Mandibular canal is between mandibular foramen and mental foramen and it includes inferior alveolar neurovascular bundle [1]. Bifid or trifid mandibular canal, which is described in literature in 1970s, is an anatomic variation of mandibular canal [1,2]. Bifid and trifid mandibular canals can be assessed by using panoramic radiograph, Computed Tomography (CT) and CBCT [3]. Rouas P et al., stated that panoramic radiograph was insufficient in the detection of bifid mandibular canal, CBCT which gives out less radiation when compared with CT has been reported to be perfect in assessing such anatomic variations [4]. A large number of studies have been conducted about bifid mandibular canal prevalence by using CBCT [1,5-7].
Mandibular canal and its variations should be known by dentists before a large number of dental and surgical processes [8]. Complications such as haemorrhage and paraesthesia can be prevented through correct assessment and planning before surgical processes [9].
Third molar extraction in mandibular molar area and implant applications in mandibular posterior edentulous cases are very common and bifid mandibular canal with mandibular canal variation has clinical significance in such cases. To the best of our knowledge, present study is first study conducted with bifid mandibular canal in literature, in which the study population was grouped as groups with third molars {group A: impacted (A1) and erupted (A2)} and groups without third molars {group B: only third molars missing (B1) and posterior edentulous area (B2)} in which bifid mandibular canal frequency were assessed. The aim of this study was to assess bifid mandibular canals by analysing CBCT images in Turkish population of eastern Anatolia region.
Materials and Methods
A retrospective study was conducted in which 501 CBCT images of 332 patients of age group between 19-71 years were scanned between January 2019 and June 2019 were included. The study was approved by Inonu University Scientific Research and Publication Ethics Committee (number:2018/15-7). In present study 142 images of 89 patients who had impacted third molars, 137 images of 94 patients who had erupted third molars, 84 images of 65 patients who had only third molar missing, and 138 images of 84 patients who did not have any molars and who had posterior edentulous area were assessed. Posterior edentulous area images were obtained from pre operation implant planning patients, while impacted third molar tooth images were obtained from records of patients who had underwent CBCT screening for third molar surgery. CBCT images showing “complete recovery” of extraction socket in edentulous area, the anatomical region between mandible foramen and mental foramen being within the Field of View (FOV), clear appearance of the study area were included and dental implant or graft cases with posterior edentulous area, images with movement artefact, images with metal artefact, cases with metabolic bone disease, images in which fracture has occurred in the study area as a result of trauma, images with pathologies such as cyst and tumour in the study area were excluded.
Evaluation of CBCT Images
CBCT images obtained by using NewTom 5G (Verona, Italy) were used. Exposure parameters were 110 kV, maximum 20 mA and scanning time was 18 seconds and FOV values were 18×16, 15×12 and 12×8, while voxel values were 0.2, 0.25 and 0.3 mm in the images. The images were assessed by an oral radiologist who had a CBCT experience of more than 7 years. For intra observer agreement, after three weeks 30% of the images were reassessed (The intraobserver reliability was assessed for all measurements using the İntraclass Correlation Coefficient (ICC), and ICC was between 0.84 and 0.91). In each CBCT image, bifid mandibular canal presence was recorded with sub-groups depending on gender, and patients as group A (group A1 and A2) and group B (group B1 and B2). After bifid mandibular canal presence was detected in reconstructive panoramic images, it was also confirmed with MPR (Multiplanar reformat) images. Only MPR images were assessed for buccolingual canal presence.
In our study, bifid mandibular canals were grouped according to modified Naitoh classification [7]. According to this classification, 6 groups were assessed as retromolar, dental, forward, buccolingual, bicanal and trifid canal.
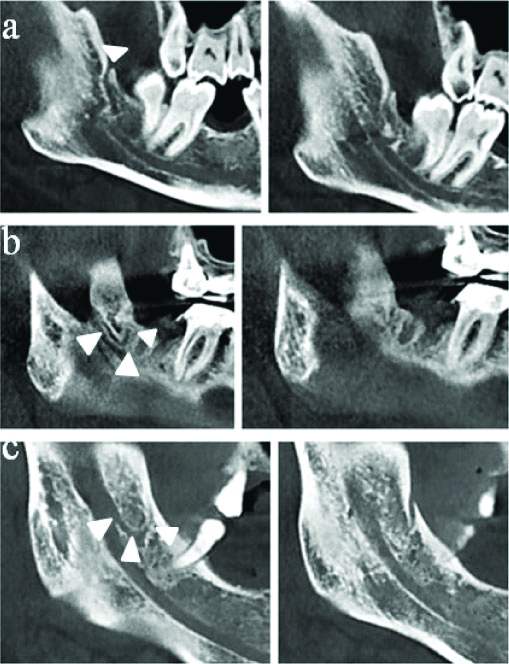
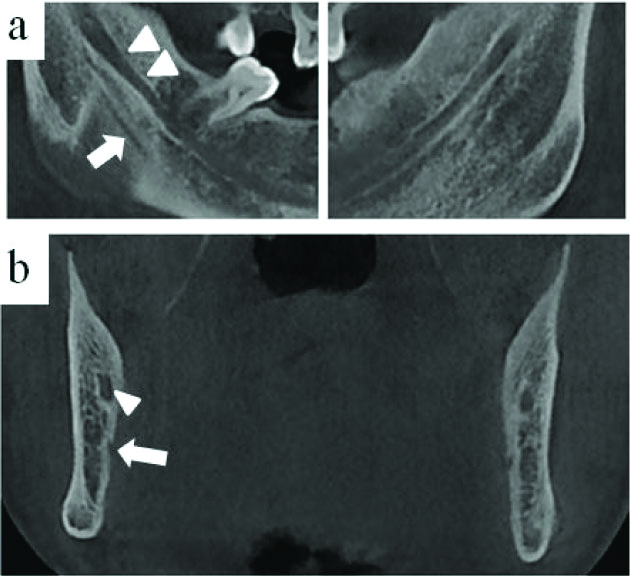
1. Retromolar canal: Bifid canal that leaves the main canal, advances within ramus area and ends with retromolar foramen. Retromolar canal is further grouped in three sub-groups, sub-group 1 that directly reaches the bone surface [Table/Fig-1a], sub-group 2 that makes a single flexion and takes a “V” shape in the retromolar area [Table/Fig-1b] and sub-group 3 that makes double flexions and takes a “U” shape in the retromolar area [Table/Fig-1c].
Three sub-group of retromolar canal (white arrowheads): a) The retromolar canal (sub-group 1) courses directly to the surface of the bone; b) The retromolar canal (sub-group 2) makes a single flexion and takes a “V” shape in the retromolar area; c) The retromolar canal (sub-group 3) that makes double flexions and takes a “U” shape in the retromolar area.
2. Dental canal: Bifid mandibular canal that extends to the roots of third [Table/Fig-2a] or second molars [Table/Fig-2b].
Dental canal: Bifid mandibular canal that extends to the roots of third; a) or second molars; b) (white arrowheads: Main Canal, White arrow: Dental Canal).
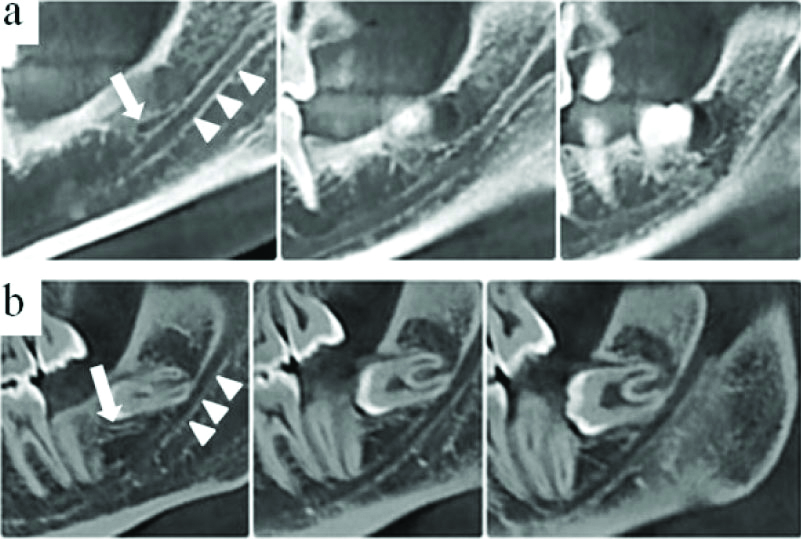
3. Forward canal: Bifid mandibular canal that courses parallel to the main canal by leaving the superior wall of the main canal without confluence [Table/Fig-3a] or the confluence [Table/Fig-3b].
Forward canal: a) forward canal without confluence; b) forward canal with confluence. (white arrowheads: main canal, white arrow: forward canal).
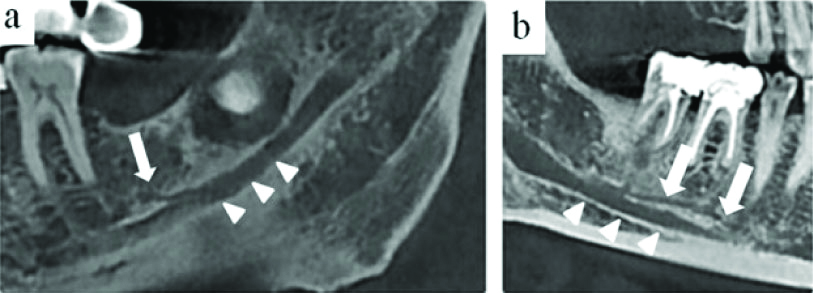
4. Buccolingual canal: Bifid mandibular canal that starts from the buccal [Table/Fig-4a] or lingual [Table/Fig-4b] wall of the main canal.
Buccolingual canal: a&b) white arrowheads: main canal, white arrow: buccolingual canal.
5. Bicanal: A bifid mandibular canal that leaves the inferior of main canal and courses with the anteroinferior of the canal [Table/Fig-5a,b].
Bicanal: a&b) white arrowheads: main canal, white arrow: bifid mandibular canal.
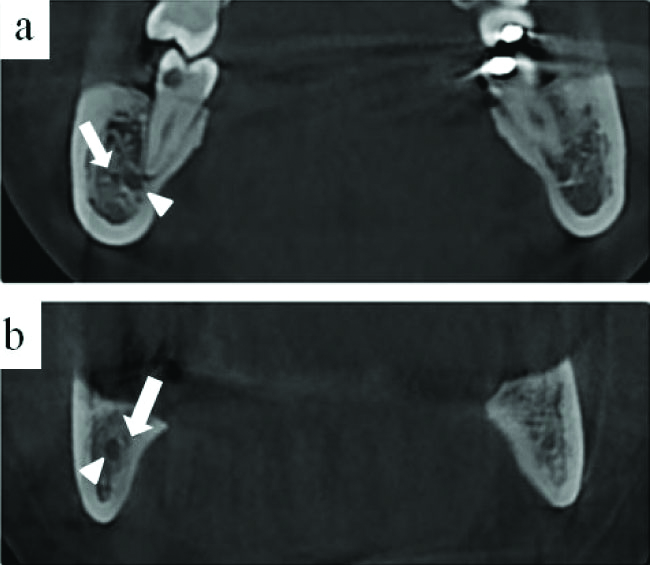
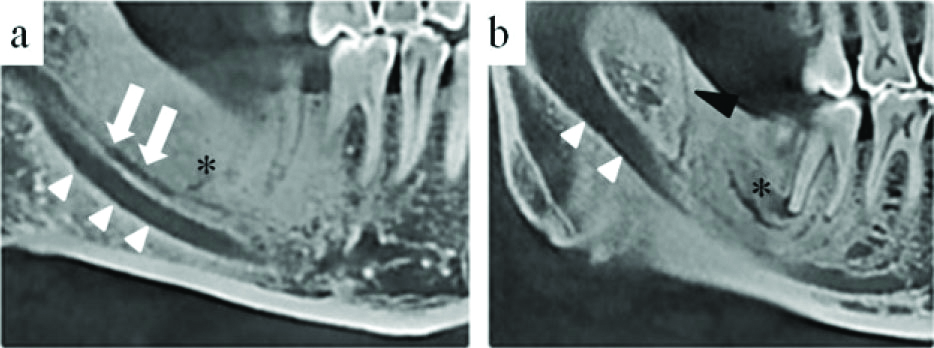
6. Trifid canal: Bifurcation of two bifid canals from one side of the mandibular canal [Table/Fig-6 a,b].
a) Trifid canal (white arrow): a&b) dental canal (asteriks); b) retromolar canal (black arrowheads); and a&b) main canal (white arrowheads).
Statistical Analysis
Statistical analyses were performed by using SPSS 21.0 (SPSS Inc., Chicago, IL) program. Chi-square was used to compare the frequency of canal in group A (group A1 and A2) and group B (group B1 and B2) (p<0.05). Descriptive statistics were used for the bifid mandibular canal sub-type prevalence.
Results
The mean age was found as 36.8 (in women 36.45 and in men 37.19) Of the 332 patients, 151 (45%) were aged 19-29 years, 59 (17.5%) were 30-39 years, 45 (13.5 %) were 40-49 years, 46 (14%) were aged 50-59 years and 31 (9.5 %) were aged 60-71 years. Of the 501 mandibles assessed, bifid mandibular canal was found in 210 (41.9%). While 106 (39.7%) of these bifid mandibular canals were seen in women, 104 (44%) were seen in men. Of the 332 patients the prevalence of bifid mandibular canal was found according to age groups, 42.98% in 19-29 years, 45.78% in 30-39 years, 47.61% in 40-49 years, 37.14% in 50-59 years and 19.56% in 60-71 years. No statistically significant difference was found between women and men [Table/Fig-7], (p=0.283). Of the 279 mandibles in group A, bifid mandibular canal was found in 132 (47.3%), while in group B bifid mandibular canal was found in 78 (35.1%) of 222 mandibles. Statistically significant difference was found between the frequency of bifid mandibular canal being seen in these groups [Table/Fig-7], (p=0.006). While bifid mandibular canal was seen in 65 (45.8%) of 142 mandibles in group A1, in 67 (48.9%) of 137 in group A2. No statistically significant difference was found between the prevalence of bifid mandibular canal in group A1, and group A2 [Table/Fig-7], (p=0.601). Bifid mandibular canal was found in 35 (41.7%) of 84 in group B1; 43 (31.2%) in group B2. No statistically significant difference was found between the group B1 and group B2 [Table/Fig-7], (p=0.112).
Statistical comprasion of the prevelance of bifid canal according to gender, groups and subgroups.
| Presence of Bifid mandibular canal | Evaluated image (501) | Chi-square test |
|---|
| n | % | n | p-value |
|---|
| Male | 104 | 44 | 236 | 0.283 |
| Female | 106 | 39.7 | 265 |
| Group A* | 132 | 47.3 | 279 | 0.006 |
| Group B* | 78 | 35.1 | 222 |
| Group A1* | 65 | 45.8 | 142 | 0.601 |
| Group A2* | 67 | 48.9 | 137 |
| Group B1* | 35 | 41.7 | 84 | 0.112 |
| Group B2* | 43 | 31.2 | 138 |
*Group A: Presence of third molar; Group B: Absence of third molar; Group A1: İmpacted third molar; Group A2: Erupted third molar; Group B1: Only third molar missing mandibula; Group B2: Posterior edentulous mandibula (p-value<0.05)
Bifid mandibular canals types and subgroups were determined in [Table/Fig-8] according to groups (A1, A2, B1, B2).
Prevelance of bifid canal types and subtypes according to subgroups.
| Group | | Group |
|---|
| Type name | A1 | A2 | B1 | B2 | | A1 | A2 | B1 | B2 |
|---|
| n (%) | n (%) | n (%) | n (%) | | n | n | n | n |
|---|
| Retromolar canal(type 1) | 14 (21.5)71 (33.8) | 23 (34.3) | 16 (45.7) | 18 (41.9) | Subtype 1 (direct) | 6 | 15 | 6 | 9 |
| Subtype 2 (V shape) | 3 | 2 | 1 | 3 |
| Subtype 3 (U shape) | 5 | 6 | 9 | 6 |
| Dental canal(type 2) | 26 (40)39 (18.6) | 11 (16.4) | 2 (5.7) | - | extending to third molar | 19 | 10 | - | - |
| extending to second molar | 7 | 1 | 2 | - |
| Forward canal(type 3) | 11 (16.9)63 (30.1) | 21 (31.3) | 12 (34.3) | 19 (44.2) | confluence | 2 | 7 | - | 4 |
| Without confluence | 9 | 14 | 12 | 15 |
| Buccolingual canal(type 4) | 11 (16.9)19 (9) | 6 (9) | - | 2 (4.65) | buccal | 3 | 4 | - | - |
| lingual | 8 | 2 | - | 2 |
| Bicanal(type 5) | 2 (3)11 (5.2) | 5 (7.5) | 1 (2.85) | - | | | | | |
| Trifid canal(type 6) | 1 (1.5)7 (3.3) | 1 (1.5) | 1 (2.85) | 4 (9.3) | Retromolar and forward | - | 1 | - | 4 |
| Retromolar, dental and forward | 1 | - | 1 | - |
| TOTAL | 210 (100) | | | | | | | | |
Discussion
It is very important to know the localisation of mandibular canal with its configurations before surgical procedures involving the mandible [10]. Bifid mandibular canal is a variation of the mandibular canal, the canal is divided into two branches at ramus or body and each branch can include neurovascular bundle [10]. In panoramic radiograph, bifid mandibular canal assessments can be wrong due to superimposition, patient position errors, magnification, distortion and mylohyoid muscle [11]. CBCT is the primary radiological diagnostic method to diagnose bifid mandibular canal correctly and suitably and it is strongly recommended by dentists [12,13].
In studies conducted with CBCT previously, the prevalence of bifid mandibular canal in each mandible were reported as 16.2% in Korean, 22.8% in Spain, 18.42-46.5% in Turkish, 8.4% in Northern China and 15.6-43% in Japan populations [3,5-7,13-15]. In this study which was conducted on Southwest of eastern Anatolia region Turkish population, the prevalence of bifid mandibular canal in 501 mandible of 332 patients was found as 41.9%. This result was in parallel with studies conducted on Turkish population [5].
No statistically significant difference was found in the present study in terms of bifid mandibular canal prevalence between men and women, this result was in parallel with previously conducted studies in literature [3,6,7,14].
In the presence of bifid mandibular canal, problems can occur in local anaesthesia, implant surgery, bone graft procedures, osteotomies and third molar extractions [16-19]. Since bifid mandibular canal is clinically important in third molar extraction and implant surgery, the study population was grouped according to these. In this study, the frequency of bifid mandibular canal in group A was found as 47.3% (A1-45.8%, A2-48.9%). No significant change was found in bifid mandibular frequency between group A1 and group A2 patients who were planned for mandibular third molar surgery. Bifid mandibular canal prevalence was assessed in group B2 for implant planning and it was found as 31.2%. In this study, bifid canal subtypes were assessed according to modified Naitoh M classification [7]. Retromolar type was found as the most frequent type in Zhang Y et al., study with a rate of 68.4%, in Kang JH et al., study with a rate of 52.5%, and in Rashsuren O et al., study with a rate of 71.3% [3,6,20]. In their study, they conducted only with retromolar canal Lizio G et al., found the prevalence of retromolar canal as 14.6% [21]. In this study, retromolar type was found as the most frequent type among bifid mandibular canals with a rate of 33.8%. Of the 71 retromolar canals found in our study, 36 were found as subtype 1, 9 were found as subtype 2 and 26 were found as subtype 3 [Table/Fig-8].
Dental canal prevalence in bifid mandibular canals was found as 8.3% in Orhan K et al., study, as 14.9% in Zhang Y et al., study and as 18.8% in Rashsuren O et al., study [3,5,6]. It was found as 18.6% in current study. While 29 of the 39 dental canals found in our study ended at the third molar root, 10 was found to end at the second molar root. In this study in group B2 dental canal prevalence in bifid mandibular canals was accepted as 0 since there were no molars and only 2 dental types were found in mandibles with only third molars missing. Of the 132 bifid mandibular canals in group A dental type were found as 37 (28%) [Table/Fig-8]. According to this result, it was thought that it would not be right to include mandibles with third and second molars missing while assessing dental canal frequency and it was accepted that the actual value would be 28% and this value was higher than the literature. Since no distinction was made about third molar and second molar absence in the population in studies conducted in the literature, the values they specified about dental canal prevalence was thought to be lower than the normal [3,5,6,14].
The prevalence of forward canal among bifid mandibular canals was found as 4.1% in Rashsuren O et al., study, as 13.7% in Zhang Y et al., study and as 29.8% in Orhan K et al., study [3,5,6]. In this study, forward canal prevalence was found as 30%. While 13 of the 63 forward canals detected in our study were found to be confluence, 50 were found to be without confluence [Table/Fig-8].
In previous study, Orhan K et al., found buccolingual type as 14.5%; Zhang Y et al., found buccolingual type as 0%, bicanal as 0.6%, trifid canal as 2.4% and Rashsuren O et al., found buccolingual type as 0% and trifid canal as 5.8% [3,5,6]. In this study, buccolingual type was found as 9%, while trifid canal was found as 5.2% and bicanal was found as 3.3%. While 7 of the 19 buccolingual canals were in buccal, 12 were found in lingual.
CBCT is a highly suitable method for the detection, confirmation and verification of bifid mandibular canals [22]. It is important to notice the anatomy of the mandibular canal and its variations in order to prevent complications resulting from third molar extraction and implant surgery.
Limitation(s)
Small sample size and retrospective nature of this study is the limitation. Clinical studies with CBCT should be done for implant and third molar surgery.
Conclusion(s)
The prevalence of bifid mandibular canal was found as 41.9% in this study conducted with CBCT. No difference was found between genders in terms of prevalence. Bifid mandibular canal prevalence was found to be higher in group A when compared with group B. Hence, CBCT is a significantly useful tool for the exploration of bifid canals that uses less ionising radiation rather than other 3D imaging systems.
Contribution(s)
ND and SBD: project development, data collection, and manuscript writing.
ND: data analysis.
SBD: manuscript editing.
*Group A: Presence of third molar; Group B: Absence of third molar; Group A1: İmpacted third molar; Group A2: Erupted third molar; Group B1: Only third molar missing mandibula; Group B2: Posterior edentulous mandibula (p-value<0.05)