Introduction
Hospitalisation in the Neonatal Intensive Care Unit (NICU) as a closed chamber, separates neonates from their parents and causes anxiety in the parent’s mind. Nurses can provide a great volume of information in a short period by telenursing.
Aim
To evaluate the effects of telenursing through phone calls on the anxiety levels in parents with neonates, hospitalised in the neonatal intensive care unit.
Materials and Methods
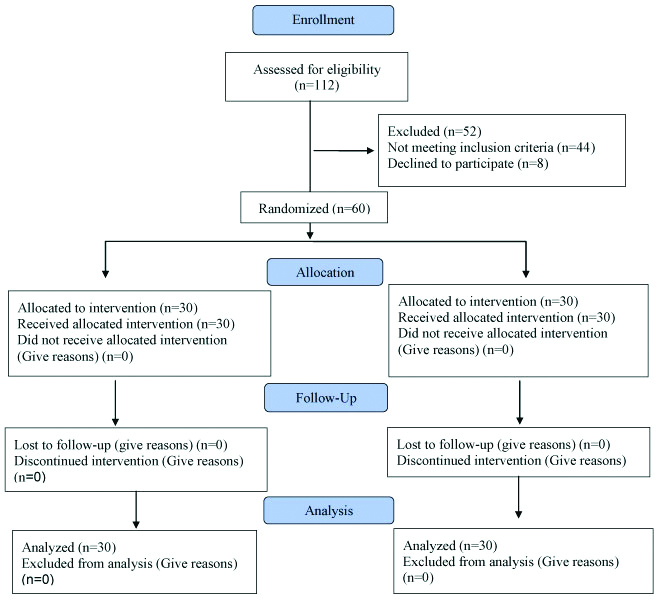
This before-after Quasi-experimental study, with a control group, was conducted from November 2018 to April 2019 among parents of premature neonates admitted in NICU of Mofid Children’s Medical Centre, Tehran, Iran. They were selected through the convenience sampling method, 60 individuals were selected for this research, and they were divided into 30 participants for intervention and control groups. In the intervention group, 15 telephonic conversations between parents and nurses were done totally for 15 days. During these phone contacts, the researcher provided information to one of the parents about the neonate’s respiration, recent vital signs, consciousness level, sleeping rhythm, feeding. The data was collected by using the self-report Beck Anxiety Inventory, and socio-demographics questionnaires. The Beck Anxiety Inventory was filled out once before the intervention and then after phone calls on the first day and fifth, tenth and fifteenth day of admission in the intervention groups. This was also filled out in control groups and were compared in both the groups.
Results
The findings indicated that there was a significant difference in terms of anxiety in the intervention group before (51.80±11.2) and after (25.1±3.4). There was a significant statistical difference between the intervention group and the control group in the fifth, tenth and fifteenth day of hospitalisation (p≤0.001). The anxiety level in the control group before (52.45±11.9) and after (50.43±10.18) intervention showed no significant difference.
Conclusion
The telenursing intervention was effective in reducing anxiety in parents who had their premature neonates in NICU.
Introduction
Neonatal Intensive Care Unit (NICU) dedicated about 10% of hospital beds to themselves. Although since 1995, the number of NICU beds increased about 26% [1,2]. Globally, 13 million neonates are born every year all over the world and about 5-18% of newborns are premature [3,4]. Most of these cases are born in Africa and Asia [5].
According to the World Health Organisation (WHO) report, 3,438 (5.7%) of premature infants are <32 gestational weeks, and the mean days of their hospital stay are 35 days [5,6]. Parents often experience stress, guilt, anxiety, depression, fatigue, sleep disorder, and fear, after the neonate’s admission in NICU [7,8]. Families make decisions for neonates in NICU, and as a result, this responsibility increases their mental pressure [9-11].
Consequently, controlling the anxiety of parents is the priority. Thus, it is essential to consult and help them in the decision-making process [12].
Parents have a remarkable role in improving the patient’s condition. The important fact is that, besides physicians and health personnel endeavours, the decisions, which were made by the parents also affects their infant’s health [9,13]. Due to lack of information about the neonates’ general condition and process of treatment; the decision making process adds in the parents’ anxiety. Parents of neonates in NICU are interested in receiving understandable answers and also being informed about changes in their patients’ clinical conditions [9,14]. By use of telenursing, it is possible to transfer a great volume of information in a short period of time.
Telenursing refers to representing nursing services by the means of applying communication technologies such as telephone, computer, and the internet [12,15]. Among technological devices, Telephone is a traditional one used since past. Due to availability of this technology in almost all patients’ homes, families are able to find answers to many questions they might have in mind, by home calls [13].
As far as searched, there was no previous research in Iran about telenursing on anxiety neonates’ parents during hospitalisation, effect of telenursing on neonates in the NICU. Hence this study aimed to assess the effect of telephone notification by nurses on the parent’s anxiety level, who had a premature neonate in the NICU of Mofid Children’s Hospital affiliated to Shahid Beheshti University of Medical Sciences at Tehran.
Materials and Methods
Study Design and Population
This Quasi-experimental study was conducted in the NICU of Mofid children’s medical centre, Tehran, Iran from November 2018 to April 2019.
The Shahid Beheshti University of Medical Sciences Research Ethics Committee (IR.SBMU.RAM.REC.1394.352) granted ethical approval and the Iranian Registry of Clinical Trial code is IRCT 20190617043912N1. Approximately 129 new newborns are admitted to NICU each year and 30% of them are premature. For the sample size according to previous study, with a confidence level of 95% and test power of 90%, 60 individuals were selected for this research, and they were divided into 30 participants for each group [16].
The randomisation was performed by the central randomisation unit at the Neonatal Health Research Centre, using block randomisation with the same block sizes. All participants were allocated a number. Then the randomisation numbers were given to the head of nursing staff. Thus, she allocated participants to intervention and control groups randomly. All participants provided written informed consent before the data collection; this included permission to use in publications.
Inclusion Criteria
All parents of infants admitted to neonatal intensive care units, have access to the telephone and no hearing or speech problems.
Exclusion Criteria
Parents who showed unwillingness to participate in the study, not able to understand and speak Persian and some who had no access to telephone services.
First, after admission into the NICU, the assistant researcher visited the parents and explained the research objectives. Then an informed consent was attained from the parents in both intervention and control groups, and the demographics form was completed for the parents and neonates.
In 15 consecutive days, the researcher called to the parents (each day, one call) and announced information to family member about recent vital signs of the neonate’s respiration, consciousness level, sleeping rhythm, feeding, and the priority of physical attendance of his/her parents or absence of this necessity. The Beck Anxiety Inventory previously available to family members was filled out one time before intervention, and subsequently after phone contacts in first, fifth, tenth and fifteenth day of their neonates’ admission by self-reporting method. Control group did not received telenursing intervention. Finally, the anxiety level of the participating parents in both the groups was assessed by using the beck anxiety inventory [Table/Fig-1].
Content validity of beck anxiety inventory was assessed and confirmed by 10 nursing academic board members, Shahid Beheshti University of Medical Sciences. For assess reliability, two methods were used: internal reliability and external reliability. To consider internal reliability, α-Cronbach’s index was used and computed 96% in the present study and to consider external reliability identified as re-test method, it was used Interclass Correlation Coefficient (ICC) that obtained 85%.
An informed consent was signed and demographic questionnaire was filled out by the parents, 24 hours after hospitalisation of their neonate in NICU. In order to respect the confidentiality of the participants’ name, phone number of one of parents was recorded. This phone number is in access to researcher and saved as a special code with the recommended name of that member. Researcher has called only by one phone number that previously announced to family member.
All of phone calls were done during 16-16:15 in the evening. At the beginning of each conversation, the parents were asked to repeat parts of the former conversation to ensure that the proper understanding of previous conversation was attained. The average duration time of the conversations was 15 minutes.
The telephone intervention procedure was standardised and also recorded for each parent based on Cox’s Interaction Model of Client Health Behaviour (IMCHB) [17]. It involved a systemic comprehensive assessment of the participant’s requirements, including basic features like the type of participant’s characteristics, the date, time, and nature of the call, as well as a detailed description of the symptoms, problems, or the call reasons. Moreover, all of the present study premature neonates’ required NICU stay for 15 days as recommended by the physicians. Eight of premature neonates’ require NICU more than 15 days. At the end of the intervention, a farewell ceremony was held for the parents and their neonates.
Statistical Analyses
The samples were described by using descriptive statistical methods including the mean and the Standard Deviation (SD). The descriptive statistical method’s findings were calculated based on both qualitative and quantitative data. Shapiro-Wilk test was used in order to determine the normal distribution of the data. Taking into account, the homogeneity of the qualitative factors in two groups, the mean score of the variables were compared between the two groups. This was done by using a parametric t-test, and also Wilcoxon test for non-parametric. Data analyses were performed in SPSS version 21.0 software.
Results
Sixty neonates’ parents were enrolled in this Quasi-experimental study. Minimum, maximum, and average ages of parents were calculated as 20, 39, and 29 years, respectively. Most of the participants were mothers (83.3%), and the majority of them had an education of a high school diploma (43.3%). The majority of neonates were girls, at 83.3% [Table/Fig-2].
Demographic characteristics of premature neonates and their parents in two groups of intervention and control.
| Variable | Intervention N (%) or Mean±SD | Controls N (%) or Mean±SD | p-value |
|---|
| Parent age (year) | 34±3.5 | 36±30 | 0.23 |
| Parent sex | Male | 5 (16.7%) | 3 (10%) | 0.21 |
| Female | 25 (83.3%) | 27 (90%) |
| Parent education level | Illiterate | 0 | 0 | 0.19 |
| Primary school | 0 | 0 |
| High school diploma | 13 (43.3%) | 10 (33.3%) |
| College | 17 (56.7%) | 20 (66.6%) |
| Gestational age (week) | 29±2.5 | 30±1.1 | 0.09 |
| Neonate sex | Male | 5 (16.7%) | 3 (10%) | 0.21 |
| Female | 25 (83.3%) | 27 (90%) |
The [Table/Fig-3] shows the average anxiety scores at different stages of the research. Based on this table, at the beginning of the study (the first day of admission), there was no significant difference between the anxiety scores of the control and intervention groups (p>0.05). In other hands, The comparison mean of anxiety scores in the control and intervention groups in the first, fifth, tenth and fifteenth day of admission showed a significant difference at the level of one percent error between two groups (p<0.001). Also, the p-value for the comparison of the mean total score during the 15 days of admission, which is equal to -8.44, is significant at a 1% error level.
Average of anxiety level of neonates’ parents in the neonatal intensive care unit.
| Mean (SD) | T-test | p-value |
|---|
| Control | Intervention |
|---|
| Before phone intervention | 52.45 (11.9) | 51.80 (11/2) | -0.21 | 0.04 |
| After first day of admission | 49.80 (9.7) | 42.73 (7/1) | -3.22 | 0.002 |
| After fifth day of admission | 51.20 (11.1) | 37.87 (6.3) | -6.74 | ≤0.001 |
| After tenth day of admission | 50.21 (10.8) | 36.46 (4/5) | -7.71 | ≤0.001 |
| After fifteenth day of admission | 49.50 (7.4) | 33.27 (5.3) | -16.41 | ≤0.001 |
| End of intervention (average first, fifth, tenth and fifteenth day of admission) | 50.43 (10.18) | 25.1 (3.4) | -8.44 | ≤0.001 |
According to the results of the Wilcoxon test in [Table/Fig-3], showed that daily conversations effectively reduced anxiety at 1% error level (p≤0.001) [Table/Fig-4].
Comparison of averages of anxiety level of neonates’ parents between the intervention and control groups.
| Time | Wilcoxon test | p-value |
|---|
| Before phone intervention and after first day of admission | -4.54 | ≤0.001 |
| Before phone intervention and after fifth day of admission | -4.72 | ≤0.001 |
| Before phone intervention and after tenth day of admission | -4.56 | ≤0.001 |
| Before phone intervention and after fifteenth day of admission | -4.36 | ≤0.001 |
Discussion
The results of comparing the mean scores of parents’ anxiety levels between the intervention and control groups indicated that telenursing made a significant statistical difference in the intervention group.
Findings of a study showed that the effectiveness of active telephone support on breastfeeding premature infants in Sweden in 2013. They concluded that telenursing improved breastfeeding, maternal satisfaction, mother and infant attachment, and also alleviated maternal anxiety [18]. In another study, the effect of phone intervention by nurses on the mood and anxiety level of patients with implantable cardioverter defibrillators and their caregivers was assessed. They stated that eight weeks of telephone follow-up decreased the anxiety level considerably [19]. Also, a study was concluded that telenursing had a positive-effect on increasing attachment and mitigating the level of stress in mothers with premature infants [7].
Results of a study established that telenursing via the Internet was more effective and has fewer costs than the conventional hospital-based follow-up [17]. A study showed that telemedicine reduces care costs and enhances emotional support during and after hospitalisation [20].
Another study described a significant statistical relationship between informing families about patients’ conditions and reducing their anxiety level after phone intervention [13]. Telenursing can be effective as a treatment plan for accelerating recovery after coronary artery bypass grafting [21].
In the present study, the mean score of primary anxiety before phone calls in the intervention group and in the control group was 51/80±11/2 and 52.45±11.9, respectively. However, after intervention, score of anxiety improved in intervention group. This finding of the present study is to coordinate with above studies. It seems that resolving information’ gap in patient’s families by use of telenursing can improve their anxiety level.
Limitation(s)
Use of Beck Anxiety Inventory is a limitation due to its probable bias during self-reporting. Also, the different cultural context of participants in phone conversations can be effective in intervention output.
Conclusion(s)
The telenursing intervention was effective in reducing anxiety in parents who had their premature neonates in NICU for 15 days. Given the easy access to a telephone for almost all parents and its simple use, including this technology in the educational and care context of neonatal parents is recommended. Also, using this technology requires establishing remote communication methods courses in educational programs of nurses. In its context, this research provides the ground for further studies and technology introduction to the nursing field. In addition to that, the technology can be used in planning in order to cut and minimise the costs, caused by temporal and spatial limitations.
[1]. Halpern NA, Pastores SM, Critical care medicine in the United States 2000-05: An analysis of bed numbers, occupancy rates, payer mix, and costsCrit Care Med 2010 38(1):65-71.10.1097/CCM.0b013e3181b090d019730257 [Google Scholar] [CrossRef] [PubMed]
[2]. Freedman S, Capacity and utilization in health care: The effect of empty beds on neonatal intensive care admissionAm Econ J: Econ Policy 2016 8(2):154-85.10.1257/pol.2012039327942353 [Google Scholar] [CrossRef] [PubMed]
[3]. Reihani T, Sekhavat Poor Z, Heidarzadeh M, Mosavi SM, Mazlom SR, The effect of spiritual self-care training on feeling of comfort in mothers of hospitalized preterm infantsJournal of Midwifery And Reproductive Health 2014 2(2):112-19. [Google Scholar]
[4]. WHO. What is a preterm baby? Geneva: World Health Organization. 2017 [Google Scholar]
[5]. Axelin A, Parents as pain killers in the pain management of preterm infants 2010 MS. University of Turku [Google Scholar]
[6]. Villanueva ELA, Gutiérrez AKC, Pichardo CM, Lucio JR, Epidemiological profile of premature laborGinecol Obstet Mex 2008 76(09):542-48. [Google Scholar]
[7]. Jafarzadeh ZA, Maghsoudi J, Barekatain B, Marofi M, Effect of telenursing on attachment and stress in mothers of preterm infantsIranian Journal of Neonatology IJN 2019 10(1):65-71. [Google Scholar]
[8]. Busse M, Stromgren K, Thorngate L, Thomas KA, Parents’ responses to stress in the neonatal intensive care unitCrit Care Nurse 2013 33(4):52-59.10.4037/ccn201371523908169 [Google Scholar] [CrossRef] [PubMed]
[9]. Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Berns SD, Family support and family-centreed care in the neonatal intensive care unit: Origins, advances, impactSemin in Perinatol 2011 35(1):20-28.10.1053/j.semperi.2010.10.00421255703 [Google Scholar] [CrossRef] [PubMed]
[10]. Eden LM, Callister LC, Parent involvement in end-of-life care and decision making in the newborn intensive care unit: An integrative reviewJ Perinat Educ 2010 19(1):29-39.10.1624/105812410X48154621197127 [Google Scholar] [CrossRef] [PubMed]
[11]. Shorofi SA, Jannati Y, Roohi Moghaddam H, The psychosocial needs of the families of the patients admitted to intensive care units: A review of literatureClin Exc 2014 3(1):46-57. [Google Scholar]
[12]. Moore T, Woodrow P, High dependency nursing care: observation, intervention and support for level 2 patients: Routledge 2009 Jun 4 LondonRoutledge Taylor & Fransis:29610.4324/9780203875889 [Google Scholar] [CrossRef]
[13]. Chien WT, Chiu YL, Lam LW, Ip WY, Effects of a needs-based education programme for family carers with a relative in an intensive care unit: A quasi-experimental studyInt J Nurs Stud 2006 43(1):39-50.10.1016/j.ijnurstu.2005.01.00616183062 [Google Scholar] [CrossRef] [PubMed]
[14]. Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E, Clinical practice guidelines for support of the family in the patient-centreed intensive care unit: American College of Critical Care Medicine Task Force 2004-2005Crit Care Med 2007 35(2):605-22.10.1097/01.CCM.0000254067.14607.EB17205007 [Google Scholar] [CrossRef] [PubMed]
[15]. Hall SL, Cross J, Selix NW, Patterson C, Segre L, Chuffo-Siewert R, Recommendations for enhancing psychosocial support of NICU parents through staff education and supportJ Perinat 2015 35(S1):S29-36.10.1038/jp.2015.14726597803 [Google Scholar] [CrossRef] [PubMed]
[16]. Abdeyazdan Z, Shahkolahi Z, Mehrabi T, Hajiheidari M, A family support intervention to reduce stress among parents of preterm infants in neonatal intensive care unitIran J Nurs Midwifery Res 2014 19(4):349-53. [Google Scholar]
[17]. Isetta V, Lopez-Agustina C, Lopez-Bernal E, Amat M, Vila M, Valls C, Cost-effectiveness of a new internet-based monitoring tool for neonatal post-discharge home careJ Med Internet Res 2013 15(2):e3810.2196/jmir.236123419609 [Google Scholar] [CrossRef] [PubMed]
[18]. Ericson J, Eriksson M, Hellström-Westas L, Hagberg L, Hoddinott P, Flacking R, The effectiveness of proactive telephone support provided to breastfeeding mothers of preterm infants: study protocol for a randomized controlled trialBMC Pediatr 2013 13(1):7310.1186/1471-2431-13-7323663521 [Google Scholar] [CrossRef] [PubMed]
[19]. Sneed NV, Finch NJ, Michel Y, The effect of psychosocial nursing intervention on the mood state of patients with implantable cardioverter defibrillators and their caregiversProgress in Cardiovascular Nursing 1997 12(2):04-14. [Google Scholar]
[20]. Gray JE, Safran C, Davis RB, Pompilio-Weitzner G, Stewart JE, Zaccagnini L, Baby CareLink: using the internet and telemedicine to improve care for high-risk infantsPediatrics 2000 106(6):1318-24.10.1542/peds.106.6.131811099583 [Google Scholar] [CrossRef] [PubMed]
[21]. Bikmoradi A, Masmouei B, Ghomeisi M, Roshanaei G, Impact of Tele-nursing on adherence to treatment plan in discharged patients after coronary artery bypass graft surgery: A quasi-experimental study in IranInt J Med Inform 2016 86:43-48.10.1016/j.ijmedinf.2015.12.00126725694 [Google Scholar] [CrossRef] [PubMed]