Variation in the Branching Pattern of Superior Thoracic Artery- A Rare Case
Saikarthik Jayakumar1, Gunapriya Raghunath2, Karthiga Kannan3, Anand Paramasivam4, Saraswathi Ilango5
1 Assistant Professor, Department of Basic Medical Sciences Anatomy, Majmaah University, Zulfi, Riyadh, Saudi Arabia.
2 Professor, Department of Anatomy, Saveetha Medical College, Chennai, Tamil Nadu, India.
3 Professor, Department of Oral Medicine, Majmaah University, Zulfi, Riyadh, Saudi Arabia.
4 Professor, Department of Basic Medical Sciences, Physiology, Majmaah University, Zulfi, Saudi Arabia.
5 Assistant Professor, Department of Physiology, Madha Medical College, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Saikarthik Jayakumar, Majmaah University, Zulfi, Riyadh, Saudi Arabia.
E-mail: SAI41RAD@GMAIL.COM; s.jaya@mu.edu.sa
Superior thoracic artery is usually a branch from the first part of axillary artery. It descends down up to the 2nd intercostal space and anastomose with internal thoracic and intercostal arteries. However, during routine dissection for medical students it was observed that the superior thoracic artery on the right side showed unusual branching pattern, dividing into medial and lateral branches. The lateral branch coursed around the medial wall of axilla horizontally superficial to the long thoracic nerve of bell which divided into medial and lateral branch. This variation is of radiological, surgical and morphogenic importance as no such branching pattern have been described in the literature previously.
Axillary artery, 1st part, Morphogenesis, Variation
Case Report
Among ten cadavers that were dissected during routine dissection in the axilla region for medical students at Madha Medical College and Research Institute, one cadaver (male with age approximately around 50 years) had a unilateral variation in the course of the Superior Thoracic Artery (STA) on the right side limb alone [Table/Fig-1] and the left side had no such variations [Table/Fig-2]. The rest of its 5 branches of axillary artery did not show any variation. The present case has a rare variation where the STA divides into medial and lateral branches and in turn the lateral branch again divides into two terminal medial and lateral branch [Table/Fig-2,3]. STA raised from 1st part of axillary artery and at the level of 2nd rib the artery divided into two prominent branches in an inverted ‘T’ shaped manner unusually.
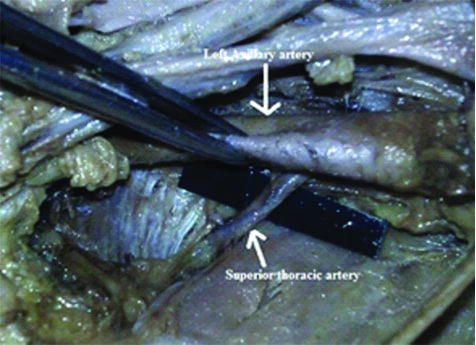
Shows the normal left side axillary artery (White arrow shows axillary artery- top, superior thoracic artery- bottom).
shows the right side axillary artery. Note the variation in the branching pattern of STA when compared to its usual course on the right side (In Table/Fig. 2 White arrow points the axillary artery- top, bend arrow points superior thoracic artery and the bottom arrow points the variant medial and lateral branches of STA. In Table/Fig. 3 the white arrow in the left points on the long thoracic nerve, the middle and right arrow points the variant medial and lateral branches of STA)
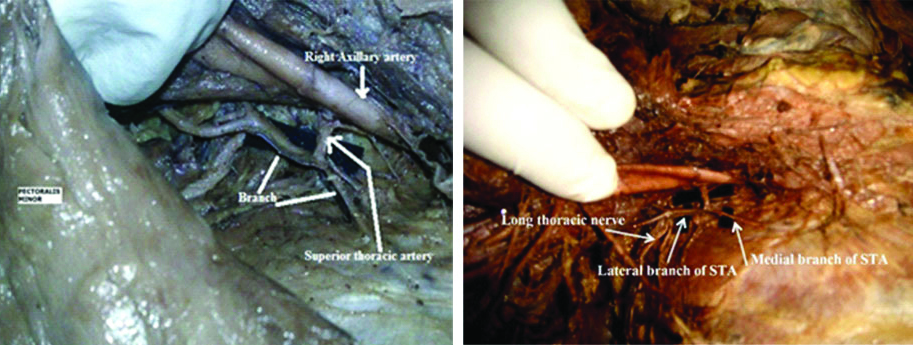
The medial branch followed the usual course of axillary artery and supplied the 1st intercostal space. The lateral branch had a variant course towards the medial wall of axilla. The STA divided into a medial branch and a lateral branch which again divided into ‘Y’ shaped branch-upper and lower running deep towards subscapularis muscle. This lateral branch was found superficial to long thoracic nerve of Bell and coursed laterally along the medial wall of axilla [Table/Fig-3]. No such variation has been reported in the literature. Since this variation was noted during routine dissection, no ethical approval was needed.
Discussion
Axillary artery is a continuation of subclavian artery and a number of variations have been noted thus far [1-3]. Variations in course, branches, double axillary artery have all been described [4,5]. Anatomically axillary artery is divided into 3 parts by pectoralis minor muscle, the proximal being the first part and the distal being the 3rd part. The 1st part gives one branch –STA, the 2nd part gives two branches – thoraco-acromial and lateral thoracic artery, the 3rd part gives three branches – anterior and posterior circumflex artery, subscapular artery. Apart from the usually named 6 branches, other branches such as superior subscapular artery and alar thoracic artery were described by Huelke, (1959) [6]. The abnormal branching pattern of axillary artery is less common in male than in females [1].
The axillary artery develops from the seventh cervical segmental artery and any morphological variation in its branching pattern is linked to its development [7]. De Garis CF and Swartley WB (1928) described 23 different types of axillary artery which showed greater tendency of variation amongst the African race than in Caucasians [4]. There is also found to be a sex difference in the branching pattern with female showing more variation than males [8]. Astik R and Dave U reported incidence of variation in axillary artery can be as high as upto 62.5% [9]. The most common variations in STA that were reported in the literature usually are; a) arising from 3rd part of subclavian artery; b) in few cases STA was absent [6]; c) could arise from thoraco-acromial trunk [1]; d) arising as second branch of 1st part of axillary artery – the first branch being an aberrant one supplying serratus anterior [10].
Usually STA is small branch in case of males and it courses down beneath subclavius muscle and anastomose with internal thoracic artery and intercostal arteries [11]. There can be numerous reasons of the variation in normal branching pattern of axillary artery and it could be due to the defects of neighbouring tissue and also defects in embryonic vascular network development. Variations in axillary artery are not unusual [Table/Fig-4] [12-23].
Shows the variations in the branching pattern of axillary artery.
| Author | Year | Finding |
|---|
| Cavdar S et al., [12] | 2000 | Third part of axillary artery gave 2 branches- superficial and deep brachial arteries which gave rise to various branches. The superficial brachial artery divided into radial and ulnar artery |
| Jacquemin G et al., [13] | 2001 | Bilateral origin of superficial ulnar artery from the axillary artery with different courses in two limbs |
| Saeed M et al., [14] | 2002 | Variations in branching pattern in subclavian and axillary systems. |
| Natsis K et al., [15] | 2006 | High origin of superficial ulnar artery on the right side with a looped course |
| Venieratos D and Lolis ED, [16] | 2001 | Common trunk from the third part of axillary artery dividing into various branches |
| Panagouli E et al., [17] | 2009 | Superficial ulnar artery from the second part of axillary artery on the right side. On the left side, a single common trunk from the second part dividing into two branches. |
| Daimi SR et al., [18] | 2010 | First part giving rise to thoracoacromial trunk and two posterior circumflex humeral arteries and high origin of radial arteries |
| Sawant SP et al., [19] | 2012 | Superior thoracic, lateral thoracic, thoraco-acromial arteries raised from deep part of axillary artery which was found have two parts- superficial and deep axillary artery |
| Gaur S et al., [20] | 2012 | Variation in the branches of axillary artery is more common on the second part. |
| Naveen K et al., [21] | 2014 | Profundabrachii artery originated from the 3rd part of axillary artery |
| Aastha AJ and Kumar MS, [22] | 2015 | Superior thoracic artery passes between two divisions of lateral cord and third part gave a single common trunk. |
| Ezzati M et al., [23] | 2018 | Common trunk in the second part of axillary artery, which divided into Lateral Thoracic, Subscapular arteries and then muscular branches. |
Many of the branches may arise as a common trunk or constant branches may arise separately in different part of the axillary artery [24]. Previous literatures have shown that variations in the first part is very rare [12] and more common on the second part of axillary artery (Gaur S et al., 2012) [20]. Among the usually named 6 branches, lateral thoracic, subscapular artery (87%) and Posterior Circumflex-humeral Artery (PCA) (86.5%) are most common branches of variable origin. When PCA arises from deep brachial artery it passes through the lower triangular space along with radial nerve rather than in the quadrangular space with axillary nerve [25]. In the present case, the lateral branch of STA is in close proximity with the long thoracic nerve [Table/Fig-3,5]. It can also be noted that, this lateral branch bifurcates over the surface of the nerve. The places of arterial bifurcation are sites where aneurysms are more prone to happen due to higher haemodynamic stress at such sites. Such an aneurysm may compress long thoracic nerve there by leading to deficits in the function of serratus anterior muscle [26].
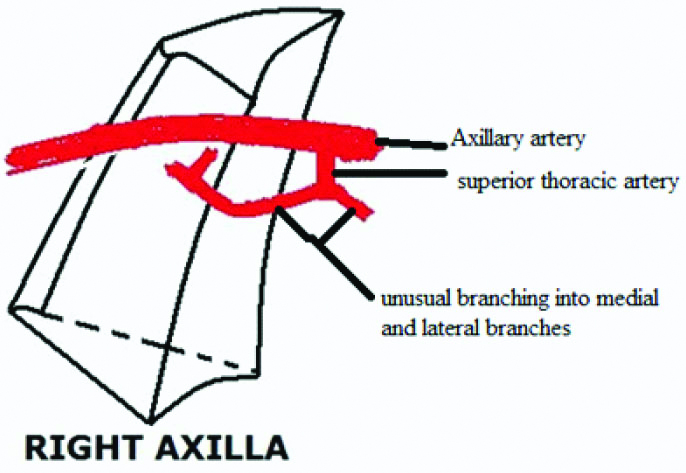
Schematic representation of the case report.
Formation of vascular system involves vasculogenesis and vascular remodelling. Genetic regulation may be a vital factor in the formation of blood vessels during the early stages of development, however in later stages blood flow plays a pivotal role in the formation of blood vessels. The plasticity of blood vessels is determined by various genes such as ephrin B2 (for arteries) and neuropilin- 2 (for veins) which is one of the factor playing a role in branching morphogenesis [27,28]. Studies have shown apart from the normal genetic expression which controls branching points, haemodynamics (hypoxia) and cardiac output regulation also determines the branching morphogenesis [29]. The present case is unique because of its variation in branching pattern where there might have been an area of tissue hypoxia during embryogenesis along the axilla, which would have probably upregulated hypoxia induced factor–1 gene to trigger sprouting from primitive vascular capillaries to that region. Failure of such anomalous branch to regress might have caused this sort of a distinctive changes in branching morphology of STA even though genetic and other factors cannot be ruled out.
Deep seated axillary abscess is usually drained along the medial wall of axilla as the other 3 walls of axilla contains important neurovascular structures namely lateral thoracic, axillary and subscapular arteries along the anterior, lateral and posterior walls respectively [30]. Sound knowledge of the vascular variations is important for surgeons during mastectomy with axillary clearance for CA-breast, to anaesthesiologist and orthopaedic surgeons considering the frequency of procedures done in this region for instance on the humerus. Since this variant branch is in close proximity with shoulder joint, utmost care should be taken during any interventional procedure to not injure such variant branch of STA.
Conclusion(s)
Variations in axillary artery are very common but a variation in the branching pattern of STA is very rare. During coronary bypass grafting as well as other reconstructive surgeries of the axillary artery after trauma, vascular grafts from branches of upper extremities arteries are used. For accurate diagnosis of underlying pathology in the axillary region, a thorough knowledge of variant and normal anatomy is vital for vascular radiologist, clinical anatomist and surgeons.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. Na
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 21, 2019
Manual Googling: Dec 30, 2019
iThenticate Software: Jan 23, 2020 (12%)
[1]. Pandey SK, Gangopadhyay AN, Tripathi SK, Shukla VK, Anatomical variations in termination of the axillary artery and its clinical implicationsMed Sci Law 2004 44(1):61-66.10.1258/rsmmsl.44.1.6114984216 [Google Scholar] [CrossRef] [PubMed]
[2]. Valnicek SM, Mosher M, Hopkins JK, Rockwell WB, The subscapular arterial tree as a source of microvascular arterial graftsPlast Reconstr. Surg 2004 113(7):2001-05.10.1097/01.PRS.0000122235.09892.DA15253189 [Google Scholar] [CrossRef] [PubMed]
[3]. Moore KL, Dalley AF, Clinically oriented Anatomy 2014 7th edPhiladelphiaLippincott Williams & Wilkins:713-30. [Google Scholar]
[4]. De Garis CF, Swartley WB, The axillary artery in White and Negro stocksAm J Anat 1928 41:35310.1002/aja.1000410208 [Google Scholar] [CrossRef]
[5]. Hollinshead WH, Anatomy for surgeons in general surgery of the upper limbThe back and limbs 1985 New YorkA Heber Harper Book:290-300. [Google Scholar]
[6]. Huelke DF, Variations in origin of branches of the axillary arteryAnatomical Record 1959 135(1):33-41.10.1002/ar.1091350105 [Google Scholar] [CrossRef]
[7]. Wollard HH, The development of the principal arterial stems in the forelimb of the pigContrib Embryol 1922 14:139 [Google Scholar]
[8]. Trottler M, Henderson JL, Gass H, Brua RS, Weisman S, Agrecs H, The origins of branches of the axillary artery in whites and in American NegroesAnat Rec 1930 46:13310.1002/ar.1090460205 [Google Scholar] [CrossRef]
[9]. Astik R, Dave U, Variations in branching pattern of the axillary artery: A study in 40 human cadaversJ Vasc Bras 2012 11(1):12-17.10.1590/S1677-54492012000100003 [Google Scholar] [CrossRef]
[10]. Orhan M, Nuket GM, Bari C, Multiple variations in the axillary arterial tree relevant to plastic surgery: A case reportInternational Journal of Morphology 2007 25(2):357-62.10.4067/S0717-95022007000200020 [Google Scholar] [CrossRef]
[11]. Birch R, Pectoral girdle and upper limb. In: Susan Standring, EditorGrays anatomy- The anatomical basis of clinical practice 2016 41st editionLondonElsevier:776-862. [Google Scholar]
[12]. Cavdar S, Zeybek A, Bayramicli M, Rare variation of the axillary arteryClin Anat 2000 13(1):66-68.10.1002/(SICI)1098-2353(2000)13:1<66::AID-CA8>3.0.CO;2-M [Google Scholar] [CrossRef]
[13]. Jacquemin G, Lemaire V, Medot M, Fissette J, Bilateral case of superficial ulnar artery originating from axillary arterySurg Radiol Anat 2001 23:139-43.10.1007/s00276-001-0139-211462864 [Google Scholar] [CrossRef] [PubMed]
[14]. Saeed M, Rufai AA, Elsayed SE, Sadiq MS, Variations in subclavian-axillary arterial systemSaudi Med J 2002 23:208-12. [Google Scholar]
[15]. Natsis K, Papadopoulou AL, Paraskevas G, Totlis T, Tsikaras P, High origin of a superficial ulnar artery arising from the axillary artery: Anatomy, embryology, clinical significance and a review of the literatureFolia Morphol (Warsz) 2006 65:400-05. [Google Scholar]
[16]. Venieratos D, Lolis ED, Abnormal ramification of axillary artery: Sub-scapularcommon trunkMorphologie 2001 85(270):23-24. [Google Scholar]
[17]. Panagouli E, Tsaraklis A, Gazouli I, Anagnostopoulou S, Venieratos D, A rare variation of the axillary artery combined contralaterally with an unusual high origin of a superficial ulnar artery: Description, review of the literature and embryological analysisItal J Anat Embryol 2009 114:145-56. [Google Scholar]
[18]. Daimi SR, Siddiqui AU, Wabale RN, Variations in the branching pattern of axillary artery with high origin of radial artery. A case reportInt J Anat Variations 2010 3:76-77. [Google Scholar]
[19]. Sawant SP, Shaikh ST, More RM, The Study of variations in the branches of axillary arteryInter J Adv Physiol Allied Sci 2012 1:01-07./10.5455/ijmsph.2012.143-146 [Google Scholar] [CrossRef]
[20]. Gaur S, Katariya SK, Vaishnani H, Wani IN, Bondre KV, Shah GV, A cadaveric study of branching pattern of the axillary arteryInt J Biol Med Res 2012 3:1388-91. [Google Scholar]
[21]. Naveen K, Jyothsna P, Nayak SB, Mohandas RKG, Swamy RS, Deepthinath R, Variant origin of an arterial trunk from axillaryartery continuing as profundabrachii artery- A unique arterial variation in the axillaand its clinical implicationsEthiop J Health Sci 2014 24(1):93-96.10.4314/ejhs.v24i1.1324591805 [Google Scholar] [CrossRef] [PubMed]
[22]. Aastha AJ, Kumar MS, an unusual variation of axillary artery: A case reportJournal of Clinical And Diagnostic Research 2015 9:05-08. [Google Scholar]
[23]. Ezzati M, Nasrabadi HT, Abedelahi A, Bahlakeh G, Kheirjou R, Ataei ML, Variations in the branches of axillary arteryInt J Anat Var 2018 11(3):75-76. [Google Scholar]
[24]. Hollinshed WH, Anatomy for surgeons in general surgery of the upper limb. The back and limbs 1958 New YorkA Heber Harper book:290-300. [Google Scholar]
[25]. Farhan T, Selman M, Anatomical study of axillary artery variationJ Fac Med Baghdad 2010 52(3):324-27. [Google Scholar]
[26]. Alfano JM, Kolega J, Natarajan SK, Xiang J, Paluch RA, Levy EI, Intracranial aneurysms occur more frequently at bifurcation sites that typically experience higher haemodynamic stressNeurosurgery 2013 73(3):497-505.10.1227/NEU.000000000000001623756745 [Google Scholar] [CrossRef] [PubMed]
[27]. Wani MA, Means RT Jr, Lingrel JB, Loss of LKLF function results in embryonic lethality in miceTransgenic Res 1998 7:229-38.10.1023/A:10088098098439859212 [Google Scholar] [CrossRef] [PubMed]
[28]. Gerety SS, Anderson DJ, Cardiovascular ephrinB2 function is essential for embryonic angiogenesisDevelopment 2002 129:1397-410. [Google Scholar]
[29]. Jones EA, le Noble F, Eichmann A, What Determines Blood Vessel Structure? Genetic Prespecification vs. HemodynamicsPhysiology 2006 21:388-95.10.1152/physiol.00020.200617119151 [Google Scholar] [CrossRef] [PubMed]
[30]. Datta AK, Axilla. Textbook in Essentials of human anatomy 2012 4th edKolkataCurrent books international:47-52. [Google Scholar]