CT Findings in Melioidosis: A Case Report
Amala Ammu Mathew1, Rohini Avantsa2, U Shrikrishna3
1 Junior Resident, Department of Radiodiagnosis, K S Hegde Medical Academy, Mangalore, Karnataka, India.
2 Professor, Department of Radiodiagnosis, K S Hegde Medical Academy, Mangalore, Karnataka, India.
3 Head, Department of Radiodiagnosis, K S Hegde Medical Academy, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Amala Ammu Mathew, Siliconia Apartments, Permanur, Ullal, Mangalore-575017, Karnataka, India.
E-mail: amalaammumathew@gmail.com
Melioidosis is caused by Burkholderia pseudomallei. Even though it affects multiple organs, the most affected organ is lung followed by spleen. It has radiological features which is a mimicker of tuberculosis and is being commonly misdiagnosed as tuberculosis in India. In patients with septicaemia or a fever of unknown aetiology high suspicion is required for the diagnosis. We present a pictorial review of the radiological manifestations in a patient presenting with multi-visceral abscesses which will help radiologists to arrive at an early diagnosis.
Burkholderia pseudomallei, Contrast-enhanced computed tomography, Hepatic abscess, Splenic abscess
Case Report
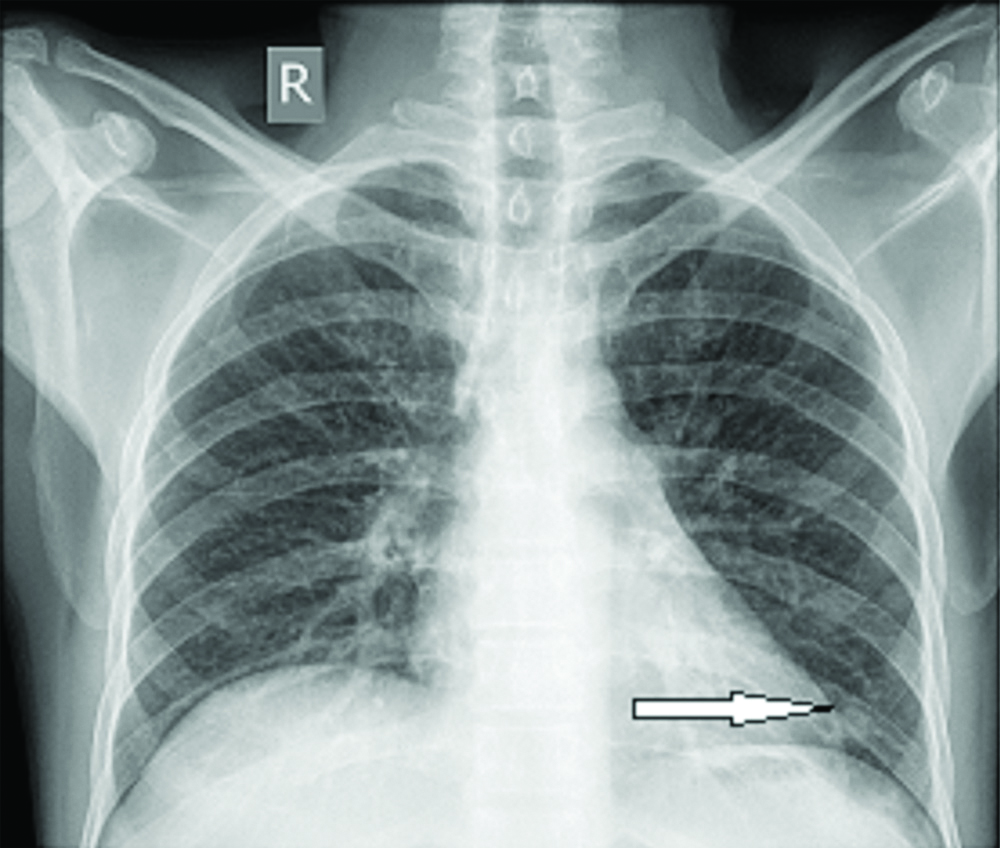
A 46-year-old male patient presented with a five-day history of fever and abdominal pain. Patient had history of alcoholic liver disease and chronic calcific pancreatitis. The patient was a known type 2 diabetic and was on insulin for 14 years with poor control of diabetes. His TLC was 6700/cmm and Neutrophills were 86%, lymphocytes 13%. ESR was 90. Serum bilirubin was 3.5 mg/dL, A/G ratio was 0.5, SGPT was 63 U/L, SGOT was 85 U/L, ALP was 535 U/l, blood urea and serum creatinine was normal. Sputum AFB was negative. His haemoglobin level was 10 gm/dL. Patient was evaluated for dengue, typhus and malaria and results were negative. No history of tuberculosis or contact with TB patients. With this clinical background, the patient was subjected to radiological investigations and was subjected to chest X-ray, USG abdomen and pelvis. X-ray chest (PA View) showed two ill-defined homogenous rounded opacities in the left lower zone [Table/Fig-1]. No evidence of pleural effusion and no features of mediastinal widening/hilar opacities were found.
X-ray chest shows ill-defined rounded opacities (white arrow) in the left lower zone.
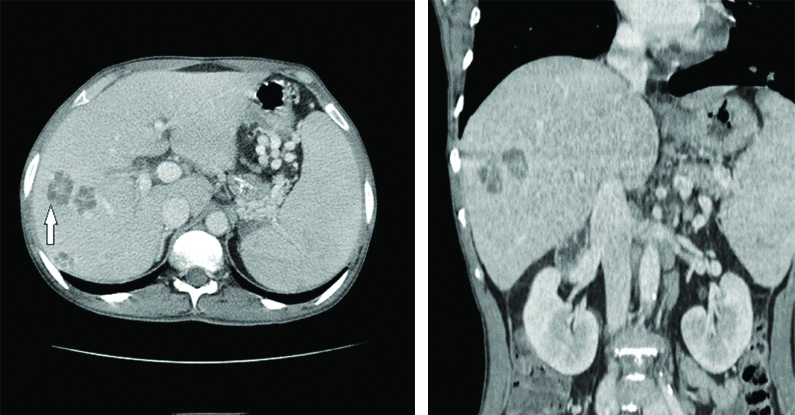
Ultrasonography and doppler evaluation showed multiple hypoechoic lesions in both lobes of the liver measuring less than 1 cm in diameter. There was splenomegaly with multiple hypoechoic lesions (possibly representing abscesses). Further the prostate was enlarged with heterogeneous parenchyma and showed multiple hypoechoic to anechoic areas within, suggestive of evolving abscess. The lesions did not show any colour uptake on doppler evaluation. The differential diagnosis considered was Tuberculosis and Meliodosis. The patient was further subjected to CECT Abdomen and thorax to further characterise the lesions. Contrast-Enhanced CT (CECT) showed the following features. Liver showed multiple solitary and multiloculated peripherally enhancing fluid density lesions in both lobes largest in segment VII measuring 25×21 mm [Table/Fig-2]. Few lesions were noted in the subcapsular location with extension to perihepatic region. The lesions showed characteristic enhancing internal septations which were presented as cartwheel or honeycomb pattern [Table/Fig-2].
Hepatic melioidosis. Axial and coronal computed tomography scan showing multiple discrete liver abscesses with typical cartwheel or honey comb pattern (arrow).
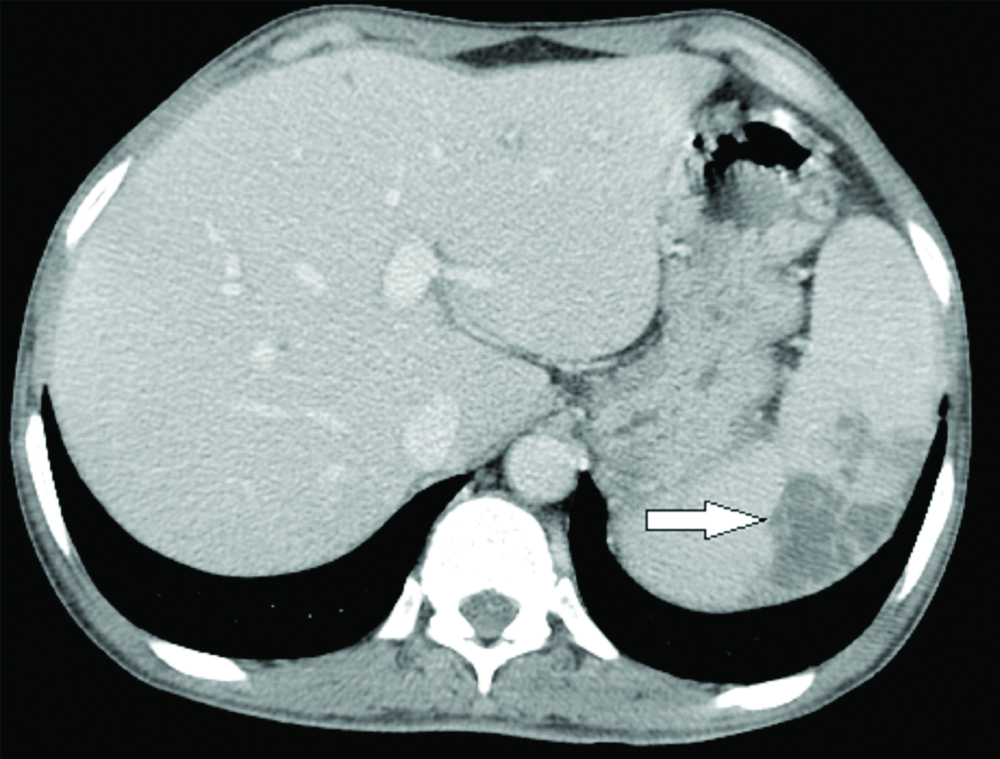
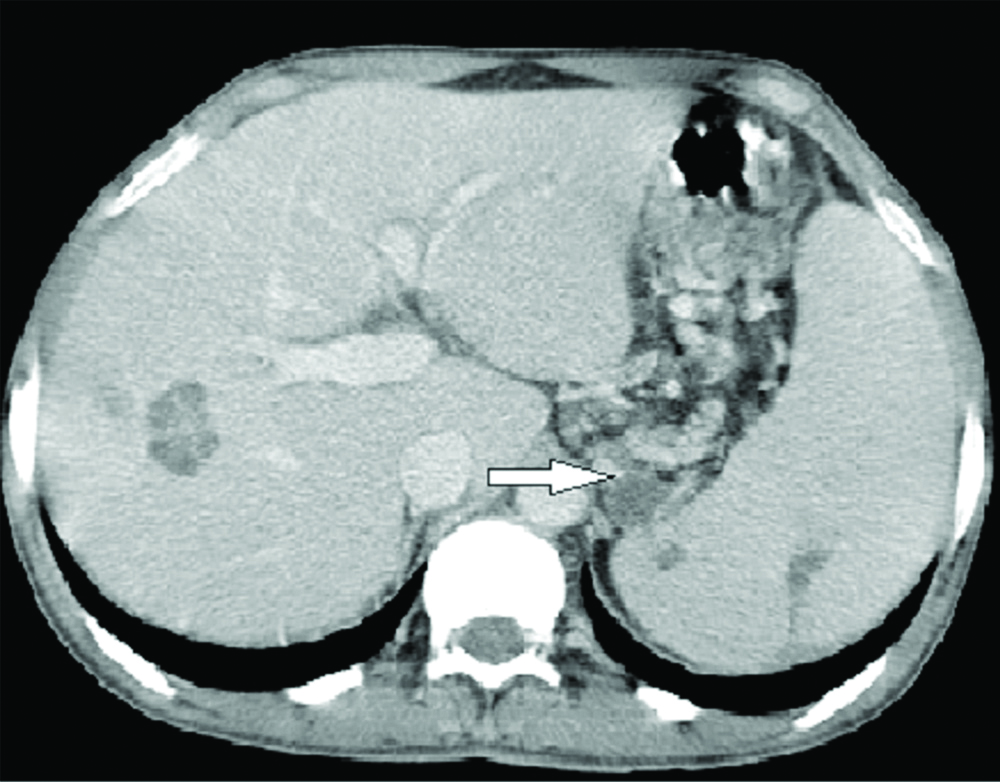
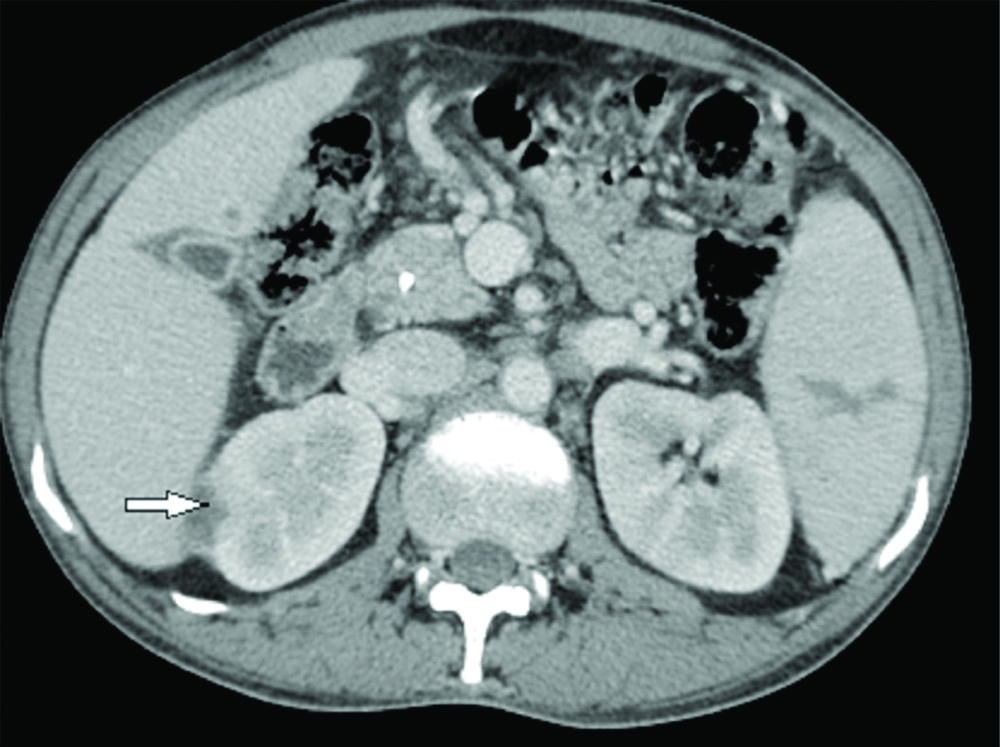
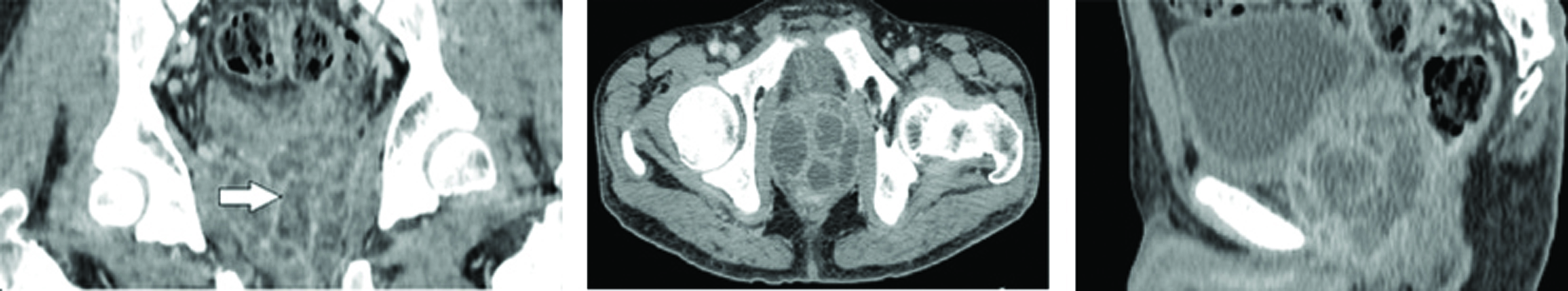
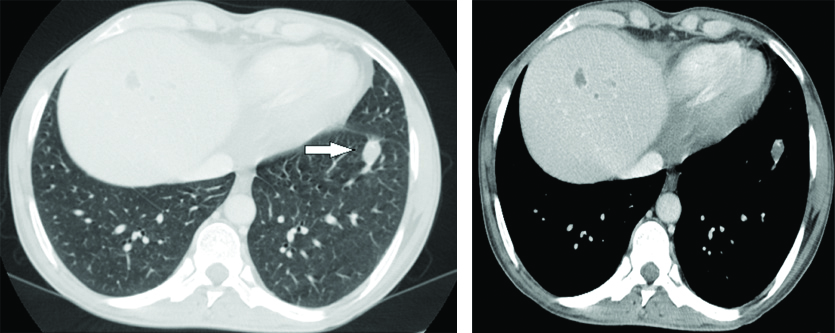
Spleen was enlarged in size with multiple subcapsular solitary and multiloculated peripherally enhancing hypodense lesions. Large abscess with diameter greater than 5 cm were revealed usually called “necklace sign” due to multiple lesions with peripheral location [Table/Fig-3]. Few similar lesions were seen in gastrosplenic space abutting tail of pancreas, fundus of stomach and medial surface of spleen [Table/Fig-4]. Multiple multiloculated enhancing hypodense lesions were noted in both kidneys with few of them having pericapsular extension [Table/Fig-5]. Prostate was enlarged in size and showed multiple multiloculated peripherally enhancing hypodense lesions [Table/Fig-6]. Fluid density lesions were seen in left lung lower lobe anterior basal segment and in lingual [Table/Fig-7]. Blood culture showed Burkholderia pseudomallei. Treatment with i.v ceftazidime with cotrimoxazole for two weeks followed by eradication therapy with Cotrimoxazole for six months was advised.
Splenic abscesses (white arrow). Multiple hypodensities in spleen with melioidosis. Note that spleen is mildly to moderately enlarged.
Few hypodense lesions (arrow) are seen in gastrosplenic space.
Axial images showing hypodense lesions in both kidneys (arrow).
Axial, coronal and sagittal CECT of the abdomen shows multiple ill-defined peripherally enhancing collections in prostate. (white arrow).
CECT of thorax shows well-defined hypodense lesion in the left lung (arrow).
Discussion
Burkholderia pseudomallei enter commonly through a skin epithelial defect, and majority of human cases are due to percutaneous inoculation. Inhalation and ingestion are other known routes. The patients can have multiple clinical presentations from being asymptomatic to being in a septicaemic state [1]. Melioidosis is endemic to Northern Australia and Asia. The annual incidence of Melioidosis is 12.7/100,000 in the tropical countries [1]. About 90% mortality rate is seen in untreated cases hence accurate diagnosis is essential. The patients at risk are those who are exposed to wet soil and patients with diabetes, chronic liver disease and other immunocompromised conditions [1]. It can have acute and chronic presentation. It can present either as asymptomatic infection, septicaemia, localised infection, multiple abscesses involving any organ [1]. Because of the similarity in clinical and radiological manifestations, it is usually mistaken for other infections like tuberculosis especially in India where tuberculosis is prevalent. Limited awareness of the disease leads to underdiagnosis. Melioidosis should always be considered as a differential in patient presenting with focal abscesses especially in diabetic patients. It is a treatable condition and hence, high index of suspicion should be present when a diabetic patient presents concurrent liver and splenic abscesses. Usually patients with melioidosis have multiple pulmonary nodules. Pneumonia is one of the most common clinical presentations in pulmonary melioidosis. Patients had multiple parenchymal lung nodules with no evidence of mediastinal lymph adenopathy and pleural effusion. Patient did not have any features of consolidation. Pneumothorax as a complication of pulmonary melioidosis is very rare and was not seen in present patient [2]. Patients usually have multiple hepato-splenic abscesses [3]. Present patient had multiple abscesses in liver, spleen, kidneys, peritoneum and prostate. Prostate abscess is usually not a very common finding and was found in present case. Abscesses in gastrosplenic space found in present case are very unusual. CNS findings ranging from cerebritis to well-defined macroabscess. In present patient CT brain was normal. Ultrasound abdomen helps detecting microabscesses in liver, spleen and other solid organs. CECT thorax helps to identify diffuse nodular opacities which can involve the lung, coalescent nodular pattern, cavitatory nodules or consolidation. CECT abdomen and pelvis plays a major role in identifying abscesses in liver, spleen and other solid organs. Contrast study of brain helps to identify CNS findings range from cerebritis to well-defined macroabscess [1]. Lung is the most involved organ and the radiological features are small nodular densities which predominantly involves upper lobe [2]. Sparing of the lung apex and presentations with concurrent liver and splenic abscesses helps in diagnosing melioidosis from tuberculosis. Mediastinal lymphadenopathy and pleural effusion are usually seen in tuberculosis and not in Melioidosis and thus helps in differentiating from tuberculosis [3].
Spleen is the most common extrapulmonary organ to be affected, followed by liver, kidneys, prostate. Concurrent spleen and liver abscess are usually seen with Melioidosis than with infections caused by other organisms. Burkholderia pseudomallei is the most common causative agent found in patients with spleen and liver abscesses and confirming the organism in blood culture is the definitive diagnosis. Therefore, empirical antibiotics should be started if the patient is from, or has travelled to an endemic area and presents with multiple splenic abscesses with or without concurrent liver abscess [4]. Abscesses appear as multiple small hypoechoic lesions or as multiloculated hypoechoic lesions with no evidence of internal vascularity on USG. On CT, abscesses appear as multiple small discrete lesions or multiple peripherally enhancing multiloculated hypodense lesions [5]. Multi-loculated lesions may represent either a cluster of multiple small lesions or coalescence of multiple small abscesses. Honeycomb pattern of liver abscess and “necklace sign” in lesions with diameter greater than 5 cm and in lesions with multiple peripheral loculations is characteristic of Melioidosis. Detection of splenic abscess alone should raise a high suspicion of Melioidosis [5]. Involvement of kidneys varies from multiple ill-defined or well-defined hypodensities, rim enhancing lesions, abscess and pyelonephritis [6]. Prostate involvement is unusual and the CECT manifestation is enlarged gland with multiple small non-enhancing fluid densities [7]. It has a predilection for peripheral zone [8]. Hence, prostate specific antigen can be normal or mildly increased. Present case patient presented with these rare involvement. Primary skin infection tends to occur in younger patients. Musculoskeletal involvement is usually part of multisystem Melioidosis and a localised form is less common [9].
Conclusion(s)
Imaging findings of Melioidosis may be similar to many other infections, especially tuberculosis. Multisystem involvement, characteristic appearance of abscesses, presence of multiple splenic abscess, concurrent hepatic and splenic abscesses, multiple abscesses in prostate, kidneys and peritoneum, lung infiltrate which spare apex and absence of lymph nodes gives a clue. An awareness of this condition affecting patients with comorbid disease like diabetes, chronic liver disease is important for early diagnosis and prompt treatment.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 27, 2019
Manual Googling: Jan 08, 2020
iThenticate Software: Jan 13, 2020 (4%)
[1]. Bala Raghu Raji V, Vasanthraj PK, Ramachandran R, Sai V, Multi-system infection- tuberculosis or melioidosis?Egypt J Radiol Nucl Med 2018 49(3):689-92.10.1016/j.ejrnm.2018.03.012 [Google Scholar] [CrossRef]
[2]. D’silva A, Jayannan J, Karnam A, Nair S, Vasanthi N, Bilateral pneumothorax-rare manifestation of melioidosisJ Clin Diagn Res 2018 12(9):OD05-06.10.7860/JCDR/2018/37171.12057 [Google Scholar] [CrossRef]
[3]. Currie BJ, Melioidosis: An important cause of pneumonia in residents of and travellers returned from endemic regionsEur Respir J 2003 22(3):542-50.10.1183/09031936.03.0000620314516149 [Google Scholar] [CrossRef] [PubMed]
[4]. Madhu SD, Melioidosis: A rare but emerging infectious disease in India and role of radiologist in diagnosisIJARS 2016 5(3):6 [Google Scholar]
[5]. Muttarak M, Peh WCG, Euathrongchit J, Lin S-E, Tan AGS, Lerttumnongtum P, Spectrum of imaging findings in melioidosisBr J Radiol 2009 82(978):514-21.10.1259/bjr/1578523119098086 [Google Scholar] [CrossRef] [PubMed]
[6]. Patro S, Panda S, Mishra D, Keerthi S, Burkholderia infections in diabetic patients emerging as a challenge for physicians: A case seriesJ Clin Diagn Res 2019 13:OD04-07.10.7860/JCDR/2019/39889.12671 [Google Scholar] [CrossRef]
[7]. Sood S, Khedar RS, Joad SH, Gupta R, Septicaemic melioidosis: Case report from a non-endemic areaJ Clin Diagn Res 2014 8(12):DD01-DD02.10.7860/JCDR/2014/9684.525725653950 [Google Scholar] [CrossRef] [PubMed]
[8]. Chee YC, Chee YN, An unusual case of primary melioidotic prostatic abscess complicated by perianal abscessID Cases 2018 11:51-52.10.1016/j.idcr.2018.01.00129349040 [Google Scholar] [CrossRef] [PubMed]
[9]. Huang WY, Wu G, Chen F, Li MM, Li JJ, Multi-systemic melioidosis: A clinical, neurological, and radiological case study from Hainan Province, ChinaBMC Infect Dis 2018 18(1):64910.1186/s12879-018-3569-830541464 [Google Scholar] [CrossRef] [PubMed]