Introduction
Pre-Eclampsia (PE) is a pregnancy-specific disorder which further complicates and leads to eclampsia. The Factor V Leiden (FVL) is an autosomal dominant genetic abnormality with incomplete penetrance predisposes to thrombosis. It codes for Factor V, as it is a missense mutation where arginine is replaced by glutamine. The FVL is a heterozygous condition which has risk of complicated pregnancy outcomes.
Aim
To find out association between the Factor V Leiden Mutation (FVLM) and PE.
Materials and Methods
The study was designed as case-control, where 150 PE gravid women were cases and 150 healthy normotensive gravid women were controls enrolled from the Department of Obstetrics and Gynaecology in RL Jalappa Hospital and Research Centre, Tamaka, Kolar, Karnataka, India. The methodology for maternal FVLM adopted was, isolation of the Deoxyribo Nucleic Acid (DNA) by using salting-out method followed by Polymerase Chain Reaction and Restricted Fragment Length Polymorphism (PCR-RFLP) with MNL1 enzyme. On digestion FVL allele was visible as an uncut 268 base pair fragment with PCR while the Leiden was cleaved to produce 163 and 67 base pair fragments (wild type). The 37 base pair fragment was not visible on the gel due to its small size. Homozygous Leiden mutation produces two bands corresponding to 200 base pair and 67 base pair (homozygous Leiden) for heterozygous Leiden Mutation four bands corresponding to 200 base pair, 163 base pair, 67 base pair, 37 base pair (heterozygous/Wild Type/mutant Leiden). Statistical analysis was done by using the SPSS software 13. The difference in frequency between two groups was not statistically significant.
Results
Frequency of the leiden variant was 5.3% among cases and 6.7% in the control groups. Leiden variant of factor V in homozygous condition was not found in either of the study groups.
Conclusion
FVLM is not a significant marker for PE in the Kolar population.
Blood coagulation, Missense, Mutation, Pregnancy
Introduction
PE is a pregnancy complicated hypertensive disorder which usually occurs before eclampsia [1,2]. PE is a syndrome characterised by an increase in Blood Pressure (BP) 140/90 mmHg, oedema, proteinuria 300 mg/L for 24 hours of the urinary collection which occurs after the 20th week of gestation and often complicated by renal failure and coagulopathy [2]. The global prevalence of PE is 2-8% [3]. In India, its incidence is about 28.7%, whereas in the southern India particularly in Karnataka and Andhra Pradesh, it is 19.8%, 21.0%, respectively [4]. It is a foremost obstetric confront as it majorly contributes to maternal and perinatal mortality and morbidity by complicating the pregnancy with seizures, increase in BP further complicates to eclampsia and death [1]. However, it affects even the growth of foetus by causing intra uterine growth retardation, foetal insufficiency, intra uterine death. At present, the only available therapeutic option is the removal of placenta [5].
PE is a complex genetic disorder, follows the autosomal dominant pattern of Mendelian inheritance. PE occurs as a result of numerous common variants at different loci which individually have small effects collectively add to an individual’s susceptibility. By previous studies, it is evident that no single cause or genetic variant will account for all the cases of PE [6]. For the development of PE apart from genetic risk factors like genotypes of mother and foetus individually and combined, a heterozygous condition in mother or family, family history of hypertension and PE. Other factors like endothelial dysfunction, inflammation, and coagulopathy will have combined effect [7]. However, the different variants and candidate gene approaches are associated with various subsets of disease conditions [6]. Overall, 70 biological candidate, genes were examined. The list of genes is as follows:
Vasoactive proteins: Angiotensinogen, Angiotensin-converting enzyme.
Thrombophilia and hypofibrinolysis: FVL, Methylene Tetra Hydro Folate Reductase, Prothrombin, and Plasminogen Activator Inhibitor-I.
Oxidative stress and lipid metabolism: Apolipoprotein E, Microsomal epoxide hydrolase, glutathione S-transferase.
Endothelial injury: Vascular Endothelial Growth Factor Receptor-1, Vascular Endothelial Growth Factor.
Immunogenetics: Tumour necrosis factor α, Interleukin 10 [6].
FVLM of Thrombophilia is an autosomal dominant genetic condition that exhibits incomplete variable penetrance [8]. FVLM is a gene for clotting Factor V. In coagulation cascade Factor V is converted to Factor Va in presence of active protein C. Due to FVLM there will be resistance in acquired protein C. This leads to thrombophilic condition in veins and spiral arteries. As pregnancy itself is a stressful condition, FVLM increases the risk of clotting [8]. As in PE placental ischemia and endothelial damage occur and reduces the uteroplacental perfusion. This alters the uteroplacental vasculature like an incomplete trophoblastic invasion of spiral arteries. This leads to an imbalance in haemostasis system [7]. For FVLM with thrombophilia is an added risk for PE. The changes like endothelial damage, uteroplacental insufficiency were initiated during placentation or due to any pre-existing factors are still imprecise. As some changes are evident in PE after the 20th week of gestation, but some pre-existing factors like thrombophilia, abnormality in blood clotting proteins these factors are there before pregnancy or it is expressing during PE pregnancy is left over as indistinct [9]. FVLM in thrombophilia was observed 1 in 1000 of the homozygous condition [10] and heterozygous condition is 1 in 500 [11]. There was a paucity of data regarding the study of FVLM and PE due to inconsistency in results, especially in the southern part of India. This is the second study in the south eastern part of India and the first study in Karnataka, India. So this makes us find out the fact of whether there was an association between FVLM and PE in Kolar population. The study aim was to find out the association between FVLM in PE (Kolar population).
Materials and Methods
Study Design and Participants
In this prospective case-control study 300 subjects, (150 in each group) were enrolled from the Department of Obstetrics and Gynaecology from August 2014 to July 2015 in RL Jalappa Hospital attached to Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar, Karnataka, India. The sample size was calculated by using Open Epiweb tool www.OpenEpi.com with 95% confidence interval and 80% power, (updated and accessed April 04, 2013, May 23, 2016). The diagnostic criteria of PE by Department of Obstetrics and Gynaecology in RL Jalappa Hospital and Research Centre was based on American College of Obstetrics and Gynaecologist is as follows [12]:
Systolic blood pressure of ≥140 and160 mmHg; and
Diastolic blood pressure of ≥90 and110 mm Hg on 2 occasions with 2/hours, 2 weeks of gap after 20th week of gestation;
Proteinuria with ≥300 mg per 24 hours of urine collection or protein/creatinine ratio of ≥0.3 on dip stick reading is +1;
In absence of proteinuria thrombocytopenia with a platelet count of ≤100000/ microliter;
Renal insufficiency (Serum creatinine ≥1.1 mg/dL/doubling concentration without any renal disorders);
Impaired liver functions (double the values of the normal range of liver transaminases);
Pulmonary oedema, cerebral or visual disturbances.
Inclusion Criteria
Both primigravida and multigravida in the age group of 18-45 years with clinically diagnosed as PE.
Exclusion Criteria
Pregnant women with eclampsia, chronic hypertension, and a pregnant woman less than 20 weeks of gestation.
Control Group
Normotensive pregnant women who had no complication till delivery, no history of hypertension, PE or Eclampsia.
Ethics: After approval from the institutional research ethical committee clearance with number: No.DMC/KLR/IEC-CEC/167/2015-2016 the study was initiated. Informed consent was obtained from each participant before enrolment.
Sample collection and DNA isolation: About 3 mL of peripheral venous blood was collected in EDTA vacutainer and stored at 4°C till further analysis. DNA was isolated from the peripheral blood lymphocytes using salting-out method [13]. The quality of sample was determined by UV spectrophotometry (Perkin Elmer model Lambda 35, USA).
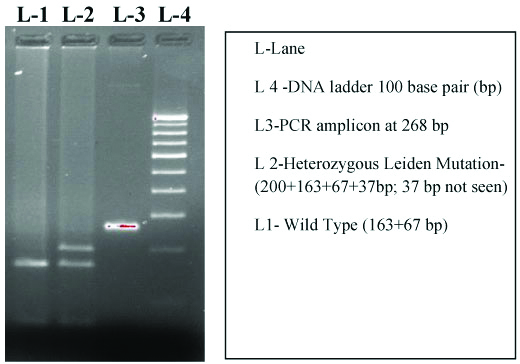
Genotyping of FVL: FVLM gene polymorphism with forward primers 5’TGCCCAGTGCTTA ACAAGACCA3” and reverse primers are 5’ TGTTAT CACACTG GTGCTAA 3″ (Bangalore Genei, India) explained in [Table/Fig-1]. Genomic DNA was amplified by PCR [14] on Bio-Rad C1000 Touch Thermal Cycler. The polymorphic region was amplified with primer pairs explained in [Table/Fig-1]. The 20 μL reaction mixture included 1x assay buffer, 100 ng genomic DNA, 0.2 mMdNTP, 1 picomole of each primer, 2.5 mM MgCl2 and 1 unit Taq DNA polymerase (Bangalore Genei, India). The program comprised of an initial denaturation at 95°C for 3 minutes followed by 35 cycles at 95°C for 30 seconds, 58°C for 30 seconds and 72°C for 30 seconds; final extension involved 10 minutes at 72°C. The 268 bp amplicon was subjected to restriction digestion with 5 units of Mnl I (New England Biolabs, USA) at 37°C for 3 hours and analysed on 3% agarose gel with ethidium bromide staining. On digestion of the FVL allele, PCR products with heterozygous, homozygous Leiden mutation, wild type was explained in [Table/Fig-2]. The diagrammatic representation of PCR products and RFLP with heterozygous Leiden mutation, wild type was explained in [Table/Fig-3].
Representing Factor V Gene polymorphism, location on chromosome, nucleotide, amino acid substitution with PCR and RFLP.
| Gene | Chromosome location | Nucleotide | Aminoacid substitution | SNP/rs no | Forward primers | Reverse primers | RFLP enzyme |
|---|
| Factor V | 1q24.2 | 1691 | Arginine to glutamine at 506 | Exon 10/rs 6020 | 5’TGCCCAGTGCTTAACAAGACCA3″ | 5’TGTTATCACACTGGTGCTAA3″ | MNL137°C3 hours |
| PCR amplicon | Homozygous | Heterozygous | Wild type |
|---|
| 268 bp | 200 bp, 67 bp | 200 bp,163 bp, 67 bp, 37 bp | 163 bp, 67 bp |
Representing agarose gel image with PCR product and RFLP for FVLM.
Statistical Analysis
Statistical analysis was done using the Statistical Packages for Social Sciences software (SPSS, Windows version release 13, SPSS Inc., Chicago, Illinois, USA). Differences in allele frequencies and genotype distribution between cases and controls were compared using relevant contingency tables by Fisher’s-exact test. Quantitative variables were compared with student’s t-test.
Results
A total of 300 participants were included in the study. Of these, 150 samples were from PE women as cases and the remaining 150 were controls as normotensive pregnant women. The maternal age, gestational week, blood pressure readings were taken in both cases and in controls. The mean of maternal age did not show much significance in cases to controls as in cases the mean was 24.2±4.1 and controls were 25.2±3.7 so maternal age is not a major factor in PE. Gestational weeks in cases were 35.4±2.0 in controls were 38.0±1.4 with significant p-value so, it means with PE more chance for early delivery. Around 99% of the cases had oedema. The summary of the clinical profile of the patients was given in [Table/Fig-4]. Due to PE, the complications were not only in mother but even foetus had adverse effects [Table/Fig-5]. Total of 88 cases has shown complications due to PE like foetal distress, Intra Uterine Fetal Death/Demise (IUFD), Intra Uterine Death (IUD), Feto-Placental Insufficiency (FPI), Intra Uterine Growth Restriction (IUGR) has explained with type of PE and type of gravida in [Table/Fig-5]. (Remaining 62 cases of foetus did not showed above complications due to PE). The profile of FVL genotype in the two study groups was shown in [Table/Fig-6]. Frequency of the Leiden variant was 5.3% among cases and 6.7% in the control groups. The Leiden variant of factor V was not found in homozygous condition in either of the study groups. As the heterozygous condition is more in controls the FVLM was not significant in PE of South eastern part of India (Kolar). The distribution of Factor V genotypes in the study population explained in [Table/Fig-6,7] shows the Gravida and type of PE affecting the Wild type mutation and mutant Leiden in cases [Table/Fig-8], explains about the Gravida of PE effecting the Wild type mutation and mutant Leiden (heterozygous type) in controls. The statistical evaluation of the FVL genotypes with PE was explained in [Table/Fig-9].
Clinical profile of PE in the FVL study.
| Clinical parameters | Cases | Controls | p-value |
|---|
| Maternal age | 24.2±4.1 | 25.2±3.7 | 0.025 |
| Gestational age at delivery (weeks) | 35.4±2.0 | 38.0±1.4 | 0.001* |
| Systole blood pressure (mm/hg) | 149.93±19.1 | 111.7±6.89 | 0.001* |
| Diastole blood pressure (mm/hg) | 101.77±13.3 | 75.33±4.39 | 0.001* |
| Blood pressure (mm/hg) Systolic/Diastolic |
| Mild PE | 141.3±11.6/94.7±5.8 | | |
| Severe PE | 170.0±18.5/112.4±5.6 | | |
p-value calculated by Fischer’s-exact test; *p=0.001 (significant)
Maternal and Neonatal complications due to PE.
| Clinical complications | No. of subjects (88) | Primi gravida +Mild PE | Primi gravida +Severe PE | Multi gravida +Mild PE | Multi gravida +Severe PE |
|---|
| Fetal distress | 26 | 12 | 07 | 03 | 04 |
| IUGR | 13 | 04 | 05 | 02 | 02 |
| Twin pregnancy | 02 | - | 01 | - | 01 |
| First pregnancy PE, repeated in second pregnancy | 04 | - | - | 02 | 02 |
| Anaemia with PE | 09 | 03 | 02 | 04 | - |
| FPI | 08 | 02 | 02 | 01 | 03 |
| PE pregnancy complicated to eclampsia | 06 | - | - | 03 | 03 |
| Preterm Delivery due to PE | 02 | - | 02 | - | - |
| IUFD | 09 | 02 | 01 | 03 | 04 |
| Hypothyroidism with PE | 09 | 02 | 02 | 03 | 02 |
IUGR: Intra uterine growth restriction; FPI: Foeto-placental insufficiency; IUFD: Intra uterine fetal death/demise
Distribution of factor V genotypes in the study population.
| Factor V genotype | Cases (n=150) | Controls (n=150) | p-value |
|---|
| WT/WT | 142 (94.7%) | 140 (93.3%) | 1.0 |
| WT/Mut Leiden | 8 (5.3%) | 10 (6.7%) |
| Mut Leiden/Mut Leiden | 0 | 0 |
p-value calculated by Fischer’s-exact test
Gravida and type of PE effecting the wild type mutation and mutant leiden in cases.
| Gravida and Type of PE | WT/MutLeiden | WT/WT |
|---|
| Multi gravida-mild | 01 | 34 |
| Severe | 02 | 25 |
| Total | 03 | 59 |
| Primi gravida-mild | 04 | 52 |
| Severe | 01 | 31 |
| Total | 05 | 83 |
Gravida of PE effecting the wild type mutation and mutant Leiden (heterozygous type) in controls.
| Gravida | WT/Mut Leiden | WT/WT |
|---|
| Multi gravida | 05 | 100 |
| Primigravida | 05 | 40 |
Statistical evaluation of FVL genotypes with PE.
| Genetic model | Dominant WT/WT+WT/MutLeidenvs.MutLeiden/MutLeiden | RecessiveWT/WT vs. WT/Mut Leiden+MutLeiden/MutLeiden |
|---|
| Cases | 150 vs. 0 | 142 vs. 8 |
| Control | 150 vs. 0 | 140 vs.10 |
| p-value | - | 0.4 |
p-value calculated by Fischer’s-exact test
Discussion
The risk factors differ with ethnicity, maternal age and dietary factors. So each subject is not same even of same age group and same gravida. Few studies have been piloted on FVLM and PE. Hardly studies were evaluated on FVLM and thrombophilia in relation to PE. But none of the studies proved that FVLM can be a genetic marker for PE. As PE itself is a multifactorial disorder, genetically complex to understand and often associated with ethnicity may be difficult to find out specific marker [15]. So the present study focused on association of FVLM and PE. Aggarwal S et al., in his study mentioned that there was association between PE and FVL SNP. The study analysis proved the positive association between PE and FVLM with Odds Ratio (OR) of 2.08. Separate analysis of mild and severe PE showed higher association with the mild PE (OR=2.15) than the severe PE (OR=1.9) [16]. The frequency in the south Indian population fails to indicate a statistically significant association between PE and FVLM [17]. A study from south Indian population from Hyderabad with 105 PE subjects and 100 normotensive pregnant women author found no statistical significance with FVLM in PE [17]. Present study matches with these results. Previous studies from outside India have found both positive and negative association between PE and FVLM. In a meta-analysis conducted by Kosmas IP et al., included 19 studies revealed a positive association between FVLM and PE with 2.5 fold increase risk [18]. Karimi S et al., in their study, mentioned about German and Indonesian women in which German women had association and Indonesian women were not associated. So FVL carrier frequency has been shown to vary between ethnicities [15]. The polymorphism of FVLM in thrombophilia has not been observed in Japan, Southeast Asia and Africa. The frequency of FVLM is as high as 15% was reported in the European populations [19]. In another meta-analysis done by Wang X et al., with 37 studies with 5048 PE patients and 6796 controls in Portuguese population the OR for the association between FVL and all PE patients was 1.60 (95%CI 1.28-2.00) and 2.45 (95%CI 1.63-3.69) for the cases of severe PE [20]. A massive meta-analysis of 31 studies involving 7522 patients revealed a positive association between FVLM and PE. The pooled OR association of FVL was 1.81 but the value of OR increased to 2.24 when the cases of severe PE tested separately [21]. The studies with association and disassociation with FVLM in PE were explained in [Table/Fig-10] [15-17,18,20-34]. However in India, FVLM has been examined for association with PE in North Indian population- Lucknow by Aggarwal S et al., with 200 PE and 200 normotensive pregnant women were compared for the frequency of Leiden mutation and found to be 4%. Further mutation increased the risk by two fold (OR: 2.08, p-value 0.03) [16]. Present study findings were same as study done in south Indian population by Kamineni V et al., in south-eastern Indian population. Both studies showed FVLM was not statistically significant. In this light, the data obtained in this study suggest that FVL may not be a relevant marker for PE in the south Indian population [17]. Present data suggest that carriers of the FVL mutation are at increased risk for severe PE.
Studies in relation with FVL mutation in PE [15-17,18,20-34].
| Sl. No. | Author-Year | Country | Associated/Not |
|---|
| 1. | Wang X et al., 2014 (M) [20] | Portugal | Associated with severe PE |
| 2. | Karimi S et al., 2012 [15] | Iran | Associated |
| 3. | Hiltunen LM et al., 2010 [22] | Finland | Associated |
| 4. | Kahn SR et al., 2009 (MC) [23] | Montreal-Cannada | Not associated |
| 5. | Dudding T et al., 2008 (M) [24] | Australia | Associated |
| 6. | Mutze S et al., 2008 (R) [25] | Germany | Not associated |
| 7. | Zahed LF et al., 2006 [26] | Lebanon | Not associated |
| 8. | Nurk E et al., 2006 [27] | Hordaland-Bergan | Associated |
| 9. | Mello G et al., 2005 [28] | Italy | Associated with severe PE |
| 10. | Davalos IP et al., 2005 [29] | Mexico | Not associated |
| 11. | Lin J et al., 2005 [21] (M) | USA | Associated with severe PE |
| 12. | Prasmusinto D et al., 2004 [30] | Germany | Associated |
| 13. | Prasmusinto et al., 2004 [30] | Indonesia | Not associated |
| 14. | Salomon O et al., 2004 [31] | Israel | Not associated |
| 15. | Kosmos IP et al., 2003 (M) [31] | Loannia-Greece | Associated |
| 16. | Rigó J Jr et al., 2000 [33] | Hungary | Associated |
| 17. | Kupferminc MJ et al., 2000 [34] | Israel | Associated |
| 18. | Dizon-Townson DS et al., 1996 [35] | USA | Associated with severe PE |
| 19. | Aggarwal S et al., 2011 [16] | Lucknow-North India | Associated |
| 20. | Kamineni V et al., 2015 [17] | Hyderabad-South India | Not associated |
| 21. | Present study | Kolar-South India | Not associated |
MC: Multi-centric cohor; M-Meta-analysis; R-Review
Limitation(s) and Future Research Aspects
Genetic screening on FVLM in both mother and foetus and also in couples (mother and father) was to be performed. Women who carry FVLM along with thrombophilia are at increased risk for PE so FVLM with thrombophilia in PE subjects has to be screened. The Carriers of thrombophilic mutations has to be screened.
Conclusion(s)
In this case-control study the FVL gene polymorphism lack significant association in the PE women (Kolar population) so it may not be a relevant genetic marker for South Indian population.
Declaration: Author has presented the article in 2016 at Natcon Conference.
p-value calculated by Fischer’s-exact test; *p=0.001 (significant)
IUGR: Intra uterine growth restriction; FPI: Foeto-placental insufficiency; IUFD: Intra uterine fetal death/demise
p-value calculated by Fischer’s-exact test
p-value calculated by Fischer’s-exact test
MC: Multi-centric cohor; M-Meta-analysis; R-Review
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 27, 2019
Manual Googling: Jan 01, 2020
iThenticate Software: Jan 23, 2020 (21%)
[1]. Sachan R, Patel ML, Sachan P, Gaurav A, Singh M, Bansal B, Outcomes in hypertensive disorders of pregnancy in the North Indian populationInt J Womens Health 2013 5:101-08.10.2147/IJWH.S4047323687451 [Google Scholar] [CrossRef] [PubMed]
[2]. Petla LT, Chikkala R, Ratnakar KS, Kodati V, Sritharan V, Biomarkers for the management of pre-eclampsia in pregnant womenIndian J Med Res 2013 138:60-67. [Google Scholar]
[3]. WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia. 2011; ISBN 978-92-4-154833-5 [Google Scholar]
[4]. Agrawal S, Walia GK, Prevalence and risk factors for symptoms suggestive of pre-eclampsia in Indian womenJ Womens Health Issues Care 2014 3:610.4172/2325-9795.1000169 [Google Scholar] [CrossRef]
[5]. Powe CE, Levine RJ, Karumanchi SA, Preeclampsia, a disease of the maternal endothelium: The role of anti-angiogenic factors and implications for later cardiovascular diseaseCirculation 2011 123(24):01-27.10.1161/CIRCULATIONAHA.109.85312721690502 [Google Scholar] [CrossRef] [PubMed]
[6]. Williams PJ, Pipikin FB, The genetics of preeclampsia and other hypertensive disorders of pregnancyBest Practice & Research Clinical Obstetrics and Gynecology 2011 25:405-17.10.1016/j.bpobgyn.2011.02.00721429808 [Google Scholar] [CrossRef] [PubMed]
[7]. Spina V, Aleandri V, Morini F, The impact of the factor V Leiden mutation on pregnancyHum Reprod Update 2000 6(3):301-06.10.1093/humupd/6.3.30110874575 [Google Scholar] [CrossRef] [PubMed]
[8]. Babker AMA, Elzaki SG, Dafallah SE, The role of thrombophilia in recurrent pregnancy lossWorld Journal of Pharmaceutical Research 2015 4(10):191-201. [Google Scholar]
[9]. Garg N, Polipalli SK, Kapoor S, Genetic conflicts and pathophysiological changes in pregnancy: A risk factor for pre-eclampsiaInt J Pharm Sci 2015 4(11):549-83. [Google Scholar]
[10]. Makris M, Factor V Leiden: To test or not to test, that is the debateBlood Transfus 2012 10:255-56. [Google Scholar]
[11]. Battinelli EM, Marshall A, Connors JM, The role of thrombophilia in pregnancyThrombosis 2013 :1-9.10.1155/2013/51642024455235 [Google Scholar] [CrossRef] [PubMed]
[12]. Shu C, Liu Z, Cui L, Wei C, Wang S, Tang JJ, Protein profiling of preeclampsia placental tissuesPLoS ONE 2014 9(11):e11289010.1371/journal.pone.011289025392996 [Google Scholar] [CrossRef] [PubMed]
[13]. Miller SA, Dykes DD, Polesky HF, A simple salting out procedure for extracting DNA from human nucleated cellsNucleic Acids Res 1988 16(3):121510.1093/nar/16.3.12153344216 [Google Scholar] [CrossRef] [PubMed]
[14]. Abdullah WZ, Kumaraguru S, Ghazali S, Dip Yusoff NM, Factor V Leiden and Prothrombin G20210 a mutations among healthy Indians in MalaysiaLabmedicine 2010 41(5):284-87.10.1309/LM9W9L8GQPCZVAYO [Google Scholar] [CrossRef]
[15]. Karimi S, Yavarian M, Azinfar A, Rajaei M, Kootenaee MA, Evaluation the frequency of Factor V Leiden Mutation in pregnant women with preeclampsia syndrome in an Iranian populationIran J Reprod Med 2012 10(1):59-66. [Google Scholar]
[16]. Aggarwal S, Dimri N, Tandon I, Agarwal S, Preeclampsia in North Indian women: The contribution of genetic polymorphismsObstet Gynaecol 2011 37(10):1335-41.10.1111/j.1447-0756.2010.01523.x21564405 [Google Scholar] [CrossRef] [PubMed]
[17]. Kamineni V, Khan IA, Vattam KK, Poornima S, Hassan S, Influence of thrombophilic genes: MTHFR (C677T), FVL (G1691A), ACE(I28005D) in pregnant women with pre-eclampsiaObstet Gynecol Int J 2015 2(1):01-07.10.15406/ogij.2015.02.00023 [Google Scholar] [CrossRef]
[18]. Kosmas IP, Tatsioni A, Ioannidis JP, Association of Leiden mutation in factor V gene with hypertension in pregnancy and pre-eclampsia: A meta-analysisJ Hypertens 2003 21:1221-28.10.1097/00004872-200307000-0000212817161 [Google Scholar] [CrossRef] [PubMed]
[19]. Kujovich JL, Factor V Leiden thrombophiliaGenet Med 2011 13(1):01-16.10.1097/GIM.0b013e3181faa0f221116184 [Google Scholar] [CrossRef] [PubMed]
[20]. Wang X, Bai T, Liu S, Pan H, Wang B, Association between thrombophilia gene polymorphisms and preeclampsia: A meta-analysisPLos One 2014 26(9):e100789doi: 10.1371/journal.pone.0100789. e Collection 201410.1371/journal.pone.010078924967675 [Google Scholar] [CrossRef] [PubMed]
[21]. Lin J, August P, Genetic thrombophilias and preeclampsia: a meta-analysisObstet Gynecol 2005 105(1):182-92.10.1097/01.AOG.0000146250.85561.e915625161 [Google Scholar] [CrossRef] [PubMed]
[22]. Hiltunen LM, Laivuori H, Rautanen A, Kaaja R, Kere J, Krusius T, Factor V Leiden as risk factor for unexplained stillbirth- A population-based nested case-control studyThromb Res 2010 125:505-10.10.1016/j.thromres.2009.09.01619828176 [Google Scholar] [CrossRef] [PubMed]
[23]. Kahn SR, Platt R, McNamara H, Rozen R, Chen MF, Genest J Jr, Inherited thrombophilia and preeclampsia within a multicenter cohort: The montreal preeclampsia studyAm J Obstet Gynecol 2009 200:15-59.10.1016/j.ajog.2008.09.02319070828 [Google Scholar] [CrossRef] [PubMed]
[24]. Dudding T, Heron J, Thakkinstian A, Nurk E, Golding J, Pembrey M, Factor V Leiden is associated with pre-eclampsia but not with fetal growth restriction: A genetic association study and meta-analysisJ Thromb Haemost 2008 6:1869-75.10.1111/j.1538-7836.2008.03134.x18752569 [Google Scholar] [CrossRef] [PubMed]
[25]. Mutze S, Rudnik-Schoneborn S, Zerres K, Rath W, Genes and the preeclampsia syndromeJ Perinat Med 2008 36:38-58.10.1515/JPM.2008.00418184097 [Google Scholar] [CrossRef] [PubMed]
[26]. Zahed LF, Rayes RF, Mahfouz RA, Taher AT, Maarouf HH, Nassar AH, Prevalence of factor V Leiden, prothrombin and methylene tetrahydrofolate reductase mutations in women with adverse pregnancy outcomes in lebanonAm J Obstet Gynecol 2006 195:1114-18.10.1016/j.ajog.2006.06.08217000243 [Google Scholar] [CrossRef] [PubMed]
[27]. Nurk E, Tell GS, Refsum H, Ueland PM, Vollset SE, Factor V Leiden, pregnancy complications and adverse outcomes: The hordaland homocysteine studyQJM 2006 99:289-98.10.1093/qjmed/hcl04016613994 [Google Scholar] [CrossRef] [PubMed]
[28]. Mello G, Parretti E, Marozio L, Pizzi C, Lojacono A, Thrombophilia is significantly associated with severe preeclampsia: Results of a large-scale, case-controlled studyHypertension 2005 46:1270-74.10.1161/01.HYP.0000188979.74172.4d16246971 [Google Scholar] [CrossRef] [PubMed]
[29]. Dávalos IP, Moran MC, Martínez-Abundis E, González-Ortiz M, Flores-Martínez SE, Machorro V, Methylenetetrahydrofolate reductase c677t polymorphism and factor V Leiden variant in mexican women with preeclampsia/eclampsiaBlood Cells Mol Dis 2005 35:66-69.10.1016/j.bcmd.2005.03.00815905108 [Google Scholar] [CrossRef] [PubMed]
[30]. Prasmusinto D, Skrablin S, Fimmers R, van der Ven K, Ethnic differences in the association of factor V Leiden mutation and the c677t methylenetetrahydrofolate reductase gene polymorphism with preeclampsiaEur J Obstet Gynecol Reprod Biol 2004 112:162-69.10.1016/S0301-2115(03)00314-2 [Google Scholar] [CrossRef]
[31]. Salomon O, Seligsohn U, Steinberg DM, Zalel Y, Lerner A, Rosenberg N, The common prothrombotic factors in nulliparous women do not compromise blood flow in the feto-maternal circulation and are not associated with preeclampsia or intrauterine growth restrictionAm J Obstet Gynecol 2004 191:2002-09.10.1016/j.ajog.2004.07.05315592283 [Google Scholar] [CrossRef] [PubMed]
[32]. Kosmas IP, Tatsioni A, Ioannidis JP, Association of Leiden mutation in factor V gene with hypertension in pregnancy and pre-eclampsia: A meta-analysisJ Hypertens 2003 21:1221-28. [Google Scholar]
[33]. Rigó J Jr, Nagy B, Fintor L, Tanyi J, Beke A, Karádi I, Maternal and neonatal outcome of preeclamptic pregnancies: the potential roles of factor V Leiden mutation and 5,10 methylenetetrahydrofolate reductaseHypertens Pregn 2000 19:163-72.10.1081/PRG-10010013210877984 [Google Scholar] [CrossRef] [PubMed]
[34]. Kupferminc MJ, Fait G, Many A, Gordon D, Eldor A, Severe preeclampsia and high frequency of genetic thrombophilic mutationsObstet Gynecol 2000 96:45-49.10.1097/00006250-200007000-0001010862840 [Google Scholar] [CrossRef] [PubMed]
[35]. Dizon-Townson DS, Nelson LM, Easton K, Ward K, The factor V Leiden mutation may predispose women to severe preeclampsiaAm J Obstet Gynecol 1996 175:902-05.10.1016/S0002-9378(96)80022-6 [Google Scholar] [CrossRef]