Immunisation is the most cost-effective health intervention which has a key role in achieving fourteen out of seventeen Sustainable Development Goals. It has been labelled as “One of the Best Buys in Global Health” [1]. WHO estimates that, vaccines save 2-3 million lives and protect millions each year against vaccine-preventable diseases and disabilities [1]. These diseases account for more than half of the total under- five mortality [2]. With improvement in global coverage, an additional 1.5 million deaths can be averted [3].
National Family Health Survey (NFHS) reports improvement in Full Immunisation Coverage of India (FIC) from 43.5% in 2005-06 to 62% in 2015-16. Under-five mortality is also decreased from 74% (2005-06) to 50% (2015-16) [4].
Still, cases of vaccine preventable diseases reported in the country were; Diphtheria: 8788, Pertussis: 13,208, Tetanus: 7,000 and Measles: 19,474 in 2018 [3].
Bihar presents a dismal picture with FIC of 61.7% in 2015-16, which has increased from 32.8% in 2005-06 owing to various strategies like prioritising and focusing on low-performing areas, health system strengthening and newer technologies in monitoring and gap assessment [5-7]. Although, the FIC is comparable to national-level data, the under-five mortality rate is still higher (58 per 1000) and the leading cause is vaccine-preventable disease [5,8].
Of the various factors, effectiveness of vaccination depends on its timely administration also. With delay in vaccination, the duration of susceptibility of the child is increased, which may result in disease outbreaks [9,10]. Studies have suggested that various factors interplay which increase the risk of disease in children not vaccinated timely [11]. The pre-existing conditions such as malnutrition, overcrowding, poor socio-economic status, poor health care facility and access further aggravate the situation. Thus, timely administered vaccines are cost-effective as it reduces burden of hospitalisation and deaths [12]. Also, once delayed, the chances of full Immunisation decreases [13].
Wide variation in timely vaccination has been reported globally. The developed countries exhibit less proportion of children with delayed vaccination than the developing African and South-east Asian countries. Timely vaccination coverage reported at national level was 35% for DPT-1 and 55% for Bacille Calmette Guerin (BCG) at a delay of one month from the recommended date of vaccination; findings of District Level Household and Facility Survey-4 data [14]. Within the country, inter-state variation is also reported [15-17]. Timely vaccination also represents the adequacy of healthcare utilisation and access [18,19].
There is lack of data on timeliness of vaccination in Bihar. Thus, this study aimed to ascertain the timeliness of age-specific vaccination, drop-out rates and the association of timeliness of vaccination with demographic characteristics of household.
Materials and Methods
An observational, cross-sectional study was conducted in 59 low-performing blocks of Bihar in the month of January and February, 2019. The blocks where vaccination coverage was <70% were called low- performing blocks and these were identified through coverage evaluation survey conducted by UNICEF- Bihar.
Children aged 12-23 months formed the study population. Two-stage sampling was performed. In each 59 blocks, 30 villages were selected, using cluster-random sampling with probability proportional to size. First village was selected randomly using computer-generated random number table. For the selection of rest twenty-nine villages, sampling-interval was calculated. From each village, 7 households were selected which had children in the age group of 12-23 months. At the village level, first house was selected randomly (Note-method). For the selection of rest 6 households, house-order was calculated. Following state-level demographic facts were taken into account for the calculation of house-order: Birth Rate of Bihar: 26.8/1000 population [20], Infant Mortality Rate of Bihar: 48/1000 Live Birth, [5] Average Family Size of Bihar: 5.5 [21].
All children aged 12-23 months were included in study who were there at household in the last night provided their caretakers were also present at the time of interview. In the present study, only those children were included in the analysis who had written document of vaccination history in form of vaccination card or mother-child protection card. If the date of vaccination was missing on the vaccination card, such children were excluded from the analysis. Therefore, a total of 9,201 children were included in the analysis.
A semi-structured and pre-tested questionnaire was conceived on the basis of WHO vaccination coverage evaluation format [22]. Questions were translated into Hindi and provided to all data collectors. Data collection was carried out in a mobile-based application “SDRC Collect”. Data collectors were recruited and trained on study collection procedure and study instrument. Before the commencement of data collection, pre-testing of questionnaire and SDRC Collect Application was done in two slums areas of Patna, Bihar. Necessary amendments were made after pre-testing. Informed consent was taken from the caregivers.
Questionnaire included the demographic details comprising of place of residence; rural or urban, date of birth, gender, availability of vaccination card, birth weight, birth order, place of birth and place of vaccination was recorded. Vaccination details such as whether the child was vaccinated against the specific vaccine and the date of vaccination was enquired. The vaccination details of BCG, three doses of Oral Polio Vaccine (OPV) and Pentavalent, two doses of Inactivated Polio Vaccine (IPV) and Pneumococcal Conjugate Vaccine (PCV) and Meningococcal Vaccine (MCV) was asked. In case of unvaccinated child, the reason for non-vaccination was also recorded. The present analysis was conducted on BCG, MCV and three doses of Pentavalent and OPV only. WHO guidelines were used for the calculation of timely vaccination of each vaccine. For BCG, the timely vaccination is taken at 4 weeks, for OPV1 and Pentavalent 1; 2 months, OPV2 and Pentavalent 2; 4 months, and 6 months for OPV3 and Pentavalent 3 and 12 months for MCV [Table/Fig-1].
WHO recommendations for timely vaccination of specific vaccine.
| Vaccine | WHO recommended time range of vaccination |
|---|
| BCG | Birth- 4 weeks |
| Pentavalent 1 | 4 weeks- 2 months |
| OPV 1 | 4 weeks- 2 months |
| Pentavalent 2 | 8 weeks- 4 months |
| OPV2 | 9 weeks- 4 months |
| Pentavalent 3 | 12 weeks- 6 months |
| OPV 3 | 12 weeks- 6 months |
| MCV | 38 weeks- 12 months |
Statistical Analysis
The raw data was obtained in the excel sheet. Duplicate and missing data were cleaned by using the Filter command in excel. STATA 12.0 was used to calculate the proportion of children with timely or delayed vaccination. The median age for timely and delayed vaccinated children was compared using Wilcoxon rank-sum (Mann Whitney Test). The association between timely vaccination and demographic variable was calculated using Chi-square test.
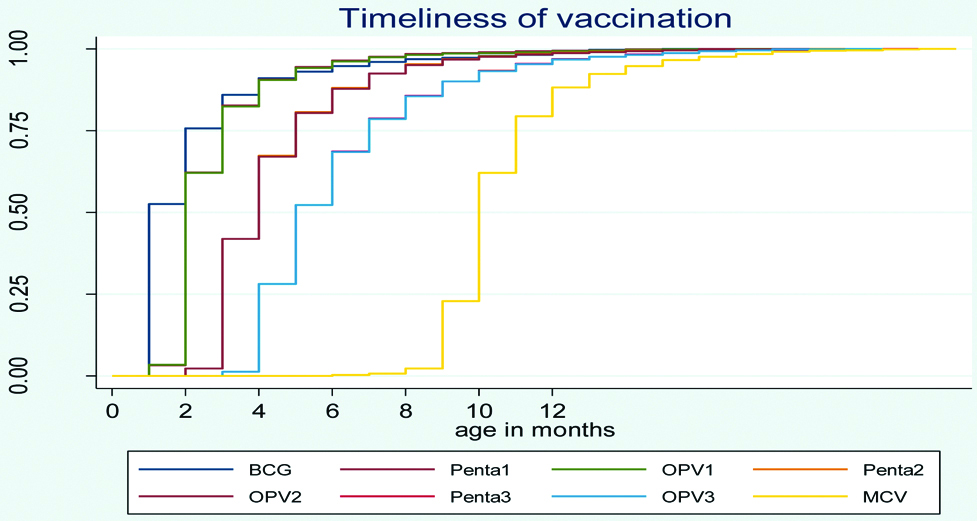
Kaplein-Meier Curve was plotted to study the cumulative vaccination coverage. The event of interest was vaccination of the child at the specific age and the survival time was defined as, age (in months) survived by the child until he is vaccinated. Thus, outcome was vaccination, a positive event. Drop-out rate is calculated for multidose vaccines. For example, the difference in coverage between first and third dose of Pentavalent/OPV and coverage difference between BCG and MCV [22].
Results
The mean age of the participating children was 17.4 months and 53% were male. Majority of the children resided in rural setting were of Hindu religion, belonging to backward caste. The mean birth weight was 2855 gm. Majority of the children had institutional delivery [Table/Fig-2].
Demographic characteristics of 12-23 months old children and their health care utilisation (N=9201).
| Demographic characteristics | N | Proportion |
|---|
| Gender |
| Female | 4300 | 47 |
| Male | 4901 | 53 |
| Place of residence |
| Rural | 7553 | 82 |
| Urban | 1648 | 18 |
| Caste |
| General | 1261 | 14 |
| Other backward caste | 4980 | 54 |
| Scheduled caste | 2398 | 26 |
| Scheduled tribe | 335 | 4 |
| Others | 227 | 3 |
| Religion |
| Hindu | 7470 | 81 |
| Muslim | 1726 | 19 |
| Others | 5 | 0 |
| Birth weight |
| <2500 gm | 666 | 7 |
| >= 2500 gm | 5067 | 55 |
| Data missing | 3468 | 38 |
| Birth order |
| (1-3) | 7824 | 85 |
| (4-6) | 1279 | 14 |
| (>=7) | 87 | 1 |
| Place of delivery |
| Health care facility | 7434 | 81 |
| Home | 1767 | 19 |
| Place of vaccination |
| Govt. health care facility | 8821 | 96 |
| Private health care facility | 266 | 3 |
| Both | 114 | 1 |
The data for 11 children is missing for Birth Order
Timeliness of Vaccination
In the present study, it was found that the coverage for each vaccine was more than ninety percentage. At the time of survey, out of the total 9201 children aged 12-23 months, 8461 children were found to be vaccinated against BCG, three doses of OPV and Pentavalent and one dose of MCV, resulting in an overall coverage of 92% (95% CI: 91.4-92.5%). However, with subsequent doses, the vaccination coverage depicted the falling trend of coverage from BCG to MCV [Table/Fig-3]. A line diagram is also used to plot the timely vaccinated against total vaccinated [Table/Fig-4]. The bars in the figure depicts the vaccinated children while the line diagram is used for timely vaccinated children. Of the total 9201 children, 9140 were reportedly vaccinated against BCG, which gradually dropped down to 8614 who were vaccinated against MCV.
Timeliness of each vaccine among children 12-23 months (n=9201).
| Vaccine | Vaccinated | Timeliness of each vaccine |
|---|
| n (%) | Timely n (%) | Delayed n (%) |
|---|
| BCG | 9140 (99.3%) | 6829 (74.7%) | 2311 (25.8%) |
| Pentavalent 1 | 9128 (99.2%) | 3248 (35.6%) | 5880 (64.4%) |
| OPV 1 | 9116 (99.1%) | 3239 (35.5%) | 5877(64.5%) |
| Pentavalent 2 | 9048 (98.3%) | 5268 (58.2%) | 3780(41.8%) |
| OPV 2 | 9044 (98.3%) | 5255 (58.1%) | 3789(41.9%) |
| Pentavalent 3 | 8943 (97.2%) | 5765 (64.5%) | 3178 (35.5%) |
| OPV 3 | 8931 (97.1%) | 5755 (64.4%) | 3176(35.6%) |
| Measles | 8641 (93.9%) | 8614 (99.7%) | 0027 (0.3%) |
| All antigens | 8461 (92.0%) | 1884 (22.3%) | 6577 (77.7%) |
Comparison of proportion of vaccinated children against timely vaccinated children.
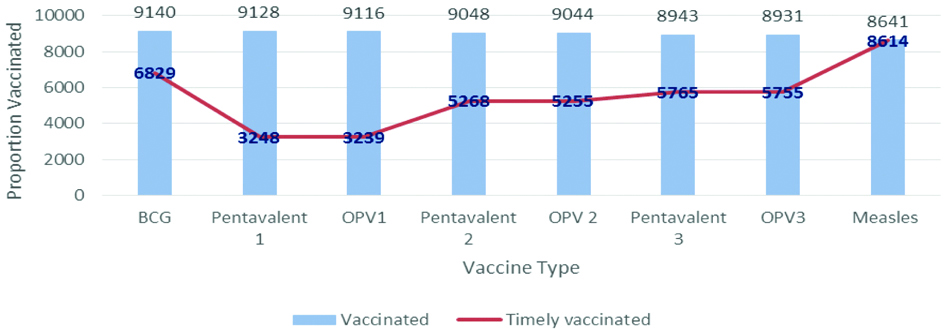
Although, the vaccination coverage for each antigen is fairly high, but it is notable from this survey that the vaccines are not administered timely. Nearly, two out of ten children were only vaccinated timely (20.5%, 95% CI: 19.6-21.3%). Of the total children who were vaccinated against BCG (9140), three- fourth (74.2%) were vaccinated timely. Almost all (99.7%) were vaccinated against MCV within 12 months. However, in case of first dose of Pentavalent and OPV, the proportion of children vaccinated within 2 months was exceptionally low (35.5%).
Cumulative Vaccination Coverage
An inverse Kaplein-Meier curve is plotted against age at vaccination in months for each antigen [Table/Fig-5]. It is evident from the graph that, it takes about 1½ months for 50% of children to get vaccinated against BCG. Similar trend of complete vaccination against Pentavalent and OPV at 5 months was noted. The cumulative incidence curve for each vaccine rose beyond 12 months thus, making the considerable delay in vaccination very apparent. The similar pattern of each curve emphasises the fact that once delayed, the child is delayed for rest of the vaccine. The curve for all doses of Pentavalent and OPV vaccine is overlapping because of the similar scheduled time of vaccination.
Cumulative vaccination coverage for each antigen based on Kaplain-meier method.
Comparison of Median Age at Vaccination in Timely Vaccinated and Delayed Vaccinated Children
In order to study the timeliness of vaccination, 12-23-month-old children were divided in two groups; first group included children vaccinated timely and the second group included delayed vaccinated children and the median age at vaccination was compared for both groups. It can be deduced from the table that with subsequent doses of vaccination the gap between median age of timely and delayed vaccinated children increased as well as the gap between subsequent vaccines also increased. The gap between timely and delayed vaccinated children was 4 weeks for first dose of Pentavalent while 14 weeks for third dose. Also, the gap between 2nd and third dose of Pentavalent and OPV was 6 weeks. The difference in median age in timely and delayed vaccinated children was highly significant for all antigens [Table/Fig-6].
Comparison of median age in timely and delayed vaccinated (12-23 months) children.
| Vaccine | Median age in timely vaccinated children | Median age in delayed vaccinated children |
|---|
| BCG* (in days) | 0 (0-28) | 58 (29-544) |
| Pentavalent 1*# | 7 (6-8) | 11 (9-87) |
| OPV 1*# | 7 (6-8) | 11 (9-96) |
| Pentavalent 2*# | 14 (10-17) | 23 (18-91) |
| OPV 2*# | 14 (10-17) | 23 (18-80) |
| Pentavalent 3*# | 20 (14-26) | 34 (27-97) |
| OPV 3*# | 20 (14-26) | 34 (27-91) |
| MCV* (in months) | 10 (9-12) | 14 (6-23) |
*p-value<0.00, #in weeks
Association of Timely Vaccination with Demographic and Health Care Utilisation Factors
The proportion of children delaying vaccination was maximum for Pentavalent 1. Therefore, the Pentavalent 1 is used to study association between various factors and timely vaccination [Table/Fig-7].
Association between timely vaccination and demographic factors.
| Demographic variables | BCG | | Pentavalent 1 | | Measles | |
|---|
| n (%) | p-value | n (%) | p-value | n (%) | p-value |
|---|
| Gender |
| Female | 3136 (73%) | <0.001 | 1487 (35%) | 0.176 | 3396 (79%) | <0.001 |
| Male | 3693 (75%) | | 1761 (36%) | | 4001 (82%) | |
| Place of residence |
| Urban | 1310 (79%) | <0.001 | 738 (45%) | <0.001 | 6117 (81%) | 0.002 |
| Rural | 5519 (73%) | | 2510 (33%) | | 1280 (78%) | |
| Religion of child |
| Hindu | 5717 (76%) | <0.001 | 2675 (36%) | 0.075 | 6099 (82%) | <0.001 |
| Muslim | 1110 (64%) | | 572 (33%) | | 1293 (75%) | |
| Caste of child |
| General | 931 (74%) | <0.001 | 505 (40%) | 0.001 | 1033 (82%) | <0.001 |
| Backward caste | 3712 (74%) | | 1767 (35%) | | 4011 (80%) | |
| Scheduled caste | 1789 (75%) | | 789 (33%) | | 1922 (80%) | |
| Scheduled tribe | 244 (73%) | | 113 (34%) | | 282 (84%) | |
| Birth weight |
| <2500 gm | 570 (86%) | <0.001 | 221 (33%) | 0.041 | 541 (81%) | 0.882 |
| >= 2500 gm | 4112 (81%) | | 1887 (37%) | | 4128 (81%) | |
| Birth order |
| (1-3) | 5905 (76%) | <0.001 | 2830 (36%) | <0.001 | 6320 (81%) | 0.081 |
| (4-6) | 871 (68%) | | 396 (31%) | | 999(78%) | |
| (>= 7) | 44 (51%) | | 20 (23%) | | 69 (79%) | |
| Place of delivery |
| At home | 792 (45%) | <0.001 | 528 (30%) | <0.001 | 1365 (77%) | <0.001 |
| At health care facility | 6037 (81%) | | 2720 (37%) | | 6032 (81%) | |
| Place of vaccination |
| Govt. health facility | 6537 (74%) | <0.001 | 3059 (35%) | <0.001 | 7104 (80%) | <0.001 |
| Private health facility | 211 (79%) | | 135 (51%) | | 202 (76%) | |
| Both | 81 (71%) | | 54 (47%) | | 91(80%) | |
The factors which were found to be highly significant across all antigens were gender, caste of the child, place of residence, place of delivery and vaccination of the child. Timely vaccination was associated with male gender (BCG: 75%, Penta1: 36%, MCV: 82%), urban place of residence (BCG: 79%, Penta1: 45%, MCV: 81%), and birth at health care facility (BCG: 81%, Penta 1: 37%, MCV: 81%). Although, other factors like caste of the child, birth order, birth weight and place of delivery and vaccination were also significantly associated with timely vaccination but these were not consistent across the groups. A decreasing trend of timely vaccination with increasing birth order was noted in case of all three vaccines (BCG: 76%, Penta 1: 36%, MCV: 81%).
Drop-outs and Left-outs
Vaccines which are given in series are used as proxy to calculate drop-out rates. The drop-out rate depicts the proportion of children who were vaccinated against initial vaccines/doses and then dropped out before completing the vaccination schedule. The first vaccine in series is BCG and last vaccine is MCV for calculation of drop-out rates. The drop-out rate for BCG-MCV series is 5.8%. More than half of these drop-out children belonged to backward and scheduled caste. It was also found that, out of every 100 children only 2 (2%), did not complete vaccination against OPV and Pentavalent. These children fall in the category of left-outs [Table/Fig-8].
Dropout rates of vaccines in series.
| Vaccine in series | Dropout rate n, (%) |
|---|
| BCG-Measles | 556 (6%) |
| Penta 1-Penta 3 | 197 (2.1%) |
| OPV-0-OPV-3 | 206 (2.2%) |
Discussion
The present study ascertains that, although the vaccination coverage at the time of survey for eight antigens was more than 90%, the timely administration was remarkably low at 20%. This pattern clearly reflected in delayed median age at vaccination for each vaccine.
Individual level data from National Family and Health Survey-4 (2015-16) reports proportion of delayed children against BCG, DPT-1 and Measles as 27.8%, 43.6% and 46.7%, respectively [23]. Although, in present study, the delayed proportion was almost comparable to NFHS-4 data for BCG vaccine, while that for Pentavalent1 was exceptionally high and for measles, very low.
Timely vaccination among infants against BCG, strongly suggests the impact of institutional delivery which has improved significantly from 19.9% in 2005-06 to 63.8% in 2015-16 in the state [5]. The strikingly low timely coverage of Pentavalent 1 and OPV 1 was found comparable across all the districts surveyed. The analysis of District Level Household Survey 4 reports the timely coverage for BCG at 1 month, Pentavalent 1 at 2 months and MCV at 12 months to be 55%, 48%, 71%, respectively [14]. The low coverage of Pentavalent 1 reported at national level corroborates with findings of our study. It can be speculated that the communication gap in delivering key messages to beneficiaries, fear of Adverse Event Followling Immunisation (AEFI), could be possible reasons for low coverage.
However, a study from rural setting of south-India reports the proportion of children with delayed vaccination against DPT1, DPT3 and MCV to be 7.4%, 64.6% and 38.8%, respectively [15].
The median age of vaccination in timely and delayed vaccinated children was compared. Even in timely vaccinated children, the vaccination was not done at recommended time except for BCG. Similar pattern of delay was observed in the NFHS-4 study which reported that the median age at vaccination against BCG; 4 days, DPT1; 66 days and MCV; 300 days [23]. Similar findings were reported from a study which was conducted on birth cohorts 2002-04 by Yadav K et al., in Ballabgarh [24]. The median age for BCG was 3.2 weeks, DPT3 19 weeks, MCV 43.5 weeks. However, the data of Bihar is comparable 15 years down the line.
On the contrary, the study conducted at a rural setting in Puducherry, states that the median delay in vaccination from their due dates were only 1 day for BCG, 7 days for Penta1, 14 days for Penta 3 and 18 days for MCV [25]. Role of community volunteers in improving timely vaccination was demonstrated by a cohort study conducted by Prinja S et al., in Haryana. In this study, the median delay in DPT series was found to decrease in post-intervention phase [26].
Demographic factors such as female gender, high birth order, Muslim religion were found to be associated significantly with delay in vaccination. Similarly, it was also reported that children who were born at health facility received vaccination timely compared to children who were delivered at home. These observations are corroborated by findings of many studies both nationally and internationally [16,27-29]. These pre-existing established risk factors were found to be significantly associated with delayed vaccination, representing gaps in achieving FIC.
The dropout rates for BCG-MCV were 6%. Similar rate was reported in a cross-sectional study conducted in Ghana [30]. Also, in our study the dropout rate between first and third dose of Pentavalent and OPV series was 2%. The dropout rates reported from a study conducted in rural area of Tripura was 3.9% only [31]. On the contrary, the same reported by studies conducted in slums of Mumbai was 12.8% for DPT1-DPT3 [32] and that reported from rural block of Rohtak, Haryana was 13.9% for BCG-Measles [33]. The main reasons as found in this study were vaccine unavailability, lack of information about vaccination, inconvenient vaccination timings and fear of adverse events following Immunisation. Above mentioned studies have also reported similar factors for vaccination drop-outs [29,30,33].
The strength of the study is first, the robust sample size. The survey was conducted over a large representative sample. Second, the authenticity of the data collection was ensured through, 3-day training of data collectors, pre-testing of questionnaire and SDRC Collect mobile app in urban slums of Patna, incorporation of GPS tracking during data collection and proficiency of data collectors in local dialect.
Limitation(s)
The main limitation of the study is that mother’s education was not assessed.
Conclusion(s)
Achieving timely vaccination has emerged as a challenge in the study. Only one-fifth of children were vaccinated timely. Even though, vaccinated on time, these children were vaccinated at later dates of time window. Of the various demographic factors influencing the timeliness of vaccination, delivery at the health care facility was found to be associated significantly. Thus, strengthening the health care facility through improving its accessibility and availability will also influence timeliness of vaccination. This study also helps us to identify the pockets of low-coverage and drop-out children. Thus, focused intervention in these pockets through gap assessment and comprehensive monitoring should be strengthened. Besides these, dissemination of key messages and counselling should also be emphasised in order to allay fear of adverse events following immunisation and to make population realise importance of timely immunisation in combating preventable disease.
The data for 11 children is missing for Birth Order