The depression and anxiety are the most recognised adverse events after a cerebro vascular accident [1,2]. Recent systematic reviews and trails from India states that 33% of all stroke survivors experience symptoms of depression and 18% experience anxiety [3-5]. Stroke survivors with depression and anxiety have decreased functional recovery, psychosocial outcome, quality of life and higher death rates and hence greater the length of hospital stay [6-13]. Early and frequent mobilisation is one of the significant parts of acute stroke care units. ‘Very Early Mobilisation’ is defined as frequent out of bed activities of daily living initiated within the first 24 hours of symptom onset [14].
Recent evidence suggests that early and repetitive out of bed activities after acute stroke are proven to be safe, feasible [15] and cost effective [16]. Further very early mobilisation is effective in improving the functional status [17,18], health-related quality of life [19] and reduce the number and severity of adverse events, length of hospital stay [20]. However, recent trials have shown that, very early mobilisation has no effect on depression further had a negative effect on functional disability [21,22]. So, the aim of present study was to determine the effect of very early mobilisation in addition to standard care compared with standard care alone on symptoms of depression and anxiety following acute stroke.
Materials and Methods
This study was a parallel active-controlled, single blinded randomised controlled trial, Registered with Clinical trial registration of India (CTRI/2016/04/006795). Ethical approval was granted by the central ethical committee of the Nitte deemed to be University (ref: NU/CEC/Ph.D-52/2012). Informed written consent was obtained from all the participants or their caregivers at the start of the study. Subjects were recruited from the stroke population group satisfying the inclusion criteria from the Department of Medicine and Neurology of KS Hegde Charitable hospital, Deralakatte, Mangaluru, Karnataka, India, from December 2013 to December 2015. An informal pilot randomised controlled study was conducted among 30 subjects prior to the actual study. Between groups mean difference (2.16) and pooled standard deviation (3.98) of HAD- Depression scale change scores (admission-discharge) were obtained. The standardised difference obtained was 0.5427. A total of 53 subjects were needed for each group with a two-sided significance of 0.05 (alpha 5%) and a power of 0.8 (beta 20%) [23].
Inclusion Criteria
Stroke patients with age above 18 years and of either gender and who was admitted within 24 hours of onset of symptoms, were able to comprehend and respond verbally, systolic BP between 120 and 180 mm Hg, an O2 saturation >92% (with or without supplementation), a pulse rate between 40 and 100 beats per minute, and within normal range of body temperature <38.5°C, Subjects were included in the study after attaining concerned medical professional permission [24].
Exclusion Criteria
Worsened within the first hour of admission to the hospital and intensive care unit, and altered sensorium. Subjects with premorbid modified Rankin Scale [25] (mRS) Score >3, modified rankin scale is a measure of disability, it is a 6 point rating scale, where ‘0’ indicates No symptoms and ‘5’ indicates Severe disability, transient ischemic attacks, concurrent progressive neurological disorder, unstable coronary condition (e.g., acute myocardial infarction) or other medical condition that would impose hazard to the subjects, or if their physiological variables (blood pressure, oxygen, heart rate, temperature) fall outside set safety limits, severe heart failure, lower limb fracture preventing mobilisation, palliative care subjects.
Subjects were randomly allotted to one of two groups (Group A, Group B) using a computer-generated random sequence method, allocation concealment done by using a sequentially numbered opaque and sealed envelope method. Implementation was done by a person, who was not related to the study, enrolled the participants and allocated them to groups based on numbers found in the envelope.
Group A: The intervention group received the standard care and in addition, out of bed activities was initiated as soon as possible after enrollment, aiming to have first mobilisation within 24 hours of the onset of the stroke symptoms. Time spent on early and out of bed activities was determined by the individual tolerance (5-30 minutes), participants obtained out of bed activities minimum two times per day for seven days or until the discharge.
Individuals in this group received out of bed activities such as sit at the edge of the couch, sitting unsupported out of bed, transfer with assistance, roll and sit up, sitting upright without support, transfer feet on the floor, stand upright with or without support, walk-early gait, advanced gait activities [15,18].
Vital signs were measured before each mobilisation within the first three days of cerebrovascular accident. If there were any abnormalities like blood pressure drop of >30 mm Hg during mobilisation, it was discontinued. Intervention was provided face to face individually by a neuro physiotherapist and intervention was delivered at Inpatient Department of Medicine and Neurology at Justice KS Hegde Charitable Hospital, Deralakatte, Mangaluru, Karnataka, India.
Group B: Participants in the standard care group, received the correct positioning in bed, passive and active (if possible) mobilisation, mobilisation in bed, sitting balance activities, facilitation of limb and trunk control activities, education of individual with stroke and caregiver [26]. Each group received the standard care treatment within 48 hours following a stroke, for 45 minutes a day, for seven days or until the discharge.
Outcome Measures
HADS: It has excellent reliability, good validity and sensitive to change screening tool that measures anxiety and depression in stroke individuals. Administration time ranges from 2-5 minutes [27-29].
HADS is 14 items, self-reported questionnaire that examine the subjects to reflect on their mood in the past week. Scores for items in each subscale of the HADS are summed to produce an anxiety score (HADS-A) or a depression score (HADS-D). It has 4-point Likert scale (ranging from 0=symptom absent, to 3=symptom present), for a total score ranging from 0-21 for each subscale [27,28]. Interpretation of scores: 0-7 for normal, 8-10 for mild distress, 11-14 for moderate distress, and 15-21 for severe distress [29]. Initially, licensed HADS questionnaire in the regional language (Kannada and Malayalam) and in Indian, English was procured from GL Assessment, UK. Reliability of Kannada and Malayalam version of HADS Questionnaire was performed and the Cronbach’s alpha value obtained for the scale was 0.73 and 0.75, respectively. HADS Questionnaire was administered at admission, seven days or discharge (whichever was earlier) and three months follow-up after cerebrovascular accident and measurements were taken by the researcher who had been blinded to the group allocation.
Statistical Analysis
The data management and analysis were performed by using Microsoft Excel and SPSS for windows, version 16.0. Chicago, USA, SPSS Inc. Demographic data and outcome measures were analysed by using mean, median, standard deviation, interquartile ranges, frequency, and percentage. Possible differences in baseline demographic characteristics between groups were analysed by using Independent t-tests for continuous measurement and Chi-square (χ2) test of independence for categorical measurement. Nonparametric statistical tests such as the Wilcoxon sign rank test was used to compare within-group and the Mann-Whitney U-test was used to compare the outcome measures between groups. The p-value <0.05 was considered as significant. The effect size and power analysis for the HADS was performed using the G Power software version 3, the effect size values were divided into “small” (≥0.2 to <0.5), “medium” (≥0.5 to <0.8), and “large” (≥0.8) [30].
Results
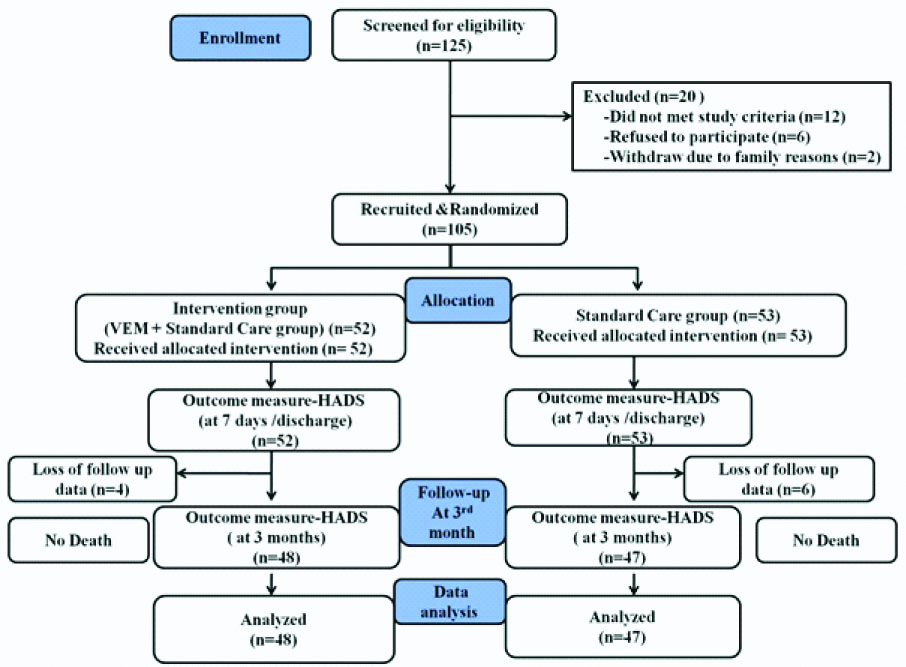
A total of 125 stroke subjects were assessed. Demographic and clinical characteristics are showed in [Table/Fig-1]. Total 105 subjects were recruited and randomised to 52 subjects allocated to the intervention group and 53 subjects allocated to the standard care group. Most of the characteristics were homogenous between groups. No death was reported in both the groups and there were 10 dropouts and they were excluded in the final analysis consort flowchart is shown in [Table/Fig-2].
Baseline demographic and clinical characteristics of recruited subjects.
| Variables | Intervention group (n=48) Number (%) | Standard care group (n=47) Number (%) | Total n=95 Number (%) | p-value |
|---|
| Age (Years) | 0.059a |
| Mean (SD) | 59.08 (10.83) | 63.02 (9.14) | 61.03 (10.17) |
| <56 | 18 (37.5) | 10 (21.3) | 28 (29.5) | 0.002b |
| 56-65 | 16 (33.3) | 20 (42.6) | 36 (37.9) |
| 66-75 | 10 (20.8) | 10 (21.3) | 20 (21.1) |
| >75 | 4 (8.3) | 7 (14.9) | 11 (11.6) |
| Sex | 0.003b |
| Male | 31 (64.6) | 31 (66) | 62 (65.3) |
| Female | 17 (35.4) | 16 (34) | 33 (34.7) |
| Side affected | 0.259b |
| Right | 30 (62.5) | 23 (48.9) | 53 (55.8) |
| Left | 18 (37.5) | 24 (51.1) | 42 (44.2) |
| Type of stroke | | | | <0.001b |
| Thrombotic | 37 (77.1) | 39 (83) | 76 (80) |
| Embolic | 5 (10.4) | 4 (8.5) | 9 (9.5) |
| Hemorrhage | 6 (12.5) | 4 (8.5) | 10 (10.5) |
| Stroke risk factors | |
| Hypertension | 29 (60.4) | 25 (53.2) | 54 (56.8) | 0.182b |
| Diabetes mellitus | 30 (62.5) | 23 (48.9) | 53 (55.8) | 0.259b |
| Cardiovascular disease (CVD) | 12 (25) | 15 (31.9) | 27 (28.4) | <0.001b |
| Smoking | 17 (35.4) | 15 (31.9) | 32 (33.7) | <0.001b |
| Alcoholics | 10 (20.8) | 12 (25.5) | 22 (23.2) | <0.001b |
| Severity (NIHSS) | 0.918b |
| Mild (0-7) | 26 (54.2) | 21 (44.7) | 47 (49.5) |
| Moderate (8-16) | 22 (45) | 26 (55.3) | 48 (50.5) |
| Length of hospital stay | 0.002a |
| Mean (SD) in days | 9.02 (3.05) | 11.38 (3.94) | 10.18 (3.69) |
SD: Standard deviation; NIHSS: National institutes of health stroke scale; a: Analysed by Independent Student’s t-test; b: Analysed by Chi-Square test
Change scores (at admission- at discharge) in HADS-Anxiety scores were higher for the intervention group (median=4.5, inter quartile range=2.25-7.75) than the standard care group (median=1, inter quartile range=0.2-5) and change scores (three months follow-up at admission) in HADS-Anxiety scores were higher for the intervention group (median=5, inter quartile range=3-7) than the standard care group (median=1, inter quartile range=0-5). Mann-Whitney U test results showed that improvement in HADS Anxiety scores were statistically significant (p<0.05) [Table/Fig-3].
Between-group comparisons of Hospital Anxiety Depression Rating Scale (HADS)- Anxiety Score on admission, at discharge and at three months follow-up in individuals with acute stroke.
| HADS-anxiety score (0-21) | Intervention group** n=48 | Standard care group*** n=47 | 95% CI of difference | Mean difference | U-value | Between-group p-value* | Power | Effect size |
|---|
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | Upper | Lower |
|---|
| On admission | 12.91 (3.41) | 12 (10-16) | 11.93 (2.88) | 11 (10-15) | -0.30 | 2.27 | 0.98 | 950 | >0.005 | 0.030 | 0.30 |
| At discharge | 7.87 (2.38) | 8 (6-10) | 10.25 (3.69) | 11 (8-12) | -3.64 | -1.11 | -2.38 | 537 | <0.001 | 0.61 | 0.76 |
| At 3rd month follow-up | 7.54 (2.28) | 8 (6-10) | 9.51 (3.23) | 9 (8-11) | -3.10 | -0.82 | -1.96 | 459 | <0.001 | 0.50 | 0.70 |
| Change score (Admission-Discharge) | 5.04 (3.02) | 4.5 (2.25-7.75) | 3.12 (2.65) | 1 (0.2-5) | 1.67 | 3.04 | 3.36 | 642.5 | <0.001 | 0.29 | 0.58 |
| Change score (Admission-3rd month follow-up) | 5.37 (3.23) | 5 (3-7) | 2.78 (3.83) | 1 (0-5) | 1.38 | 4.51 | 2.94 | 648.5 | <0.001 | 0.56 | 0.73 |
Intervention group: Very early mobilisation+standard care; SD: Standard deviation; IQR: Inter quartile range; CI=Confidence interval; *Mann-Whitney U-test p-value: <0.05; **Wilcoxon sign rank test p-value: <0.05; ***Wilcoxon sign rank test p-value: <0.05
Scores change (at admission- at discharge) in HADS-Depression scores were higher for the intervention group (median=5, inter quartile range=4-7) than the standard care group (median=2, inter quartile range=1-5) and scores change (three months follow-up at admission) in HADS-Depression scores were higher for the intervention group (median=7, inter quartile range=3.25-8.75) than the standard care group (median=2, inter quartile range=1-5). Mann-Whitney U test results showed that improvement in HADS Depression scores were statistically significant (p<0.001) [Table/Fig-4].
Between-group comparisons of Hospital Anxiety Depression Rating Scale (HADS)-Depression Score on admission, at discharge and at three months follow-up in individuals with acute stroke.
| HADS depression score (0-21) | Intervention group** n=48 | Standard care group*** n=47 | 95% CI of difference | Mean difference | U-value | Between group p-value* | Power | Effect size |
|---|
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | Upper | Lower |
|---|
| On admission | 12.18 (3.16) | 12.5 (9-14) | 12.97 (2.58) | 14 (11-15) | -1.97 | .38 | -0.79 | 950 | >0.005 | 0.01 | 0.26 |
| At discharge | 6.77 (2.65) | 6 (5-8.75) | 9.85 (3.39) | 11 (8-12) | -4.32 | -1.83 | -3.08 | 537 | <0.001 | 0.91 | 0.99 |
| At 3rd month follow-up | 6.60 (2.55) | 7 (4.25-8) | 10.19 (3.56) | 12 (8-13) | -4.84 | -2.32 | -3.58 | 459 | <0.001 | 0.91 | 0.99 |
| Change score (Admission- discharge) | 5.41 (3.14) | 5 (4-7) | 3.12 (2.65) | 2 (1-5) | 1.10 | 3.47 | 2.28 | 634.50 | <0.001 | 0.89 | 0.96 |
| Change score (Admission-3rd month follow-up) | 5.58 (4.08) | 7 (3.25-8.75) | 2.78 (3.83) | 2 (1-5) | 1.18 | 4.41 | 2.79 | 677 | <0.001 | 0.90 | 0.97 |
Intervention group: Very early mobilisation+ Standard care, SD: Standard deviation, IQR: Inter quartile range, CI: Confidence interval; * Mann-Whitney U-test p-value: <0.05;** Wilcoxon sign rank test p-value: <0.05; *** Wilcoxon sign rank test p-value: <0.05
Moderate symptoms of anxiety levels with the intervention group, on admission were reported by 58.3% of patients with the acute stroke and whereas at discharge and follow-up, only 4.25% and 12.5% of patients with acute stroke reported moderate symptoms of stroke. In Intervention group, approximately 66.7% reported moderate symptoms of depression at admission and only 6.3% reported at discharge and follow-up. In Standard care group, approximately 80.9% reported moderate symptoms of depression at admission and approximately 51.1% reported at discharge [Table/Fig-5].
Categorised HADS distribution of subjects with symptoms of anxiety and depression on admission, at discharge and at three months follow-up in individuals with acute stroke.
| HADS categorised | Admission | Discharge | Follow-up |
|---|
| Intervention group (n=48) n (%) | Standard care group (n=47) n (%) | Intervention group (n=48) n (%) | Standard care group (n=47) n (%) | Intervention group (n=48) n (%) | Standard care group (n=47) n (%) |
|---|
| Anxiety |
| Normal (0-7) | 0 (0) | 1 (2.1) | 21 (43.8) | 14 (29.8) | 23 (47.9) | 10 (21.3) |
| Mild (8-10) | 20 (41.7) | 22 (46.8) | 25 (52.1) | 5 (10.6) | 19 (39.6) | 24 (51.1) |
| Moderate (11-14) | 28 (58.3) | 24 (51.1) | 2 (4.2) | 28 (59.6) | 6 (12.5) | 13 (27.7) |
| p-value* | 0.498 | 0.001 | 0.016 |
| Depression |
| Normal (0-7) | 3 (6.3) | 0 (0) | 26 (54.2) | 10 (21.3) | 26 (54.2) | 10 (21.3) |
| Mild (8-10) | 13 (27.1) | 9 (19.1) | 19 (39.6) | 13 (27.7) | 19 (39.6) | 9 (19.1) |
| Moderate (11-14) | 32 (66.7) | 38 (80.9) | 3 (6.3) | 24 (51.1) | 3 (6.3) | 28 (59.6) |
| p-value* | 0.121 | 0.001 | 0.001 |
*Analysed by Chi-square test, p>0.05 indicates association between groups; Intervention group: Very early mobilisation+standard care
Discussion
The results of this randomised controlled trial showed that early and frequent out of bed activities coupled with the standard care reduced the levels of depression and anxiety (p<0.05) compared with the standard care alone following acute stroke. Therefore, we accepted experimental hypothesis. The results of the current study repute with the randomised controlled trial conducted by Cumming TB et al., found that very early mobilisation group, 47% (17 of 36) of the stroke survivors had no significance difference effect on the Hospital anxiety and depression scale anxiety score at seven days or at discharge compared with 40% 13/32) of the standard care (p=0.385), hospital anxiety and depression scale depression score at seven days or at discharge compared with 28% (9/32) of the standard care (p=0.012) [22]. However, no significant differences the same at three months and one year after stroke. The current randomised controlled trial is different from the Cumming TB et al., who performed a multi-centre, randomised controlled trial on 71 subjects with acute stroke [22]. Irritability, Depression, Anxiety rating scale (IDA) was used to measure depression and anxiety on admission, discharge (7th day), three months, and one year follow-up. Present study was a single centre, randomised control trial which recruited 105 subjects with acute stroke. Anxiety and depression with a HADS at admission, discharge (seven days) and three months follow-up were measured.
Aidar FJ et al., investigated the effects of aquatic physical activity on depression and anxiety on 30 individuals with ischemic stroke [31]. Their results demonstrated that aquatic exercises significantly improved the levels of depression and anxiety (p<0.05) in ischemic stroke survivors. These results are similar to the results in the present study. Eng JJ et al., performed meta-analysis on the effect of structured exercise on depression symptoms in sub-acute and chronic cerebrovascular accident patients, and their results states that exercises are possible treatment to alleviate and reduce symptoms of depression in sub-acute and chronic stroke patients [32]. These results are consistent with the findings in the present study. Potential explanations for the reduction in depression and anxiety could be attributed firstly to the early and repetitive out of bed physical activity prevents the development of immobility-related adverse events and hence reduced length of hospital stay. Secondly, additional care and time spent with the participant. Thirdly, motivation they received in the additional very early mobilisation group [15]. The strength of the present study is its eligibility criteria were broad to include a wide range of subjects with stroke. Prospective randomised controlled trial with concealed allocation, dropout rate at the three months follow-up was less than 5%. This study is the first attempt to look for the effect of very early mobilisation on depression and anxiety in acute stroke individuals in India.
Limitation(s)
Subjects recruited were not the representative of the whole stroke population {Individuals with severe aphasia and deteriorated within the first hour of admission to the hospital and intensive care unit, severe stroke subjects (NIHSS Score >16) were not included in this study}, the power of the study is reduced due to participant attrition. Further inadequate blinding, small sample size, longer follow-up was not studied and documentation of frequency, intensity, and duration of mobilisation was not done due to inadequate resources. Future studies may also benefit from greater sample size to increase the generalisability of the results.
Conclusion(s)
The results of the current study suggest that the very early mobilisation may be potential treatment to prevent or reduce symptoms of depression and anxiety up to three months following acute stroke.
SD: Standard deviation; NIHSS: National institutes of health stroke scale; a: Analysed by Independent Student’s t-test; b: Analysed by Chi-Square test
Intervention group: Very early mobilisation+standard care; SD: Standard deviation; IQR: Inter quartile range; CI=Confidence interval; *Mann-Whitney U-test p-value: <0.05; **Wilcoxon sign rank test p-value: <0.05; ***Wilcoxon sign rank test p-value: <0.05
Intervention group: Very early mobilisation+ Standard care, SD: Standard deviation, IQR: Inter quartile range, CI: Confidence interval; * Mann-Whitney U-test p-value: <0.05;** Wilcoxon sign rank test p-value: <0.05; *** Wilcoxon sign rank test p-value: <0.05
*Analysed by Chi-square test, p>0.05 indicates association between groups; Intervention group: Very early mobilisation+standard care