Rare Cutaneous Ischaemia and Pain during Infiltrative Anaesthesia for Dental Surgery: Case Reports and Literature Review
Hacer Ulutürk1, Goktug Eberlikose2, Gönen Özcan3, Dervis Yilmaz4
1 Resident, Department of Oral and Maxillofacial Surgery, Gazi University Faculty of Dentistry, Ankara, Turkey.
2 Resident, Department of Periodontology, Gazi University Faculty of Dentistry, Ankara, Turkey.
3 Professor, Department of Periodontology, Gazi University Faculty of Dentistry, Ankara, Turkey.
4 Professor, Department of Oral and Maxillofacial Surgery, Gazi University Faculty of Dentistry, Ankara, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Hacer Ulutürk, Gazi University Faculty of Dentistry, Ankara, Turkey.
E-mail: hcrulutuerk@gmail.com
Local Anaesthetics (LA) is commonly used for surgical and dental procedures. Complications related to local anaesthesia can be divided into local, systemic and immediate complications. Immediate complications include positive blood aspiration, blanching of the tissue, pain, facial paralysis and burning sensation on impingement of the nerve. Blanching develops from decreased blood flow to the tissues as a result of blood vessels narrowed by adrenaline. The precise cause of this complication is unknown; however, it may be derived because of intraarticular injection, anatomical variation, rapid injection of local anaesthetic solution, retrograde flow of the solution, misdirection of the needle and neuronal basis. This report of 2 cases describes patients with ischemic areas on their faces resulting from maxillary and mandibular buccal infiltrative anaesthesia techniques. After the skin ischaemia associated with the severe and instant pain occurs, the patient should be calmed and informed about the reversibility of the situation. It also includes information about the diagnosis, management, literature review and proposes some mechanisms for cutaneous ischaemia and pain.
Immediate complication, Local anaesthetics, Skin blanching
Case 1
A 33-year-old male patient was referred to the Department of Oral and Maxillofacial Surgery, for the treatment of dental implant in the lower left molar area. He had no history of complications during the implant surgery. His medical history was non-contributory.
A left mandibular buccal infiltrative anaesthesia was achieved using 0.1 mL of 4% articaine hydrochloride with epinephrine 1:100,000 (Ultracaine D-S Forte; Aventis, Istanbul, Turkey) with a 27 gauge needle. Negative aspiration was performed. At the time of injection the patient felt itching, a sudden pain and burning at the injection area. Within one minute the ipsilateral side of the nose, cheek, and infraorbital area and above the nasolabial line turned pale [Table/Fig-1a]. The blanching extended to the left side of the nose and the lip [Table/Fig-1b]. Intraorally, the lower left lip had clinical signs of numbness. The patient was informed about the complication. The anaesthesia of the operative area was successful. Two dental implants were inserted in the lower molar region. It was observed that, numbness and paleness completely resolved after 40 minutes of the injection. The reason of the complication may be related to fast injection of the anaesthetic solution or due to the anatomical variations. Patient was informed about the possibility of the complication in future applications.
a) First case: Blanching of the nose (alea area), cheek, with a less extent to the infraorbital area and above the nasolabial line; b) First case: Blanching extended to the left side of the nose and the lip.

Case 2
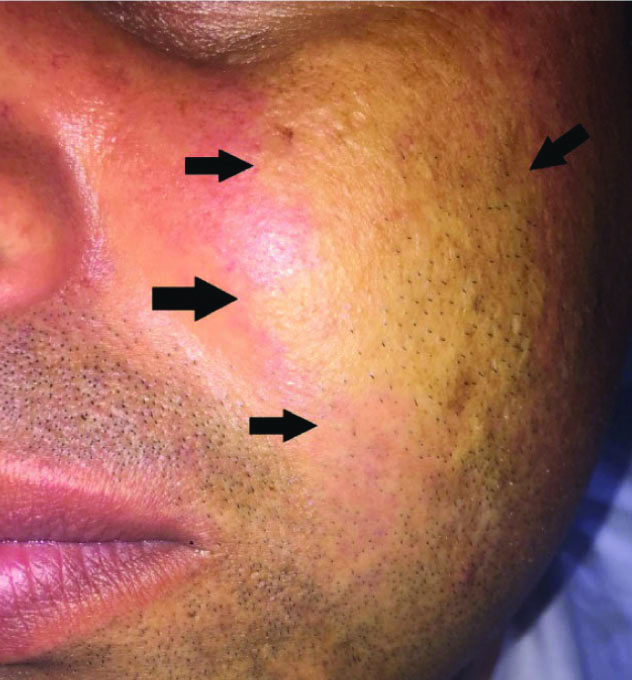
A 49-year-old male patient, American Society of Anesthesiologists (ASA) I, was referred for the extraction of his upper left second and third molar. A standard buccal infiltrative anaesthesia was conducted using 0.1 mL of 4% articaine hydrochloride with epinephrine 1:100,000 (Ultracain D-S Forte; Aventis, Istanbul, Turkey) with a 27 gauge needle in the maxillary posterior area. Negative aspiration was performed. The patient felt a sudden pain centered around the infraorbital area while injecting the solution and started being anxious. Immediately after injection ipsilateral blanching of the cheek was observed [Table/Fig-2]. Thereafter, the patient was informed about the complication. The anaesthesia of the extraction area was achieved, and the extraction of the teeth was performed. The blanching of the skin returned to completely normal appearance 30 minutes after injection.
Second case: Blanching of the cheek.
Discussion
To the best of our knowledge, this is the first case report to present reaction associated with mandibular infiltrative anaesthesia that included temporary ischaemia in the branches of the facial artery. Ophthalmic, ear and cutaneous complications during Inferior Alveolar Nerve Block (IANB) are well described in literature. The PubMed (MEDLINE) database and Google scholar was used for a literature search of articles about skin blanching published until 2019. The following search terms were used in different combinations via the conjunctions ‘and’ and ‘or’ Skin blanching, facial blanching, cutaneous blanching, paleness, dental complication, local anaesthesia and inferior alveolar nerve block. Case series and reports which contains cutaneous paleness due to local anaesthesia were selected. Fifteen publications finally met the inclusion criteria in which 10 cases were found in Google Scholar and 5 cases in PubMed. In these 16 case reports which includes our report also, 25 patients were reported [Table/Fig-3] [1-15]. Of these 25 patients, 16 underwent routine inferior alveolar block anaesthesia [Table/Fig-3]. Positive aspiration has been described in only one case [1]. This kind of complication is very rare but when it occurs it may have a considerable unfavorable psychologic effect for patient and cause inconvenience for the dentist [11].
Literature Review: Affected pale areas in association with gender, needle gauge, anaesthesia technique and solution [1-15].
| Author | Gender/age | Medical history | Needle type | Anaesthesia technique | Anaesthetic solution | Affected area (pallor) |
|---|
| Arevana PC et al., [1] | Female/21 | None | 27 G. | Troncular IAN Block | 1.8 mL 4% articaine HCl, epinephrine 1:100,000 | -Vestibule of the left upper lip and cheek |
| Blaxter PL and Britten M, [2] | Female/16 | None | No Information | Inferior Alveolar Block | Procaine, 1:300,000 adrenaline | -Lateral to the eye, above the eyebrow |
| Ezirganli S and Kazancioglu HO, [3] | Female/29 | None | 27 G. | Inferior Alveolar Block | Articaine HCl (40 mg/mL), epinephrine (adrenaline, 0.012 mg/mL). | -Lateral nasal wall, inferior orbital ridge, cheek |
| Female/32 | None | 27 G. | Inferior Alveolar Block | 4% articaine hydrochlorid, 1:100.000 epinephrine | -Lateral nasal wall, inferior orbital ridge, cheek, half of the superior lip |
| Goldenberg AS, [4] | Male/58 | None | 27 G. | Inferior Alveolar Block | 1,8 ml Lidocaine HCl, 1:100,000 epinephrine | -Forehead, upper eyelid |
| Huang RY et al., [5] | Female/32 | None | 27 G. | Inferior Alveolar Block | 2% lidocaine HCl, 1:80,000 epinephrine | -Left cheek, infraorbital, nasal heel, alae area-Right half was flushing |
| Kang SH and Won YJ, [6] | Female/25 | None | No Information | Inferior Alveolar Block | 1.8 ml lidocaine HCl, 1:80,000 epinephrine | -Nose, upper lip, central facial region, and the left zygomatic area |
| Kronman JH and Giunta J, [7] | Male/19 | None | No Information | Inferior Alveolar Block | 2% lidocaine HCl, 1:100,000 epinephrine | -Lower eyelid, malar area, the midlateral portion of the nose |
| Male/21 | None | No Information | Inferior Alveolar Block | 2% lidocaine HCl, 1:100,000 epinephrine | -Whole lower eyelid, infraorbital area down to the malar area |
| Male/23 | None | No Information | Maxillary buccal infiltrative | 2% lidocaine HCl, 1:100,000 epinephrine | -Below the right eyelid extending to the infraorbital area, midlateral side of the nose, across the cheek above the nasolabial line |
| Kumaresan R et al., [8] | Female /57 | Diabetus mellitus | 27 G | Inferior Alveolar Block | 2% Lidocaine HCl, 1:80,000 adrenaline | -left infraorbital area, the point of needle insertion, the left hard and soft palate alveolar ridge |
| McCormick RS and Adams JR, [9] | Male/45 | SCC History | Self aspirating syringe | Hard and soft palate infiltrative | 2% lignocaine, 1:80000 adrenaline | -Right side of the face in the distribution of the infraorbital artery |
| Paul R et al., [10] | Male/44 | None | 27 G. | Inferior Alveolar Block | 2% Lidocaine HCl, 1:80,000 adrenaline | -Right infra-orbital, hard and soft palate |
| Scarano A et al., [11] | Male/mean age 56 | None | 27 G. | Maxillary Buccal Infiltrative | 2% lidocaine HCl, 1:100,000 adrenaline | -Cheek near the root of the nose, lower eyelid |
| Male/mean age 56 | None | 27 G. | Maxillary Buccal Infiltrative | 2% lidocaine HCl, 1:100,000 adrenaline | -Cheek near the root of the nose, lower eyelid |
| Male/ mean age 56 | None | 27 G. | Maxillary Buccal Infiltrative | 2% lidocaine HCl, 1:100,000 adrenaline | -Cheek near the root of the nose, lower eyelid |
| Male/ mean age 56 | None | 27 G. | Maxillary Buccal Infiltrative | 2% lidocaine HCl, 1:100,000 adrenaline | -Cheek near the root of the nose, lower eyelid |
| Male/ mean age 56 | None | 27 G. | Maxillary Buccal Infiltrative | 2% lidocaine HCl, 1:100,000 adrenaline | -Cheek near the root of the nose, lower eyelid |
| Torrenta-Castells E et al., [12] | Female/10 | None | 27 G. | Inferior Alveolar Block | 2% Articaine, 1:200,000 epinephrine | -Right side of the lower lip and chin |
| Uckan S et al., [13] | Male/25 | None | 27 G. | Inferior Alveolar Block | 4% articaine HCl, 1:100.000 epinephrine | -Cheek, middle of the forehead |
| Female/30 | None | 27 G. | Inferior Alveolar Block | 4% articaine HCl, 1:100.000 epinephrine | Cheek |
| Webber B et al., [14] | Female/33 | None | No Information | Inferior Alveolar Block | 2% Lidocaine HCl, 1:100,000 epinephrine | -Left infraorbital region, left side of the nose, lower eyelid and the lip |
| Williams JV et al., [15] | Male/25 | None | 28 G. | Inferior Alveolar Block | 2.2 mL 2% lignocaine, 1:80,000 epinephrine | -Periorbital |
| Ulutürk H et al.,(present study) | Male/33 | None | 27G | Mandibular buccal infiltrative | 0.1 mL of 4% articaine hydrochloride with epinephrine 1:100,000 | ipsilateral side of the nose, cheek, infraorbital area and above the nasolabial line |
| Male/49 | None | 27G | Maxillary buccal infiltrative | 0.1 mL of 4% articaine hydrochloride with epinephrine 1:100,000 | ipsilateral blanching of the cheek |
In the first case, the blanching of the skin area may be related with the branches of the facial artery from the external carotid artery which winds its way obliquely up beneath the digastric and stylohyoid muscles and passes the submandibular gland [16]. It curves over the body of the mandible at the antero-inferior angle of the masseter; passes onto the face. It courses over the face, gives terminal branches the inferior and superior labial branch and lateral nasal branch and masseteric branches [16]. To date, mechanisms leading to cutaneous complications are not clear enough. However, researchers focus their attention on certain hypotheses.
In the second case the blanching of the skin area may correlated with the branches of the infraorbital artery which is the terminal division of the maxillary artery. The maxillary artery continues as the largest terminal branch of the external carotid artery in the head region [17]. Topographically, based on its relationship to the external pterygoid muscle the main trunk can be divided into three parts: mandibular, pterygoid and pterygopalatine. The pterygopalatine segment of the maxillary artery provides four distal branches that accompany similarly named branches of the maxillary nerve. The Infraorbital Artery (IOA) is one of the distal branches and passes forwards along the roof of the maxillary antrum to emerge with the infraorbital nerve on the face [17]. IAO enters into the face through the Infraorbital foramen and it supplies to cheek, lateral nose and lower eyelid. It anastomose with branches of the opthalmic, buccal, transverse facial arteries [11].
Intra-Arterial Injection
Epinephrine in the anaesthetic solution causes vasoconstriction along the branches of the vessels close to the injection site or the anaesthetic solution is injected into a vessel and carried to the periphery [18]. In patients with an injection of local anaesthesia into an artery, the vasoconstrictor, epinephrine rapidly produces a vasoconstriction and pain [11]. Aravena PC et al., described that intravascular injection on an IAN block is reported in a frequency of 31.3% after the first positive aspiration [1]. It has been suggested that the intravascular injection should be checked for aspiration at least twice during the procedure of anaesthesia by using adequate needle size (>25-gauge) [5]. The negative aspiration may well have been a ‘false-negative’ finding, even though the subsequent movement of either the needle or the patient may cause the injection within the vascular lumen [5]. Freuen ND et al., postulated that solutions that are injected quickly and under pressure may carry some anaesthetic solution in a retrograde direction [19]. However, this may be possible if one considers that the solution is injected under pressure, with a reduction in the injection/arterial pressure gradient during diastole [19]. This hypothesis is supported by data obtained from contrast radiography and hemodynamic and electroencephalographic studies on carotid blood flow in rhesus monkeys [20]. Reverse carotid flow can be induced by injections administered faster than 1 cartridge in 30 seconds [20,21].
In case 2, reverse flow of the solution was probably caused by the quick injection of the agent. Reflective vasospasm of the IOA can be induced by the anaesthetic solution [11]. Webber B et al., discussed that epinephrine is a vasopressor agent which works by stimulating both alfa and beta-adrenergic receptors. Epinephrine increases blood pressure by stimulating the cardiac beta 1 receptors of the myocardium, which increases its ventricular contraction strength and the heart rate, as well as by peripheral blood vessels vasoconstriction [14]. This may explain the blanching of the skin from blood flow decreasing.
Neural Theory
The reason of the blanching can be explained by a neuronal basis with the exception of the intravascular injection of local anaesthesia. The vasomotor vasoconstrictor fibers from the superior cervical sympathetic chain reach the cutaneous vessels of the face and are known to control the caliber of these vessels [22]. Postganglionic fibers extend to the external carotid plexus and to the lingual and facial plexus, among others, where they follow the arteries and smooth muscle of walls of blood vessels. The tip of the needle can injure the sympathetic fibers of the tunica adventitia of the artery resulting a vasospasm [1]. The sympathetic impulse may cause an itching pain that can occasionally be experienced by patient during the injection. Boynes SG et al., reported that skin blanching appears more often during mandibular anaesthesia compared with the maxillar anaesthesia (28.6% vs. 2.8%) [23].
According to the current case reports, skin ischaemia in patients can be explained through some of the mechanisms considered above. The vasomotor supply of cental face is mainly under vasodilator control, hence the effect of vasoconstriction is of short term and then the vessels dilate which causes the colour of skin to normal [22].
The most important measures that can be taken in order to avoid such complications in dental anaesthesia are aspiration control before injecting anaesthetic solution and injecting anaesthetic agent at a slow rate after negative aspiration. After the skin ischaemia associated with the severe and instant pain, the patient should be calmed and informed about the reversibility of the situation.
Conclusion(s)
Including the very recent ones, some textbooks do not even mention cutaneous complications but during the usage of local anaesthesia with adrenaline, the possibility of cutaneous ischaemia should be considered. The clinician must explain the patient when these kinds of anaesthesia complications occurs and comfort the patient that situation will be completely resolved and should not misinterpret the complication.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 05, 2019
Manual Googling: Nov 23, 2019
iThenticate Software: Jan 27, 2020 (18%)
[1]. Aravena PC, Valeria C, Nuñez N, Perez-Rojas F, Coronado C, Skin and mucosal ischemia as a complication after inferior alveolar nerve blockDental Research Journal 2016 13(6):56010.4103/1735-3327.19704028182074 [Google Scholar] [CrossRef] [PubMed]
[2]. Blaxter P, Britten M, Transient amaurosis after mandibular nerve blockBritish Medical Journal 1967 1(5541):68110.1136/bmj.1.5541.6816019671 [Google Scholar] [CrossRef] [PubMed]
[3]. Ezirganli S, Kazancioglu HO, An unforeseen complication arising from inferior alveolar nerve block: is anemia possible?Journal of Craniofacial Surgery 2013 24(6):2178-79.10.1097/SCS.0b013e3182a2de1a24220435 [Google Scholar] [CrossRef] [PubMed]
[4]. Goldenberg AS, Diplopia resulting from a mandibular injectionJournal of Endodontics 1983 9(6):261-62.10.1016/S0099-2399(86)80026-7 [Google Scholar] [CrossRef]
[5]. Huang RY, Chen YJ, Fang WH, Mau LP, Shieh YS, Concomitant horner and harlequin syndromes after inferior alveolar nerve block anaesthesiaJournal of Endodontics 2013 39(12):1654-57.10.1016/j.joen.2013.09.00624238467 [Google Scholar] [CrossRef] [PubMed]
[6]. Kang SH, Won YJ, Facial blanching after inferior alveolar nerve block anaesthesia: An unusual complicationJournal of Dental Anaesthesia and Pain Medicine 2017 17(4):317-21.10.17245/jdapm.2017.17.4.31729349355 [Google Scholar] [CrossRef] [PubMed]
[7]. Kronman J, Giunta J, Reflex vasoconstriction following dental injectionsOral Surgery, Oral Medicine, Oral Pathology 1987 63(5):542-44.10.1016/0030-4220(87)90224-6 [Google Scholar] [CrossRef]
[8]. Kumaresan R, Rajeev V, Karthikeyan P, Arunachalam R, An unusual complication after administrating an inferior alveolar nerve block-A case reportJournal of oral and maxillofacial surgery, medicine, and pathology 2018 30(2):151-53.10.1016/j.ajoms.2017.10.006 [Google Scholar] [CrossRef]
[9]. McCormick RS, Adams JR, Blanching of facial skin after infiltration of local anaesthetic: an unusual complication of inadvertent intra-arterial injectionThe British Journal of Oral & Maxillofacial Surgery 2016 54(9):105110.1016/j.bjoms.2016.02.01026922404 [Google Scholar] [CrossRef] [PubMed]
[10]. Paul R, Anand R, Wray P, D’sa S, Brennan P, An unusual complication of an inferior dental nerve block: A case reportBritish Dental Journal 2009 206(1):910.1038/sj.bdj.2008.112019132028 [Google Scholar] [CrossRef] [PubMed]
[11]. Scarano A, Sinjari B, Lorusso F, Mortellaro C, D’Ovidio C, Carinci F, Intense, Instantaneous, and Shooting Pain during Local Anaesthesia for Implant SurgeryJournal of Craniofacial Surgery 2018 29(8):2287-90.10.1097/SCS.000000000000457529621089 [Google Scholar] [CrossRef] [PubMed]
[12]. Torrente-Castells E, Gargallo-Albiol J, Rodríguez-Baeza A, Berini-Aytés L, Gay-Escoda C, Necrosis of the skin of the chin: a possible complication of inferior alveolar nerve block injectionThe Journal of the American Dental Association 2008 139(12):1625-30.10.14219/jada.archive.2008.010419047668 [Google Scholar] [CrossRef] [PubMed]
[13]. Uckan S, Cilasun U, Erkman O, Rare ocular and cutaneous complication of inferior alveolar nerve blockJournal of Oral and Maxillofacial Surgery 2006 64(4):719-21.10.1016/j.joms.2005.12.01816546657 [Google Scholar] [CrossRef] [PubMed]
[14]. Webber B, Orlansky H, Lipton C, Stevens M, Complications of an intra-arterial injection from an inferior alveolar nerve blockThe Journal of the American Dental Association 2001 132(12):1702-04.10.14219/jada.archive.2001.012311780989 [Google Scholar] [CrossRef] [PubMed]
[15]. Williams J, Williams L, Colbert S, Revington P, Amaurosis, ophthalmoplegia, ptosis, mydriasis and periorbital blanching following inferior alveolar nerve anaesthesiaOral and Maxillofacial Surgery 2011 15(1):67-70.10.1007/s10006-010-0238-520577772 [Google Scholar] [CrossRef] [PubMed]
[16]. Barral JP, Croibier A, Visceral Vascular Manipulations E-Book 2011 Elsevier Health Sciences10.1016/B978-0-7020-4351-2.00007-7 [Google Scholar] [CrossRef]
[17]. Allen III WF, Kier EL, Rothman SL, The maxillary artery: normal arteriographic anatomyAmerican Journal of Roentgenology 1973 118(3):517-27.10.2214/ajr.118.3.5174723177 [Google Scholar] [CrossRef] [PubMed]
[18]. Lustig JP, Zusman SP, Immediate complications of local anaesthetic administered to 1,007 consecutive patientsThe Journal of the American Dental Association 1999 130(4):496-99.10.14219/jada.archive.1999.024310203899 [Google Scholar] [CrossRef] [PubMed]
[19]. Freuen ND, Feil BA, Norton NS, The clinical anatomy of complications observed in a posterior superior alveolar nerve blockFederation of American Societies for Experimental Biology 2007 [Google Scholar]
[20]. Aldrete JA, Narang R, Sada T, Liem ST, Miller GP, Reverse carotid blood flow-A possible explanation for some reactions to local anaestheticsThe Journal of the American Dental Association 1977 94(6):1142-45.10.14219/jada.archive.1977.0365405406 [Google Scholar] [CrossRef] [PubMed]
[21]. Malamed S, The possible secondary effects in cases of local anaesthesiaRevue belge de Medecine Dentaire 2000 55(1):19-28. [Google Scholar]
[22]. Gonzalez G, Onofrio BM, Kerr FW, Vasodilator system for the faceJournal of Neurosurgery 1975 42(6):696-703.10.3171/jns.1975.42.6.06961095694 [Google Scholar] [CrossRef] [PubMed]
[23]. Boynes SG, Echeverria Z, Abdulwahab M, Ocular complications associated with local anaesthesia administration in dentistryDental Clinics 2010 54(4):677-86.10.1016/j.cden.2010.06.00820831931 [Google Scholar] [CrossRef] [PubMed]