituitary tumours to prevent rupture of the ACA or damaging optic nerve during surgery.
The present case reported highlights the value of MR imaging in identifying this variant anatomy. Although the clinical significance of this variant ACA anomaly is minor, it is the association of the vascular course with intracranial aneurysms or subarachnoid haemorrhage that has been reported time and again in literature [8,11]. The aneurysms associated with anomalous coursing ACA may be the cause of headache and altered consciousness due to subarachnoid haemorrhage. The index patient had presented with TIA and although such an association has not been described so far, we believe that the tortuous course of the vessel and its transition from horizontal position to vertical as it proceeds to join the Anterior communicating segment makes it prone to compression which can trigger a transient ischaemic episode. More research into this aspect is however warranted. We assume that transient compression of the anomalous coursing vessel could have been the reason for triggering the TIA. Therefore after the diagnosis, the patient has been placed on regular follow-up by the neurologist. Thus, MRI with Time of flight non-contrast angiography can provide important information about the cerebral vasculature and TOF MR angiography must be incorporated in all patients suspected to have neurovascular association of presenting symptoms.
Conclusion(s)
MR enables identification of variant vascular anatomy non-invasively. Both catheter angiography and MR angiography have equally high efficacy for detecting an unusual variant course of ACA and associated complications. Pre-operative detection of variations in intracranial vessel course is critical and essential to guide the neurosurgeon dealing with an aneurysm in order to avoid any catastrophe resulting from ignorance about the aberrant course of anterior circulation vessels.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 16, 2019
Manual Googling: Nov 21, 2019
iThenticate Software: Jan 30, 2020 (9%)
[1]. Collins P, Embryology and development. In: Williams PL, Bannister LH, Berry MM, Collins P, Dyson M, Dussek JE, Ferguson MWJ (eds)Gray’s Anatomy 1995 38rd ednChurchill Livingstone, Edinburgh:314 [Google Scholar]
[2]. Nandish HS, Selvapandian S, Ghosh S, Surgical significance of infraoptic course of A1 segment of anterior cerebral artery: Report of two casesAsian J Neurosurg 2019 14(3):927-29.10.4103/ajns.AJNS_34_1931497131 [Google Scholar] [CrossRef] [PubMed]
[3]. Fujimoto S, Murakami M, Anomalous branch of the internal carotid artery supplying circulation of the anterior cerebral artery: Case reportJ Neurosurg 1983 58:941-46.10.3171/jns.1983.58.6.09416854389 [Google Scholar] [CrossRef] [PubMed]
[4]. Ji C, Ahn JG, Infraoptic course of both anterior cerebral arteriesJ Korean Nerosurg Soc 2010 47(1):71-73.10.3340/jkns.2010.47.1.7120157384 [Google Scholar] [CrossRef] [PubMed]
[5]. Nutik S, Dilenge D, Carotid-anterior cerebral artery anastomosis: Case reportJ Neurosurg 1976 44(5):378-82.10.3171/jns.1976.44.3.03781249618 [Google Scholar] [CrossRef] [PubMed]
[6]. Uchino A, Nomiyama K, Takase Y, Kudo S, Anterior cerebral artery variations detected by MR angiographyNeuroradiology 2006 48(9):647-52.10.1007/s00234-006-0110-316786350 [Google Scholar] [CrossRef] [PubMed]
[7]. Curtis A, Given II, P. Pearse Morris. Recognition and importance of an infraoptic anterior cerebral artery: Case reportAm J Neuroradiol 2002 23:452-54. [Google Scholar]
[8]. Rao SA, Sai Kiran NA, Abdul AZ, Hegde AS, Infraoptic course of the anterior cerebral artery associated with anterior communicating artery and distal anterior cerebral artery aneurysmsNeurology 2015 63(5):797-99.10.4103/0028-3886.16656326448252 [Google Scholar] [CrossRef] [PubMed]
[9]. Ji C, Ahn JG, Cho SM, Infraoptic Course of both anterior cerebral arteries associated with a middle cerebral artery aneurysm and an aortic coarctationJ Korean Soc Radiol 2009 60:377-81.10.3348/jksr.2009.60.6.377 [Google Scholar] [CrossRef]
[10]. Kim MS, Yoon SW, Lee GH, Lee CH, Infraoptic course of the anterior cerebral artery-Case reportKorean J Cerebrovasc Surg 2011 13(1):15-18. [Google Scholar]
[11]. Gupta V, Chugh M, Vaishya S, Infraoptic azygos anterior cerebral artery Neurology 2008 56(4):487-88.10.4103/0028-3886.4481919127053 [Google Scholar] [CrossRef] [PubMed]