Caesarean section has greatly evolved over the decades, due to the advent of anaesthesia and good quality antibiotics. Around the world, a rise has been seen in caesarean rates in developed and emerging countries. Currently, 18.6% of all births occur by CS, ranging from 6% to 27.2% in the least and most developed regions, respectively [1]. According to the National Family Health Survey 2015-2016, the rate of c-section in some states is as high as 87.1%, with a yearly rise of 16.7% [2]; which is in contrast to the WHO recommended safe limit of 10-15% of the total number of deliveries in the country. As a result, more women are becoming pregnant with a scar on the uterus. Hence, any problems associated with the presence of a CS scar are potentially significant both for individual patients as well as at a societal level.
There is a consensus American College of Obstetricians and Gynaecologists (ACOG), Royal College of Obstetricians and Gynaecologists (RCOG), National Institute for Health Care and Excellence (NICE) that planned VBAC is a safer choice with a single previous lower segment caesarean delivery for the majority of women [3]. The present author main concern is the choice of patients, who after careful assessment of all factors can be candidates for TOLAC. Of particular interest is the development of protocols to predict performance during TOLAC.
Maternal and neonatal well being is the prime goal and warrants strict labour surveillance. With the advent of 2D, 3D and Doppler imaging and its increasing use in obstetrics and gynaecology, the objectivity of determining the mode of delivery after previous Caesarean Sections (CS) has increased.
There is a need to increase the success of TOLAC to improve the maternal outcome of previous caesarean sections. A successful VBAC would mean lesser blood loss, faster post-partum recovery, less chance of infection etc. There is now a lack of universal predictive model which could be applied to a population for predicting the success of TOLAC. The lacuna in existing knowledge also applies to the lack of objectivity in describing the caesarean scar parameters. There are few studies in literature which analysed the scar using 3D ultrasound. This technology would help us to expand the knowledge of objectively describing a scar and develop a tool which would help in right selection of patients for TOLAC, hence improving it’s success rate.
This study evaluated uterine scar of caesarean section by 2D, 3D ultrasound, Colour Doppler and assess their correlation in determining the mode of delivery among pregnant women with previous caesarean section, and also examine the most accurate ultrasonographic parameter for assessing the quality of scar on the uterus.
Materials and Methods
An observational prospective cohort study was performed in the Department of Obstetrics and Gynaecology at ESI Basaidarapur, New Delhi, during the period of September 2017 to March 2019.
Antenatal patients with previous single lower segment caesarean section were enrolled in the study after written and informed consent and after fulfilling the criteria. The ethical approval letter number is DM (A) H-19/14/17/IEC/2012-PGIMSR.
Previously researchers have performed studies on evaluation of scar parameters to determine the mode of delivery among pregnant women with previous caesarean section. The sensitivity found in these articles ranged between 75-90% [4]. Therefore, assuming p=80% as the sensitivity of scar parameters with a 5% margin of error, the minimum required sample size at 5% level of significance is 245 patients.
Inclusion Criteria
Pregnant women who have previously given birth by caesarean section once with unlimited number of vaginal deliveries, women who have signed the written consent to participate in the study, singleton pregnancies with cephalic presentation, gestational age older than 24-weeks.
Exclusion Criteria
Absolute indications of cesarean section, women who had completed all previous births vaginally, women who had a history of surgery on the uterus for other reasons or a scar of unknown aetiology, fetal macrosomia (≥4 kg), short interconception period (≤18 months), multiple pregnancies, women with bad obstetric history, women older than 40 years, women with uterine anomalies, women who had previous classical scar, uterine tetany/“active phase arrest disorder”.
3D, 2D USG {TOSHIBA Xario 200, linear probe (6-11) MHz, curvilinear probe (3-6) MHz} and Color Doppler were done twice once between (24-28) and once at 36-weeks gestation. The scar parameters were analysed and each parameter was awarded a score, as per the existing scoring system developed by Popov I et al., and finally a total ultrasound score was calculated [Table/Fig-1] [5].
Scoring by Popov I et al., [5].
| Parameter of the scar | Score (1) | Score (2) |
|---|
| Shape | balloon | triangle |
| Continuity | discontinuous | clear |
| Vascularity | hypo | hyper |
| Borders | outside | inside |
| Echo structutre | heterogenous | homogenous |
| Volume in mm3 | <4 | >4 |
| Thickness in mm | >3.5 | <3.5 |
Outcome of labour, whether caesarean or vaginal delivery was monitored and the significance of ultrasound scoring and individual clinical factors were studied.
Statistical Analysis
Statistical testing was conducted with the statistical package for the social science system (SPSS) version 17.0. Continuous variables were presented as mean±SD or median (IQR) for non normally distributed data. Categorical variables were expressed as frequencies and percentages. The Pearson’s chi-square test or the chi-square test was used. A Receiver Operating Characteristics (ROC) analysis was calculated to determine optimal cut-off value of scar parameters. The area under the curve, the sensitivity, and the specificity were also calculated to analyse the diagnostic accuracy of scar parameters correlating with mode of delivery. For all statistical tests, a p-value <0.05 was taken to indicate a significant difference.
Results
Out of 245 patients included in the study, 160 (65.3%) underwent a VBAC and 85 (34.7%) underwent a repeat LSCS. The clinical factors did not show any statistically significant difference, except the onset of labour, spontaneous versus induced, with a p-value of <0.001 [Table/Fig-2,3,4,5 and 6].
Mode of delivery among various age distributions.
| Age groups | Total | Mode of delivery | p-value |
|---|
| VBAC | Repeat LSCS |
|---|
| Frequency (%) | Frequency (%) |
|---|
| 23-25 years | 33 | 17 (51.5%) | 16 (48.5%) | 0.162 |
| 26-30 years | 163 | 108 (66.3%) | 55 (33.7%) |
| 31-35 years | 49 | 35 (71.4%) | 14 (28.6%) |
| Total | 245 | 160 (65.3%) | 85 (34.7%) |
Correlation between parity and mode of delivery.
| Parity | Total | Mode of delivery | p-value |
|---|
| VBAC | Repeat LSCS |
|---|
| Frequency (%) | Frequency (%) |
|---|
| 1 | 205 | 130 (63.4%) | 75 (36.6%) | 0.191 |
| 2 | 30 | 21 (70.0%) | 9 (30.0%) |
| ≥2 | 10 | 9 (90.0%) | 1 (10.0%) |
| Total | 245 | 160 (65.3%) | 85 (34.7%) |
Correlation between interconception period and mode of delivery.
| ICP | Total | Mode of delivery | p-value |
|---|
| VBAC | Repeat LSCS |
|---|
| Frequency (%) | Frequency (%) |
|---|
| 1-4 years | 82 | 51 (62.2%) | 31 (37.8%) | 0.131 |
| 5-6 years | 156 | 102 (65.4%) | 54 (34.6%) |
| 7-8 years | 7 | 7 (100%) | 0 (0.0%) |
| Total | 245 | 160 (65.3%) | 85 (34.7%) |
Correlation between BMI and mode of delivery.
| BMI | Total | Mode of delivery | p-value |
|---|
| VBAC | Repeat LSCS |
|---|
| Frequency (%) | Frequency (%) |
|---|
| ≤25 | 22 | 15 (68.2%) | 7 (31.8%) | 0.766 |
| >25 | 223 | 145 (65.0%) | 78 (35.0%) |
| Total | 245 | 160 (65.3%) | 85 (34.7%) |
Relationship between induced and spontaneous labour and mode of delivery.
| Induced or spontaneous | Total | Mode of delivery | p-value |
|---|
| VBAC | Repeat LSCS |
|---|
| Frequency (%) | Frequency (%) |
|---|
| 1 (spontaneous) | 95 | 78 (82.1%) | 17 (17.9%) | <0.001 |
| 2 (induced) | 150 | 82 (54.7%) | 68 (45.3%) |
| Total | 245 | 160 (65.3%) | 85 (34.7%) |
The ultrasound parameters which showed a statistically significant difference were shape of the scar, thickness of the scar and echostructure of lower uterine segment.
Analysing the shape of the scar by 3D scan, 23 out of 245 patients had a balloon shaped scar on ultrasound, out of which 10 (43.5%) underwent a successful VBAC and 13 (56.5%) underwent a repeat LSCS (p-value 0.021) [Table/Fig-7,8].
Relationship between shape and mode of delivery.
| USG shape | Total | Mode of delivery | p-value |
|---|
| VBAC | Repeat LSCS |
|---|
| Frequency (%) | Frequency (%) |
|---|
| Balloon | 23 | 10 (43.5%) | 13 (56.5%) | 0.021 |
| Triangular | 222 | 150 (67.6%) | 72 (32.4%) |
| Total | 245 | 160 (65.3%) | 85 (34.7%) |
Sensitivity, specificity, PPV, NPV of scar shape.
| Sensitivity | Specificity | PPV | NPV |
|---|
| 67.6% | 57.5% | 93.8% | 15.3% |
The echo structure of lower uterine segment in 24 out of 245 patients had a heterogeneous echo structure. The frequency of VBAC and repeat LSCS in heterogenous LUS was 10 (41.7%) and 14 (58.3%) respectively. In homogenous LUS out of total 221 patients, 150 (67.9%) underwent a VBAC and 71 (32.1%) underwent a repeat LSCS (p-value 0.010). The lower uterine segment dynamics were very important in determining the strength of scar during labour [Table/Fig-9,10].
Echostructure of lower uterine segment.
| Echo structure of LUS | Total | Mode of delivery | p-value |
|---|
| VBAC | Repeat LSCS |
|---|
| Frequency (%) | Frequency (%) |
|---|
| Heterogenous | 24 | 10 (41.7%) | 14 (58.3%) | 0.010 |
| Homogenous | 221 | 150 (67.9%) | 71 (32.1%) |
| Total | 245 | 160 (65.3%) | 85 (34.7%) |
Sensitivity, specificity, PPV, NPV of echostructure.
| Sensitivity | Specificity | PPV | NPV |
|---|
| 67.9% | 58.3% | 93.8% | 16.5% |
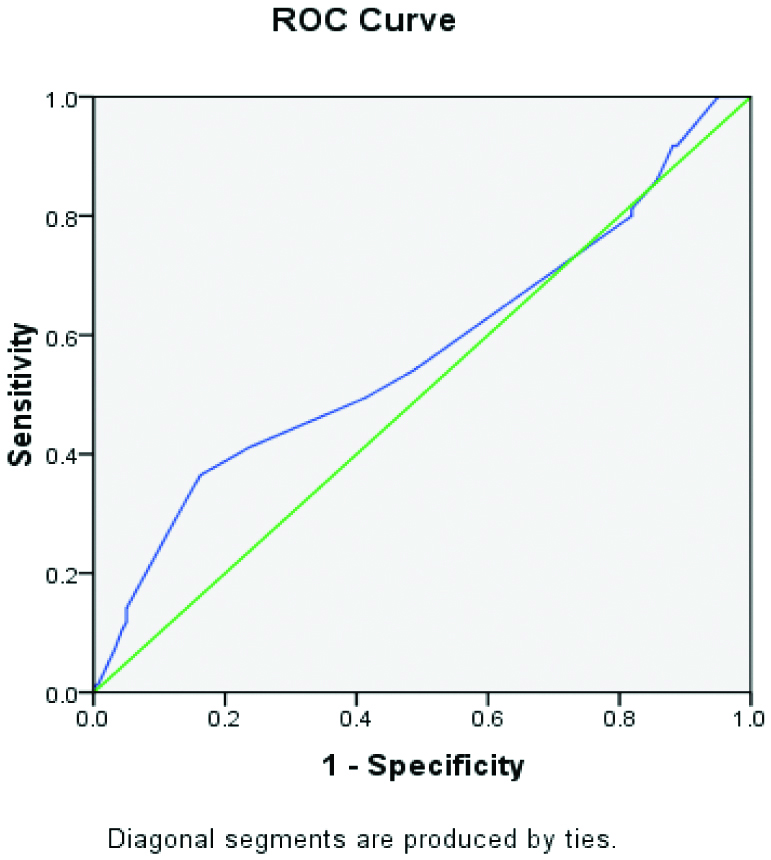
The mean scar thickness obtained in the study at (24-28) weeks for VBAC and repeat LSCS was (2.97±0.37) mm, (2.88±0.40) mm respectively and the scar thickness for VBAC and repeat LSCS at 36-weeks was (2.92±0.35) mm, (2.80±0.41) mm, respectively. The cut off value of scar thickness as generated by the ROC curve was 2.65 mm with area under the curve 0.570 [Table/Fig-11,12 and 13].
Thickness and mode of delivery.
| Thickness 2 | Total | VBAC | p-value |
|---|
| VBAC | Repeat LSCS |
|---|
| Frequency (%) | Frequency (%) |
|---|
| <2.65 | 57 | 26 (45.6%) | 31 (54.4%) | <0.001 |
| ≥2.65 | 188 | 134 (71.3%) | 54 (28.7%) |
| Total | 245 | 160 (65.3%) | 85 (34.7%) |
Sensitivity, specificity, PPV, NPV of scar thickness.
| Sensitivity | Specificity | PPV | NPV |
|---|
| 71.3% | 54.4% | 83.8% | 36.5% |
 |
|---|
| Area under the curve |
|---|
| Area | Std. errora | Asymptotic sig.b | Asymptotic 95% confidence interval |
|---|
| Lower bound | Upper bound |
|---|
| 0.570 | 0.04 | 0.071 | 0.491 | 0.649 |
The parameters like scar shape, borders, continuity, vascularity, volume, echostructure of the lower uterine segment essentially almost remained the same during (24-28) weeks of gestation and 36 weeks of gestation, respectively. It is only in the parameter of scar thickness that a slight variation was observed in the late second trimester and the thickness at term. The cut-off value of total ultrasound score as generated by the ROC curve was 11.5 with AUC 0.562 and p-value 0.016, which only implies that ultrasound scoring system proves to be invaluable in predicting the mode of delivery. The higher the score, the more the chances of successful VBAC [Table/Fig-14,15,16 and 17].
Sensitivity, specificity, PPV, NPV of total ultrasound score.
| Sensitivity | Specificity | PPV | NPV |
|---|
| 67.9% | 55.6% | 92.5% | 17.6% |
Score and mode of delivery.
| Total | Total | VBAC | Repeat LSCS | p-value |
|---|
| Frequency (%) | Frequency (%) | |
|---|
| <11.5 | 27 | 12 (44.4%) | 15 (55.6%) | 0.016 |
| ≥11.5 | 218 | 148 (67.9%) | 70 (32.1%) | |
| Total | 245 | 160 (65.3%) | 85 (34.7%) | |
ROC curve of total ultrasound score.
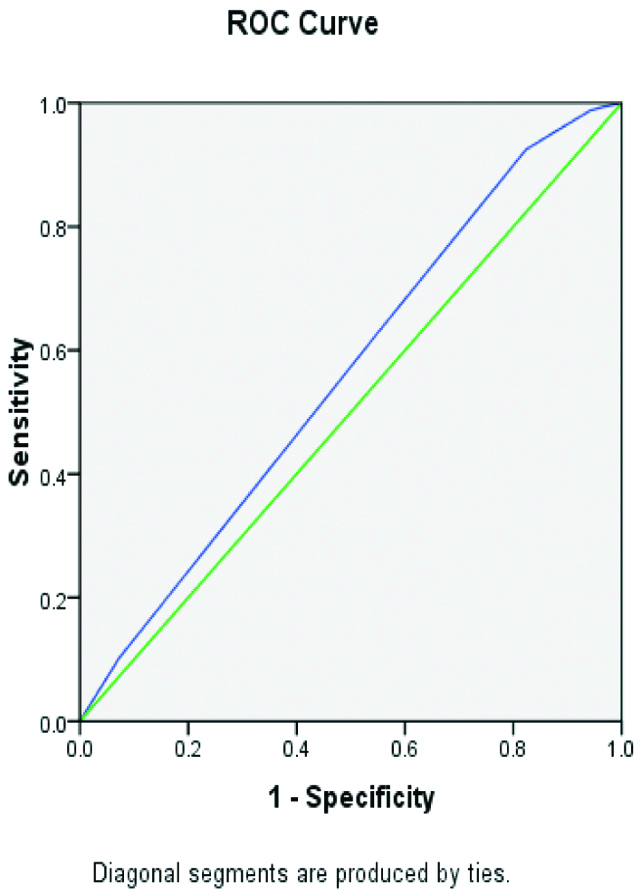 |
|---|
| Area | Std. errora | Asymptotic sig.b | Asymptotic 95% confidence interval |
|---|
| Lower bound | Upper bound |
|---|
| 0.562 | 0.039 | 0.113 | 0.485 | 0.638 |
Intraoperative scar findings.
| INTRA OP SCAR | Repeat LSCS |
|---|
| Frequency | % |
|---|
| Scar dehiscence present | 35 | 41.2% |
| Scar intact | 35 | 41.2% |
| scar thinned out | 15 | 17.6% |
| Total | 85 | 100.0% |
Discussion
Li Y et al., developed a nomogram which helped in predicting the success of VBAC, which became a valuable tool in counselling [6]. The study was a retrospective cohort, factors considered were history of vaginal delivery, gestational age, BMI, estimated birth weight, spontaneous onset of labour and cervical bishop scoring, membrane status. This particular study developed a model for prediction only taking into consideration the clinical parameters. This lacks a certain objectivity which would be conferred by analysing the ultrasound features of the scar [6].
Yang M et al., determined that a prenatal scoring would help in evaluating the success of TOLAC [7]. It was a retrospective study, the indices the authors took into consideration are fetal weight, pre pregnancy BMI, age at delivery, presence of vaginal delivery history, indication of previous caesarean. Three scoring methods were observed and compared in which the above mentioned variables were constant and the differing variable was cervical score in one model, fetal pelvi score in another model and the third model didn’t have either. The maximum area under the curve was for the model incorporating cervical score. Even this study is limiting in terms of lack of ultrasound evaluation of scar.
Gad MS et al., inferred that transvaginal scan was superior to transabdominal scan in measuring the lower uterine segment thickness [8]. The authors compared transabdominal versus transvaginal scan findings of the lower uterine segment thickness to the intra operative scar thickness findings measured with the help of a callipers. The basic advantage of this study is the intraoperative correlation of ultrasound findings. The limitation is that apart from lower segment thickness, other volume based parameters of the scar were not analysed. Also, it did not give any predicting system for TOLAC.
Basic E et al., showed that uterine scar thickness, homogeneity of the scar, scar shape, scar perfusion and scar volume were attributed contributing to the quality of scar which helps in determining the mode of delivery [4]. It’s an observational prospective cohort with a sample size of 108 patients. The authors analysed the various scar parameters, statistical significance was present in scar thickness, shape, homogeneity, volume and vascularity of the scar, this is in contrast to the present study in which only 3 parameters (i.e., shape, echostructure, thickness) were significant.
Nilanchali S et al., inferred that the patients undergoing repeat caesarean section during the trial of TOLAC had a thinner scar than those undergoing successful VBAC [9]. It was a prospective longitudinal study of 168 patients. The mean scar thickness was (4.53±1.21) mm and beyond 36 weeks was (3.02±0.92) mm when measured sonographically between 24 and 28 weeks, while in the present study the mean scar thickness obtained at (24-28) weeks for VBAC and repeat LSCS is (2.97±0.37) mm, (2.88±0.40) mm, respectively and the scar thickness for VBAC and repeat LSCS at 36 weeks is (2.92±0.35) mm, (2.80±0.41) mm, respectively. The success rate of VBAC in this study was 67.6% compared to 65.3% in the present study. The evident difference in the mean values of scar thickness in both the studies is one factor which needs further research. This would require further studies to be carried out and the causal and temporal relations if any like age, race, inter conception period, known co morbidities, technique of caesarean etc., to be analysed. This might help us throw light on the factors involved in the healing of the scar, integrity of the scar and also explain the variation in the mean value of the thickness of the scar obtained in different studies. The limitation in Nilanchali S et al., study is that it took into consideration only one parameter which is scar thickness and also the sample size is only 168 compared to 245 in the present study [9].
Naji O et al., inferred that the inclusion of RMT (Residual Myometrial Thickness) increases the sensitivity of predicting VBAC [10]. A transvaginal sonography to examine scar in 131 pregnant women with previous LSCS was carried out at 11-13, 19-21 and 34-36 weeks’, at each visit according to a defined protocol gestation and prospective measurements of the scar were recorded. The point to be noted here is that there is a significant increase in area under the curve after the inclusion of residual myometrial thickness apart from the scar thickness alone. This only further validates the dynamics of the lower uterine segment on the fate of scar eventually in labour.
Limitation(s)
The study has taken into consideration only the myometrial thickness at the scar site and did not evaluate any other scar factors which is a limitation of the study.
Conclusion(s)
The study infers that 3D ultrasound does play a vital role in selection of patients for TOLAC. The scoring helps in conferring objectivity to the findings. The positive predictive values for the significant scar parameters are high (~93%). This would helps us to counsel the patients for a trial accordingly based on individual scar findings.
Declaration: The abstract of the study is published as it was presented in the FOGSI conference “Breaking silos Across: Adolescence to Menopause” held on 10th-11th August 2019, New Delhi, India.