Letter Regarding the Article, ‘Hyponatremia in Patients Admitted with Stroke’; From the Viewpoint of Similarity to Hyponatremia Associated with Traumatic Brain Injury
Takahiko Nagamine1
1 Doctor, Department of Emergency Medicine, Matsumoto Surgical Hospital, Sunlight Brain Research Centre, Hofu, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Takahiko Nagamine, Sunlight Brain Research Centre, 4-13-18 Jiyugaoka, Hofu, Yamaguchi-747-0066, Japan.
E-mail: tnagamine@outlook.com
Dear Editor,
With great interest, i read the article “Hyponatremia in Patients Admitted with Stroke” by Karunanandham S et al., [1]. They indicated that hyponatremia is very common in these patients and that Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) and Cerebral Salt Wasting Syndrome (CSWS) are the main aetiologies. They also emphasised that distinguishing between SIADH and CSWS is crucial because treatment of these two syndromes is quite different. I deeply agree with these comments because I recently experienced severe hyponatremia associated with Traumatic Brain Injury (TBI), which is similar to hyponatremia with stroke.
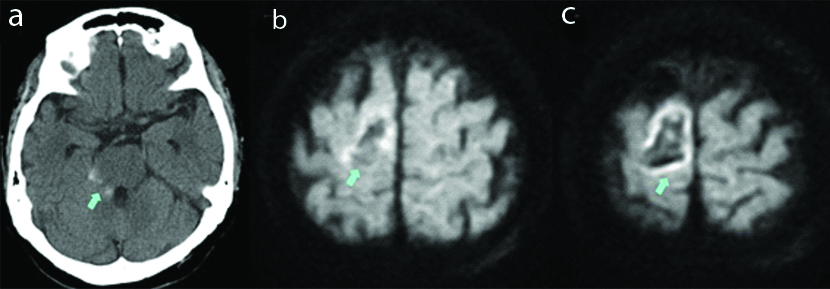
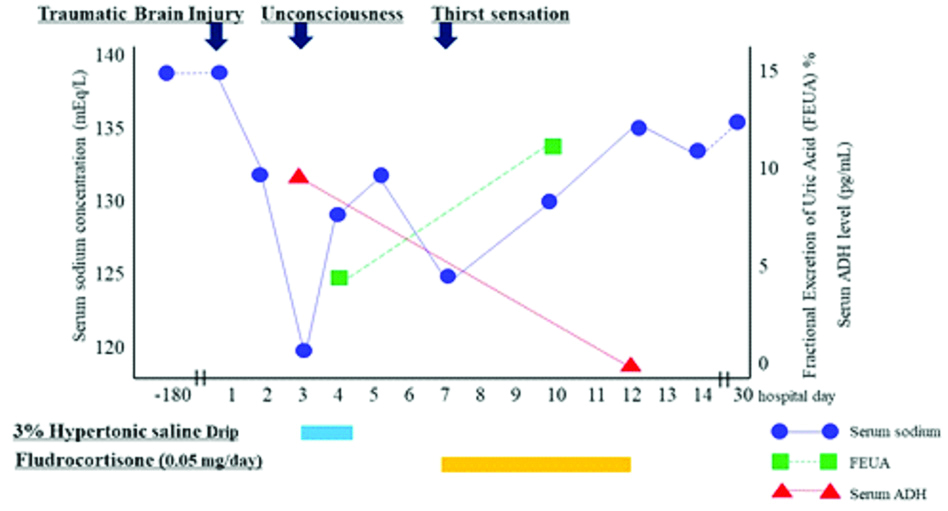
An 82-year-old female was admitted to our hospital because of headache after a fall. On arrival, her consciousness was quite clear. Radiological examination revealed traumatic subarachnoid haemorrhage and brain contusion [Table/Fig-1]. On the third hospital day, her consciousness suddenly became drowsy and her serum sodium level dropped to 119 mEq/L. Her plasma osmolality was 238 mOsm/kg H20, whereas urine osmolality was 466 mOsm/kg H20. The serum Antidiuretic Hormone (ADH) concentration increased to 9.8 pg/mL despite severe hyponatremia. On the fourth hospital day, her serum sodium level increased to 129 mEq/L with 3% hypertonic saline drip at 20~30 mL/hour, resulted in improvement in her consciousness level. The Fractional Excretion of Uric Acid (FEUA) was 4.8%, indicative of SIADH [2]. On the seventh hospital day, however, she reported severe thirst sensation and increased urination, and her serum sodium level at this time decreased to 126 mEq/L again. Therefore, considering the possibility of CSWS, fludrocortisone (0.05 mg/day) was administered. On the tenth hospital day, her serum sodium level increased to 132 mEq/L and the FEUA at this time was 10.9 %, indicative of CSWS [2]. She was finally diagnosed as having SIADH followed by CSWS caused by TBI. The clinical course of the patient is illustrated in [Table/Fig-2].
Radiological study on admission; a) Brain Computed Tomography (CT) on arrival revealing Subarachnoid Haemorrhage (SAH) in the right ambient cistern (arrow indicated). b,c) Brain Magnetic Resonance Imaging (MRI) at the time of admission showing bleeding with edema in the right temporo-parietal lobe on the diffusion weighted image (arrow).
Clinical course; change in the patient’s serum sodium levels, ADH levels, and the Fractional Excretion of Uric Acid (FEUA).
Brain damage interferes with the normal neuroendocrine function of the hypothalamus and the pituitary system, thus secreting ADH and/or natriuretic peptides and impairing sympathetic neural input to the juxtaglomerular apparatus, which leads to water reabsorption and/or an increase in sodium excretion, resulted in SIADH or CSWS [3]. To make matters worse, SIADH and CSWS may occur in one patient like the index case. The main problem of SIADH is fluid excess and hyponatremia is dilutional in nature, while CSWS is characterised by extracellular fluid volume depletion caused by increased natriuresis. Thus, distinguishing these syndromes is essential in order to correct hyponatremia adequately as Karunanandham S et al., pointed out [1]. However, distinguishing between both syndromes is difficult because accurate volume status is difficult to be determined.
In conclusion, an analogy between stroke and TBI in terms of the risk of hyponatremia can be drawn. Management of hyponatremia after brain damage is challenging because SIADH and CSWS may occur consecutively. Clinicians should be aware of SIADH and CSWS in patients with brain damage to allow for accurate diagnosis and treatment of these conditions, which require different treatments.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? NA
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 25, 2019
Manual Googling: Jan 08, 2020
iThenticate Software: Jan 25, 2020 (11%)
[1]. Karunanandham S, Rajappa T, Sevaraju K, Hyponatremia in patients admitted with strokeJ Clin Diag Res 2018 12(8):OC34-36.10.7860/JCDR/2018/36176.11954 [Google Scholar] [CrossRef]
[2]. Maesaka JK, Imbriano LJ, Miyawaki N, Determining fractional urate excretion rates in hyponatremic conditions and improved methods to distinguish cerebral/renal salt wasting from the syndrome of inappropriate secretion of antidiuretic hormoneFront Med (Lausanne) 2018 5:31910.3389/fmed.2018.0031930560127 [Google Scholar] [CrossRef] [PubMed]
[3]. Tudor RM, Thompson CJ, Posterior pituitary dysfunction following traumatic brain injury: ReviewPituitary 2019 22(3):296-304.10.1007/s11102-018-0917-z30334138 [Google Scholar] [CrossRef] [PubMed]