Rhupus syndrome is a rare condition of overlap of Rheumatoid Arthritis (RA) and Systemic Lupus Erythematosus (SLE) presenting with erosive polyarthritis and symptoms of SLE. It occasionally has renal involvement as its complication makes the diagnosis more difficult. Here the authors present a case of a 13-year-old female with severe arthritis, which gradually progressed into lupus nephritis with the presence of specific autoantibodies confirming the diagnosis of Rhupus. The child was managed with disease modifying anti-rheumatic drug (hydroxychloroquine), immunosuppressants (mycophenolate mofetil), steroid (prednisolone) and calcium channel blocker (amlodipine). Accurate diagnosis is the key for early detection since Rhupus is a very rare disorder with very limited reported cases.
Diagnosis, Rheumatoid arthritis, Systemic lupus erythematosus
Case Report
A 13-year-old female child was admitted to the hospital with the complaints of pain and swelling in both knee joints for 18 months. She was unable to stand or walk without support. She had recurrent episodes of fever with swelling of hands and feet since last one year (which could probably be RA). She was treated with Non-Steroidal Anti-Inflammatory Drug (NSAID) for the last seven months, before being referred to us due to lack of any sign of improvement in joints swelling.
On examination, she had swelling and contracture of both knee joints with restricted movements, had mild ascites with parietal oedema and bilateral pedal oedema. Vital signs and other systemic examinations were within normal parameters. She belonged to a low socioeconomic family and had no other significant medical and family history.
Laboratory investigations showed anaemia (haemoglobin: 4.8 gm/dL) with an increased Erythrocyte Sedimentation Rate (ESR) of 90 mm/ 1st hour. Antinuclear antibodies (ANA) HEp2 (Human Epithelial type 2) was positive; however, serum (complement) C3 (68 mg/dL) and serum albumin were low (0.84 g/dL). The urine protein was 6.3 mg/gm and serum creatinine was 1.2 mg/dL. The patient was positive for RA factor and Direct Coombs Test (DCT). Ultrasonography (USG) abdomen showed bilateral enlarged echogenic kidneys, mild ascites and pleural effusion. Initially, on admission, she was managed with intravenous antibiotics, methyl prednisolone, analgesics, albumin, fresh frozen plasma and packed red blood cells.
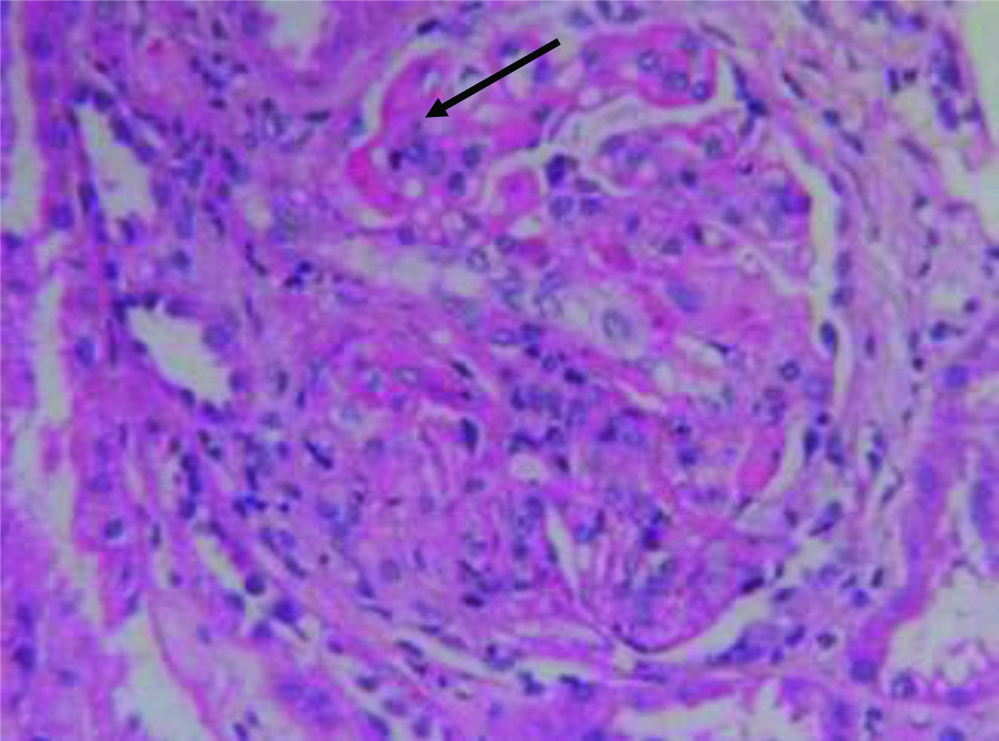
In view of the nephrotic range proteinuria, hypertension and hypocomplementemia, renal biopsy was performed. It revealed, fibrinoid tuft necrosis, diffuse proliferative class IV lupus nephritis, a mild increase in tubulointerstitial chronicity [Table/Fig-1]. Immuno-Fluorescence (IF) study showed full house (IgA 2+, IgG 3+, IgM2+, C3 2+, C1q 2+, kappa and lambda light chains 3+).
Light microscopy of renal histopathology.
Stained with H&E, PAS, MT and silver methenamine showed enlarged glomeruli with diffuse increases in mesangial matrix and cellularity, fibrinoid tuft necrosis (arrow mark), endocapillary cellularity and diffuse thickening of capillaries suggestive of ISN/RPS 2018 Class IVLN
She was diagnosed with Rhupus and was started with Disease Modifying Anti-Rheumatic Drugs (DMARDs) hydroxychloroquine at a dose of 5 mg/Kg/day for RA, mycophenolate mofetil at a dose of 1000 mg/m2 body surface area, prednisolone at a dose of 1.5 mg/Kg/day. To manage the cardiac and renal load, calcium channel blocker and diuretics, amlodipine and furosemide, respectively, were started.
Gradually, the pain and oedema subsided and the patient was discharged with the above medications to be continued. The dose of prednisolone was tapered to 1 mg/Kg/day after three months follow-up, as there was improvement in oedema and swelling of joints.
Discussion
The term Rhupus was first used in 1971 for patients who showed symptoms and laboratory parameters of both RA and SLE. Both the conditions are connective tissue disorders and in very rare cases they are seen together, hence it is difficult to comment whether they belong to a single disease or are two separate entities or are the articular manifestations of SLE [1]. According to few studies, Rhupus is considered to be an overlap disease [2,3]. Here, we presented such a rare case with clinical and laboratory findings suggestive of both RA and SLE along with renal manifestations.
Around 5-30% of cases of SLE have reported symptoms of overlap, of which, with RA it is seen in only 1% of cases [4,5]. Rhupus is such a rare disease in which the symptoms of SLE and RA overlap each other. The prevalence of this disease is only 0.09% [6] and was first named by Schur in 1971 [7]. However, it is still debated, whether Rhupus is a separate entity, or an overlap of SLE and RA or is an SLE with articular involvement. It is manifested as deforming and erosive polyarthritis along with symptoms of SLE and the presence of highly specific antibodies for SLE such as anti-dsDNA and anti-SM and for RA (ACPA) [8,9]. Rhupus is clinically characterised by erosive polyarthritis, rheumatoid nodules, malar rash, photosensitivity, alopecia and renal and neurological affections with the presence of certain autoantibodies [10].
Around 30-50% of patients with SLE might have renal disease like lupus nephritis. But very few case reports of Rhupus with renal involvement are documented in literature (based on PubMed/Google Scholar/hand searching, without language and time limit) [Table/Fig-2] [10-12]. Three studies have been published yet as per our knowledge, which have identified renal manifestations in presence of RA and SLE. It has even been postulated that patients with connective tissue disease might develop renal manifestations owing to the therapy administered for the disease such as penicillamine, NSAIDS, anti-tumour necrosis factor drugs. Beck LH and Salant DJ has also confirmed this association, as discontinuation of these drugs caused improvement in proteinuria in all cases [13].
Published cases of Rhupus syndrome overlapping with renal complications.
| Author | Language of publication | Description |
|---|
| Zhao XJ et al., [10] | Chinese | One female patient with cryoglobulinemia associated renal damage was described. |
| Li J et al., [11] | English | A total of 22 patients (39.3%) with Rhupus Syndrome and SLE had renal disorders demonstrating significant correlation (p=0.002). |
| Benavente EP and Paira SO [12] | Spanish | Of the four patients with Rhupus, one patient had presented renal affection. |
Data was collected only from abstracts for articles other than English [10-12].
Overall Rhupus is seen to be reported more in females than male [14]. In the majority of the cases, the manifestation of RA are seen first followed by SLE, as was observed in present patient [5]. Even in a study by Li J et al., 83.9% cases of Rhupus had onset with RA [11]. Even in present patient, she started with manifestations of rheumatic fever followed by joint complaints which progressed and gradually wre overlapped with nephrotic complications. According to genetic studies; there is shared autoimmunity in the development of both RA and SLE [8].
Few authors have encountered renal involvement in cases of Rhupus presenting with lupus nephritis. [Table/Fig-2] summarises Rhupus syndrome overlapping with renal complications. The index patient developed RA at a younger age, hence it was important to examine such patients carefully to rule out any other associative disease. Initially, she was managed with analgesics and steroids for joint pains but the presence of autoantibodies confirmed Rhupus. The deranged renal parameters made renal biopsy mandatory which showed lupus nephritis thus assuring the diagnosis. Specific diagnostic tests are the key for a confirmed diagnosis of Rhupus. Since the number of cases is limited, even the most beneficial treatment regime is not standard. It is similar to the regimen followed for erosive arthropathy as in RA which comprises of methotrexate or DMARDs, corticosteroids and immunosuppressants. The exact aetiology for nephritic changes is unknown and it could be a result of renal damage due to NSAIDs for RA or damage caused due to the immunocomplex deposits in the renal system [15,16].
Rhupus is a rare condition and delay in diagnosis may cause deformities or other organ complications as in present case. Patient’s renal state was deteriorating and could have progressed to End Stage Renal Disease (ESRD) if not managed promptly.
Conclusion(s)
Rhupus is a rare syndrome which is yet to be completely explored. The radiological findings, presence of autoantibodies and response to therapy confirm that it is an overlap of RA and SLE. It is important to know its clinical and serological findings for early diagnosis and treatment to reduce the possible complications.
Data was collected only from abstracts for articles other than English [
10-
12].
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 12, 2019
Manual Googling: Dec 30, 2019
iThenticate Software: Jan 13, 2020 (6%)
[1]. Bennett R, Overlap syndromesKelley’s Textbook of Rheumatology9th ed:1431-48.10.1016/B978-1-4377-1738-9.00086-4 [Google Scholar] [CrossRef]
[2]. Fernández A, Quintana G, Rondón F, Restrepo JF, Sánchez A, Matteson EL, Lupus arthropathy: A case series of patients with rhupusClin Rheumatol 2006 25(2):164-67.10.1007/s10067-005-1149-y15980935 [Google Scholar] [CrossRef] [PubMed]
[3]. Amezcua-Guerra LM, Overlap between systemic lupus erythematosus and rheumatoid arthritis: Is it real or just an illusion?J Rheumatol 2009 36(1):04-06.10.3899/jrheum.08106719208528 [Google Scholar] [CrossRef] [PubMed]
[4]. Iaccarino L, Gatto M, Bettio S, Caso F, Rampudda M, Zen M, Overlap connective tissue disease syndromesAutoimmun Rev 2013 12(3):363-73.10.1016/j.autrev.2012.06.00422743033 [Google Scholar] [CrossRef] [PubMed]
[5]. Tani C, D’Aniello D, DelleSedie A, Carli L, Cagnoni M, Possemato N, Rhupus syndrome: Assessment of its prevalence and its clinical and instrumental characteristics in a prospective cohort of 103 SLE patientsAutoimmun Rev 2013 12(4):537-41.10.1016/j.autrev.2012.09.00423063507 [Google Scholar] [CrossRef] [PubMed]
[6]. Sarkar S, Saha K, Bilateral acute lupus pneumonitis in a case of rhupus syndromeLung India 2012 29(3):280-82.10.4103/0970-2113.9911922919171 [Google Scholar] [CrossRef] [PubMed]
[7]. Schur PH, Systemic lupus erythematosus. In: Beeson PB, McDermott W, editors., edsCecil-loeb Textbook of Medicine 1971 13th edPhiladelphia, PAWB Saunders:821 [Google Scholar]
[8]. Amezcua-Guerra LM, Springall R, Marquez-Velasco R, Gómez-García L, Vargas A, Bojalil R, Presence of antibodies against cyclic citrullinated peptides in patients with ‘rhupus’: A cross-sectional studyArthritis Res Ther 2006 8(5):R14410.1186/ar203616934155 [Google Scholar] [CrossRef] [PubMed]
[9]. Simon JA, Granados J, Cabiedes J, Morales JR, Varela JA, Clinical and immunogenetic characterization of Mexican patients with ‘rhupus’Lupus 2002 11(5):287-92.10.1191/0961203302lu189oa12090562 [Google Scholar] [CrossRef] [PubMed]
[10]. Zhao XJ, Wei T, Dong B, Jia Y, Wang M, Renal damage caused by Rhupus syndrome associated with anti-neutrophil cytoplasmic antibodies vasculitis and cryoglobulinemiaBeijing Da XueXue Bao Yi Xue Ban 2015 47(5):870-74. [Google Scholar]
[11]. Li J, Wu H, Huang X, Xu D, Zheng W, Zhao Y, Clinical analysis of 56 patients with rhupus syndrome: Manifestations and comparisons with systemic lupus erythematosus: A retrospective case-control studyMedicine (Baltimore) 2014 93(10):e4910.1097/MD.000000000000004925170930 [Google Scholar] [CrossRef] [PubMed]
[12]. Benavente EP, Paira SO, Rhupus: Report of 4 casesReumatol Clin 2011 7(5):333-35.10.1016/j.reumae.2010.12.003 [Google Scholar] [CrossRef]
[13]. Beck LH, Salant DJ, Causes and diagnosis of membranous nephropathy. UpToDate B, DS (Ed), editorUpToDate 2013 Waltham, MA [Google Scholar]
[14]. Solis Cartas U, Martínez Larrarte JP, Prada Hernández DM, Gómez Morejón JA, Valdés González JL, Molinero Rodríguez C, Rhupus syndrome. A rare combinationRev Colomb Reumatol 2017 24(4):237-41.10.1016/j.rcreue.2017.05.004 [Google Scholar] [CrossRef]
[15]. Radford MG Jr, Holley KE, Grande JP, Larson TS, Wagoner RD, Donadio JV, Reversible membranous nephropathy associated with the use of nonsteroidal anti-inflammatory drugsJAMA 1996 276(6):466-69.10.1001/jama.1996.03540060042033 [Google Scholar] [CrossRef]
[16]. Santos R, Silva R, Malvar B, Pessegueiro P, Pires C, Nephrotic proteinuria in a patient with RhupusPort J Nephrol Hypert 2013 27(4):295-99. [Google Scholar]