The Impact of Pre-haemodialysis Systolic Blood Pressure on One-year Survival Rate in Chronic Haemodialysis Patients in Medan, Indonesia
Riri Andri Muzasti1, Mariati Gurning2
1 Assistant Professor in Division of Nephrology and Hypertension, Department of Internal Medicine, Faculty of Medicine, Universitas Sumatera Utara, Medan, North Sumatera, Indonesia.
2 Student, Department of Internal Medicine, Faculty of Medicine, Universitas Sumatera Utara, Medan, North Sumatera, Indonesia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Riri Andri Muzasti, JL DR Mansyur, Medan, North Sumatera, Indonesia.
E-mail: Riri.andri@usu.ac.id
Introduction
Haemodialysis (HD) patients have higher mortality than the general population. Hypertension is frequent in dialysis, but there is no consensus for an optimal target for blood pressure on HD patients. Systolic Blood Pressure (SBP) levels, which are considered “normal” in the general population, are associated with adverse outcomes in HD patients referred to as “reverse epidemiology.”
Aim
To evaluate the impact of pre-haemodialysis Systolic Blood Pressure (pre-SBP) on a one-year survival rate.
Materials and Methods
This was a cohort retrospective study done on 133 HD patients in Adam Malik Hospital in January 2017. The patients were divided into two, based on pre-SBP, <130 mmHg, and ≥130 mmHg for each patient. Demographic data, clinical, and laboratory parameters were collected, and the survival rate observed from January 1st, 2017 until December 31th, 2017.
For the processing of data, SPSS 22.0 was used. A statistical analysis using Kaplan-Meier survival analysis and conventional Cox regression was performed to evaluate one-year survival.
Results
Forty one patients (30.8%) were in category pre-SBP <130 mmHg and 92 patients (69.2%) were in category pre-SBP ≥130 mmHg. One year mortality rate was 25.6%. There was a statistically significant association between pre-SBP <130 mmHg and one-year mortality. After adjusted with age, gender, HD vintage, and Hb, pre-SBP <130 mmHg had greater mortality with Hazard Ratio (HR) 2.235 (CI: 1.110-4.499, p=0.024) compare to pre-SBP ≥130 mmHg.
Conclusion
The relationship between pre-SBP and mortality in HD patients consistently differs from those in the general population. Patients with “low” pre-SBP (<130 mmHg) is associated with greater mortality compared to those with “high” pre-SBP (≥130 mmHg).
Hypertension, Kidney disease, Predictor
Introduction
Patients on maintenance HD run a risk for a higher mortality than the general population or other chronic diseases [1]. The Dialysis Outcomes and Practice Patterns Study (DOPPS) in 2003 reported that one-year mortality rates were 15.6% in Europe and 21.7% in the United States [2]. Cardiovascular disease is the leading cause of death among HD patients [3].
Hypertension is frequent in HD patients with prevalence estimates of up to 90%; also there are no set guidelines on safe BP limits for HD patients [4,5]. The optimal target for BP on HD patients is still controversial. The Kidney Disease Outcomes Quality Initiative (KDOQI) recommendations to achieve a pre-HD SBP <140/90 mmHg and a post-HD SBP <130/80 mmHg but the evidence to support this recommendation is weak [6]. The primary pathogenic mechanism of hypertension in HD patients are volume overload, arterial stiffness, renin-angiotensin-aldosterone system, sympathetic nervous system activity, endothelial cell dysfunction, and erythropoiesis-stimulating agents [7]. In the general population, SBP has an association with the risk of adverse outcomes such as myocardial infarction and stroke linearly [8]. However, the same linear relationships have not been seen in HD patients. Poorer outcome was associated with normal to low BP, while higher BP have more survival advantage [9].
Relationship between mortality and pre-dialysis SBP (pre-SBP) <110 mmHg was associated with increased mortality. It was mentioned in a study by Zager PG et al., in a “U-shaped” curve [10]. Increased mortality associated with SBP <110 mmHg was also found in a study conducted by Maddux DW et al., and Kalantar-Zadeh K et al., [11,12]. Li Z et al., found that SBP <140 mmHg had worse one-year survival than patients with “elevated” SBP >140 mmHg [5]. The “U-shaped” or “reverse J-shaped” curve have been found in various observational studies of End Stage Renal Disease (ESRD) and was associated between BP and mortality, with the highest risk of death at lower predialysis SBP (generally <130 mmHg) and only a slight increase at the highest ranges of SBP (>180 mmHg) [13].
The study was undertaken to evaluate the impact of pre-haemodialysis SBP on a one-year survival rate.
Materials and Methods
The present study was a retrospective cohort study done on 133 HD patients in Adam Malik General Hospital Medan from January 1st 2017 until December 31st 2017. The investigation was approved by the Health Research Ethical Committee of Medical Faculty of Universitas Sumatera Utara (Approval number: LB.02.03/.II.4/1279/2017).
Medical records were reviewed to verify the diagnosis and to obtain all relevant clinical and laboratory data. Inclusion criteria were data for inpatients and outpatients with HD of any aetiology, age >18 years. The pre-SBP level of 130 mmHg was used as cut-off point based on the study of the DOPPS study [2]. Patients with loss of follow-up or lack of medical records were excluded. The survival rate was observed from January 1st, 2017, until December 31th, 2017.
Data from 133 prevalent HD patients who had at least two pre-SBP measurements in different sessions of HD were analysed. Pre-SBP was measured at the start of each HD treatment. The average of two pre-SBP as the value of pre-dialysis SBP was computed. The patients were categorised into two groups of pre-SBP: patients with average pre-SBP <130 mmHg and patients with pre-SBP ≥130 mmHg.
Duration of time between the first day of dialysis treatment and the first day the patients enter the study was defined as dialysis vintage. Two categories of the vintage were formed: (1) one year; (2) more than one year. Two categories of haemoglobin were formed: (1) <9 g/dL; (2) ≥9 g/dL.
Statistical Analysis
All data were analysed with statistical software SPSS 22.0. Bivariate and multivariate analysis was carried out using Kaplan Meier and conventional Cox Regression with the significance level set at p<0.05. Hazard Ratios were estimated using a Cox model for the relationship between pre-SBP categories and mortality and adjusted for potential confounders such as age, sex, HD vintage, and haemoglobin.
Results
In this study 133 HD patients (75 males, 58 females, median age 55 years, range 20-79 years) were analysed. The patients were under HD for 15 (1-58) months. The median of averages pre-dialysis SBP was 140 mmHg. The mean of haemoglobin was 9±1.77 g/dL. [Table/Fig-1] summarises the patients’ main characteristics.
Demographic and clinical characteristics of the patients.
| Variables | n=133 |
|---|
| Gender |
| Male | 75 (56.4%)a |
| Female | 58 (43.6%)a |
| Age median, (years) | 55 (20-79)b |
| Vintage, (month) | 15 (1-58)b |
| Predialysis SBP, mmHg | 140 (100-200)b |
| Haemoglobin (mean±SD), g/dL | 9±1.77b |
| One-year survival rate | 74.4%a |
aCategoric data: n (%); bNumeric data, normal distribution: mean±SD; non normal distribution: median (minimum-maximum)
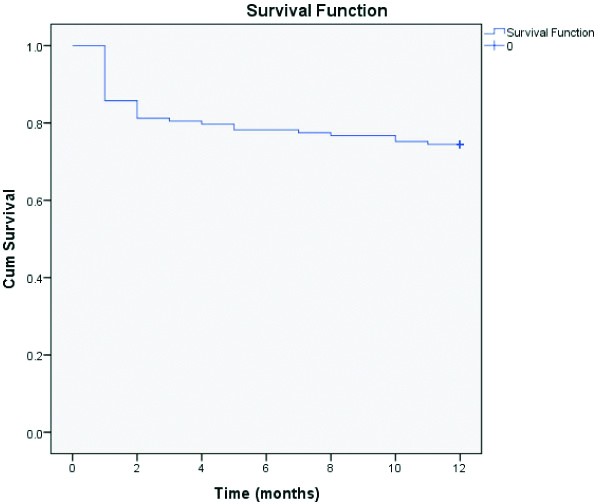
During the follow-up period (12 months), 34 patients died (25.6%). Cumulative survival rates at one year was 74.4%. Median follow-up time was 12 (1-12) months [Table/Fig-2].
One-year cumulative survival of patients over the months.
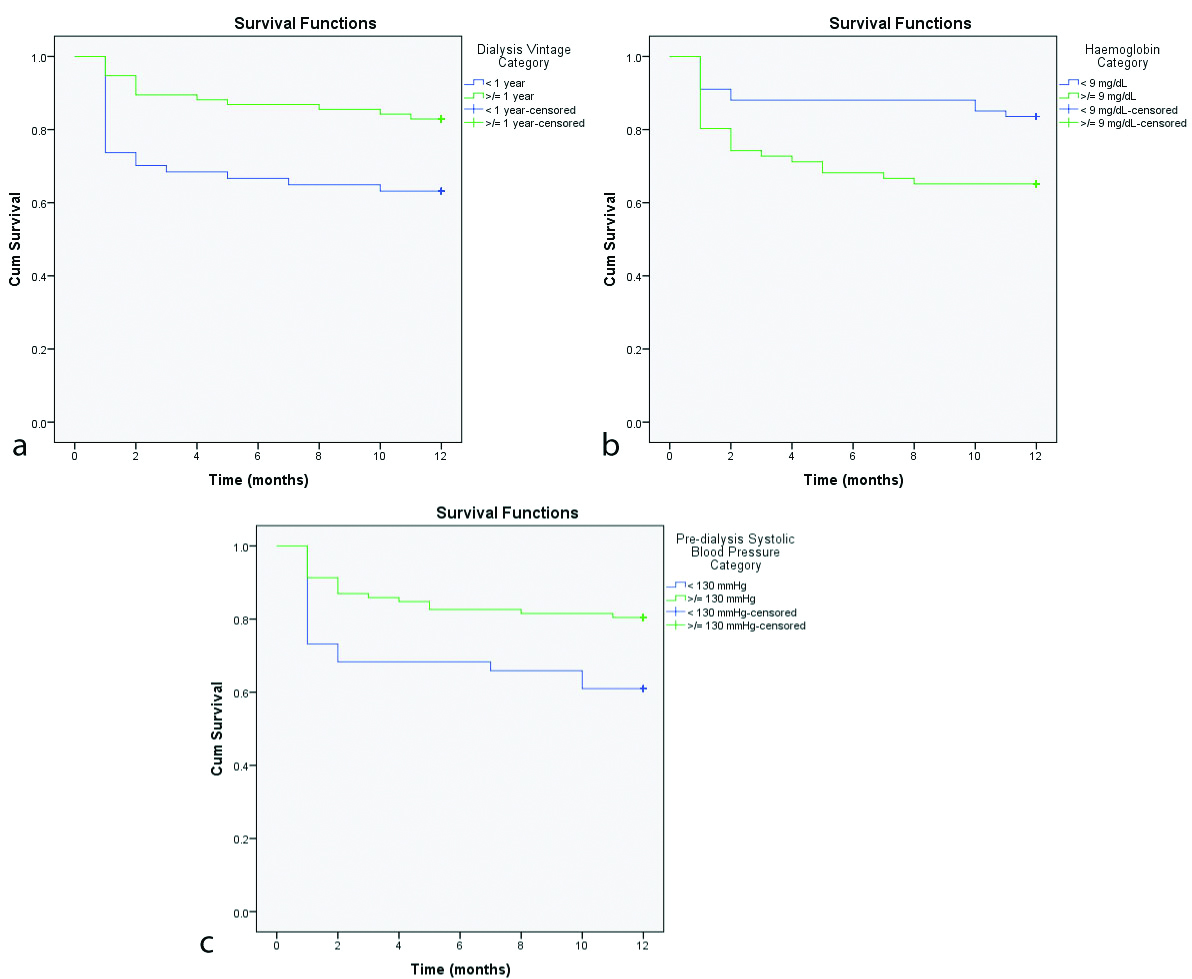
[Table/Fig-3] shows variables associated with poor survival and survival curves are expressed in [Table/Fig-4]. There was a statistically significant difference in mortality between HD patients with pre-SBP category <130 mmHg with mean survival time of 8.3 months compared to patients with pre-SBP category ≥130 mmHg with mean survival time of 10.2 months (p=0.014). There was significant difference in mortality of HD patients with haemoglobin <9 g/dL vs ≥9 g/dL (p=0.014) with mean survival time of 8.6 vs 10.6 months. There was a significant difference in mortality of HD patients with dialysis vintage of <1 year vs 1 ≥ year (p=0.012) with mean survival time of 8.4 vs. 10.6 months. Gender and age had no significant effect on mortality (p=0.0921 and p=0.127, respectively).
| Variable | One year mortality | p-value |
|---|
| Yes | No |
|---|
| Gender | Male | 15 (20%) | 60 (80%) | 0.092 |
| Female | 19 (21.7%) | 39 (79.3%) |
| Age | <40 years | 6 (20.7%) | 23 (79.3%) | 0.127 |
| 40-60 years | 23 (32.4%) | 48 (67.6%) |
| >60 years | 5 (15.2%) | 28 (84.8%) |
| Systolic blood pressure | <130 mmHg | 16 (39 %) | 25 (61%) | 0.014* |
| ≥130 mmHg | 18 (19.6%) | 74 (80.4%) |
| HD Vintage | <1 year | 0 (0%) | 12 (100%) | 0.012* |
| ≥1 year | 16 (37.2%) | 27 (62.8%) |
| Haemoglobin | <9 g/dL | 11 (16.4%) | 56 (83.6%) | 0.014* |
| ≥9 g/dL | 23 (34.8%) | 43 (65.2%) |
*p<0.05 (significant)
Kaplan-Meier curve for cumulative survival over the months according to mortality risk factors. a) HD vintage; b) Haemoglobin; c) Predialysis systolic blood pressure.
[Table/Fig-5] shows the results of multivariate analysis. Pre-SBP category <130 mmHg was found to be associated with a significant Hazard Ratio (HR) 2.235 (CI: 1.11-4.499, p=0.024) after multivariable adjustment for other potential confounders such as haemoglobin, age, gender and HD vintage.
| Variable | B | SE | Wald | Sig. | Exp (B) | 95.0% CI |
|---|
| Lower | Upper |
|---|
| Hb | -0.686 | 0.392 | 3.068 | 0.080 | 0.503 | 0.234 | 1.085 |
| Age | | | 2.398 | 0.301 | | | |
| Age (1) | 0.181 | 0.618 | 0.086 | 0.769 | 1.199 | 0.357 | 4.029 |
| Age (2) | 0.665 | 0.507 | 1.725 | 0.189 | 1.945 | 0.721 | 5.252 |
| Gender | -0.261 | 0.363 | 0.515 | 0.473 | 0.770 | 0.378 | 1.571 |
| Vintage | 0.674 | 0.368 | 3.352 | 0.067 | 1.961 | 0.954 | 4.034 |
| Predialysis SBP | 0.804 | 0.357 | 5.075 | 0.024* | 2.235 | 1.110 | 4.499 |
*p<0.05 (significant)
Discussion
The association of pre-SBP with mortality is complex. The optimal BP target remains unclear. This study evaluated associations of pre-SBP with mortality. This study confirmed that pre-SBP considered normal (<130 mmHg) was associated with higher death risk. Findings were similar to those reported in the literature by Li Z et al., Kalantar-Zadeh K et al., Zager PG et al., and Maddux DW et al., [5,9-11]. This study was unable to explain a reason for this paradoxical finding. There is a possibility that the association between increased mortality and low predialysis BP observed in extensive observational studies is driven by patients who are frail and those with advanced cardiovascular disease [14].
This study found that the prevalence of HD was more frequent in males than in females (56.4%). It is similar to the findings of Muzasti RA and Lubis HR [15], who also found that majority (56.7%) in their study population were males. DOPPS study in 12 countries between 1996-2012 found male vs. female to be 59% vs. 41%. ESRD incidence remains low in reproductive woman, because ESRD often develops in those with Atherosclerosis, Hypertension, Diabetes, and history of CVD as a risk factor [16].
This study found that the one-year mortality rate was 25.6%. It was lower than what Sibarani H et al., found (36.6%) [17]. However, this rate was still higher than in a developed country; in Japan, mortality was only 9.6% in 2009. Screening programs for kidney disease, good management of Chronic Kidney Disease, accessible nephrologist, and excellent dialysis preparation was a reason for a low mortality rate [18]. In Indonesia, characteristics of patients starting dialysis differ with other countries because of differences in the epidemiology of CKD, access to care and quality of medical care for CKD patients, and the acceptance for and timing of initiation of dialysis. Hypertension is the most common aetiology of ESRD in Indonesia. Dialysis in Indonesia was 86% budgeted by a national assurance system that covers HD only two times a week. Patients with dialysis often with severe conditions have high co-morbidity [19,20].
Cut-off HD vintage was one year based on data from the United States Renal Data System (USRDS) that the death rate was highest during first year of initial dialysis [21]. Cut-off haemoglobin that is associated with mortality is still controversial. This study used 9 mg/dL as cut-off. There was a significant association with increased mortality in patients with haemoglobin <9 mg/dL. Toida T et al., also found lower haemoglobin with more significant mortality risk [22].
Limitation(s)
Lack of information on volume status which would help identify patients for whom a low or high BP is a reflection of volume status. Another limitation is absence of data on medication used and cardiac structure or function.
Conclusion(s)
The significant difference was observed between pre-dialysis SBP <130 mmHg compared to patients with pre-dialysis ≥130 mmHg. The study recommends a proper screening for CKD for the detection and treatment of renal dysfunction earlier so it can decrease morbidity and mortality.
aCategoric data: n (%); bNumeric data, normal distribution: mean±SD; non normal distribution: median (minimum-maximum)
*p<0.05 (significant)
*p<0.05 (significant)
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 14, 2019
Manual Googling: Dec 23, 2019
iThenticate Software: Jan 20, 2020 (17%)
[1]. Robinson BM, Tong L, Zhang J, Wolfe RA, Gookin RA, Greenwood RN, Blood pressure levels and mortality risk among hemodialysis patients in the dialysis outcomes and practice patterns studyKidney Int 2012 82:570-80.10.1038/ki.2012.13622718187 [Google Scholar] [CrossRef] [PubMed]
[2]. Foley RN, Hakim RM, Why is the mortality of dialysis patients in the United States much higher than the rest of the world?J Am Soc Nephrol 2009 20(7):1432-35.10.1681/ASN.200903028219443632 [Google Scholar] [CrossRef] [PubMed]
[3]. Weiner DE, Tighiouart H, Amin MG, Stark PC, Macleod B, Griffith JL, Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: A pooled analysis of community-based studiesJ Am Soc Nephrol 2004 15:1307-15.10.1097/01.ASN.0000123691.46138.E215100371 [Google Scholar] [CrossRef] [PubMed]
[4]. Agarwal R, Nissenson AR, Batlle D, Coyne DW, Trout JR, Warnock DG, Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United StatesAm J Med 2003 115:291-97.10.1016/S0002-9343(03)00366-8 [Google Scholar] [CrossRef]
[5]. Li Z, Lacson E Jr, Lowrie EG, Ofsthun NJ, Kuhlmann MK, The epidemiology of systolic blood pressure and death risk in hemodialysis patientsAm J Kidney Dis 2006 48:606-15.10.1053/j.ajkd.2006.07.00516997057 [Google Scholar] [CrossRef] [PubMed]
[6]. KDIGO 2012Clinical practice guideline for the evaluation and management of chronic kidney diseaseKidney International Supplement 2013 3:01-116. [Google Scholar]
[7]. Buren PN, Inrig JK, Hypertension and hemodialysis: pathophysiology and outcomes in adult and pediatric populationsPediatr Nephrol 2012 27(3):339-50.10.1007/s00467-011-1775-321286758 [Google Scholar] [CrossRef] [PubMed]
[8]. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies CollaborationAge-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studiesLancet 2002 360(9349):1903-13.10.1016/S0140-6736(02)11911-8 [Google Scholar] [CrossRef]
[9]. Kalantar-Zadeh K, Kilpatrick RD, McAllister CJ, Greenland S, Kopple JD, Reverse epidemiology of hypertension and cardiovascular death in the hemodialysis populationHypertension 2005 45(2):811-17.10.1161/01.HYP.0000154895.18269.6715699452 [Google Scholar] [CrossRef] [PubMed]
[10]. Zager PG, Nikolic J, Brown RH, “U” curve association of blood pressure and mortality in hemodialysis patients. Medical directors of dialysis Clinic, incKidney Int 1998 54(2):561-69.10.1046/j.1523-1755.1998.00005.x9690224 [Google Scholar] [CrossRef] [PubMed]
[11]. Maddux DW, Usvyat LA, Xu D, Wang Y, Kotanko P, van der Sande FM, The Association of weekly pre-hemodialysis systolic blood pressure and following week mortalityKidney Blood Press Res 2018 43:88-97.10.1159/00048710529414829 [Google Scholar] [CrossRef] [PubMed]
[12]. Kalantar-Zadeh K, Block G, Humphreys MH, Kopple JD, Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patientsKidney Int 2003 63:793-808.10.1046/j.1523-1755.2003.00803.x12631061 [Google Scholar] [CrossRef] [PubMed]
[13]. Chang TI, Systolic blood pressure and mortality in patients on hemodialysisCurr Hypertens Rep 2011 13(5):362-69.10.1007/s11906-011-0223-x21800233 [Google Scholar] [CrossRef] [PubMed]
[14]. Turner JM, Peixoto AJ, Blood pressure targets for hemodialysis patientsKidney International 2017 92:816-23.10.1016/j.kint.2017.01.03828938954 [Google Scholar] [CrossRef] [PubMed]
[15]. Muzasti RA, Lubis HR, Association of phase angle on bioelectrical impedance analysis and dialysis frequency with the survival of chronic hemodialysis patientsEarth and Environmental Science 2018 125:0121110.1088/1755-1315/125/1/012116 [Google Scholar] [CrossRef]
[16]. Iseki K, Gender differences in chronic kidney diseaseKidney International 2008 74:415-17.10.1038/ki.2008.26118670407 [Google Scholar] [CrossRef] [PubMed]
[17]. Sibarani H, Muzasti RA, Lubis HR, Association between neutrophil-to-lymphocyte ratio and survival rate patient hemodialysis in Adam Malik general hospital in 2016Earth and Environmental Science 2018 125:01210810.1088/1755-1315/125/1/012108 [Google Scholar] [CrossRef]
[18]. Robinson B, Zhang J, Morgenstern H, Worldwide, mortality is a high risk soon after initiation of hemodialysisKidney Int 2014 85(1):158-65.10.1038/ki.2013.25223802192 [Google Scholar] [CrossRef] [PubMed]
[19]. Indonesian Renal Registry 2015. https://www.indonesianrenalregistry.org/data/INDONESIAN%20RENAL%20REGISTRY%202015.pdf [Google Scholar]
[20]. Prodjosudjadi W, Suhardjono A, End-stage renal disease in Indonesia: Treatment developmentEthnicity & Disease 2009 19:S1-33-36. [Google Scholar]
[21]. The United States Renal Data System 2015 Annual Data ReportAm J Kidney Dis 2017 69(Suppl1):S391-S404.Available at www.USRDS.ORG/ADR [Google Scholar]
[22]. Toida T, Iwakiri T, Sato Y, Komatsu H, Kitamura K, Fujimoto S, Relationship between hemoglobin levels corrected by interdialytic weight gain and mortality in Japanese hemodialysis patients: Miyazaki dialysis cohort studyPlos One 2017 10.1371/journal.pone.016911728046068 [Google Scholar] [CrossRef] [PubMed]