A Case of Tracheo-Bronchomegaly in a Young Male
Priti Meshram1, Sanchit Mohan2, Vishwanath Pujari3, Rohit Hegde4
1 Head, Department of Pulmonary Medicine, Grant Government Medical College, Mumbai, Maharashtra, India.
2 Junior Resident, Department of Pulmonary Medicine, Grant Government Medical College, Mumbai, Maharashtra, India.
3 Associate Professor, Department of Pulmonary Medicine, Grant Government Medical College, Mumbai, Maharashtra, India.
4 Associate Professor, Department of Pulmonary Medicine, Grant Government Medical College, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sanchit Mohan, 110,300 Resident Hostel, JJ Hospital, Byculla, Mumbai, Maharashtra, India.
E-mail: sanchit.agarwal1992@gmail.com
Tracheobronchomegaly (TBM) or Mounier-Kuhn syndrome is a disorder characterised by dilatation of trachea and major bronchi with tracheal diverticula leading to bronchiectasis as a complication. We report a 39-year-old male who was admitted at the tertiary care centre for breathlessness and recurrent lower respiratory tract infections, symptomatic for 15 years. He was a non smoker, with no history of similar illness in his family. Chest X-ray (posterior-anterior view) showed tracheal dilatation with bilateral bronchiectasis. Spirometry showed mixed ventilatory defect with poor bronchodilator reversibility in the obstructive component. Dynamic CT scan showed TBM. Fibreoptic bronchoscopy revealed a dilated trachea with prominent tracheal rings and widening of the bronchial tree bilaterally with mucopurulent secretions which were positive for streptococcus pyogenes and Acinetobacter baumanii.
Bronchiectasis, Mounier-Kuhn syndrome, Recurrent infections
Case Report
A 39-year-old male was admitted with chief complaints of breathlessness of MMRC grade 2, cough with yellow mucoid expectoration for two months, fever on and off for two months. He also gave a history of recurrent lower respiratory tract infections; he was symptomatic for 15 years. He was a non-smoker and had no similar family history of similar complaints.
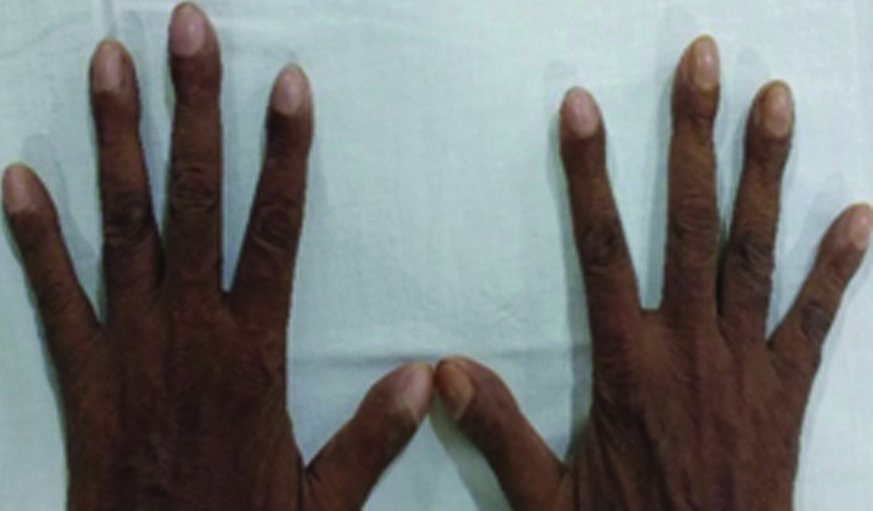
On examination, he was febrile with a heart rate of 120/minute, respiratory rate 24/minute, BP 120/80 mmHg, SPO2 93% on room air at rest, grade 3 clubbing [Table/Fig-1] and crackles in the chest bilaterally on auscultation. He had normal haemoglobin (14.5 gm%) with increased total leukocyte count (16000/cumm) with a neutrophilic predominance and a normal platelet count. All other biochemical tests (RFT, LFT, RBS urine R/M) were within normal limits.
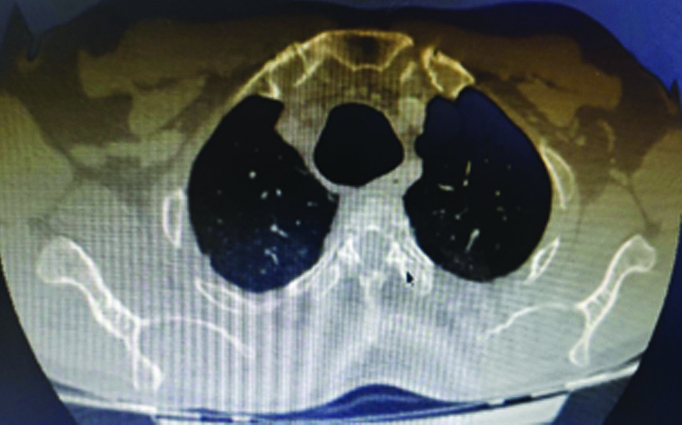
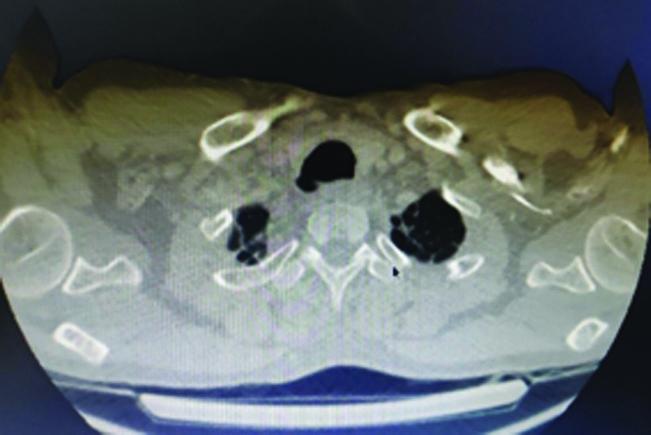
Chest radiograph (PA view) was done [Table/Fig-2] suggestive of bilateral bronchiectasis with dilated trachea. Sputum gram culture showed growth of Streptococcus pyogenes and Acinetobacter baumannii. Spirometry showed mixed ventilatory defect with poor bronchodilator reversibility in the obstructive component. Dynamic CT scan was done and TBM was noted. The trachea was grossly dilated with a diameter of 3.1 cm on inspiration and 2.1 cm on expiration [Table/Fig-3]. The bilateral tracheobronchial tree was also dilated with a diameter of 2.1 cm and 2.2 cm of the right and left bronchus, respectively. Tracheal diverticula were also noted on the right side of the trachea at the level of the thoracic inlet with bilateral cystic bronchiectasis [Table/Fig-4].
Chest X-Ray PA view showed bilateral bronchiectasis. (with Tracheomegaly).

CT Scan showing tracheomegaly.
CT scan showing tracheal diverticula.
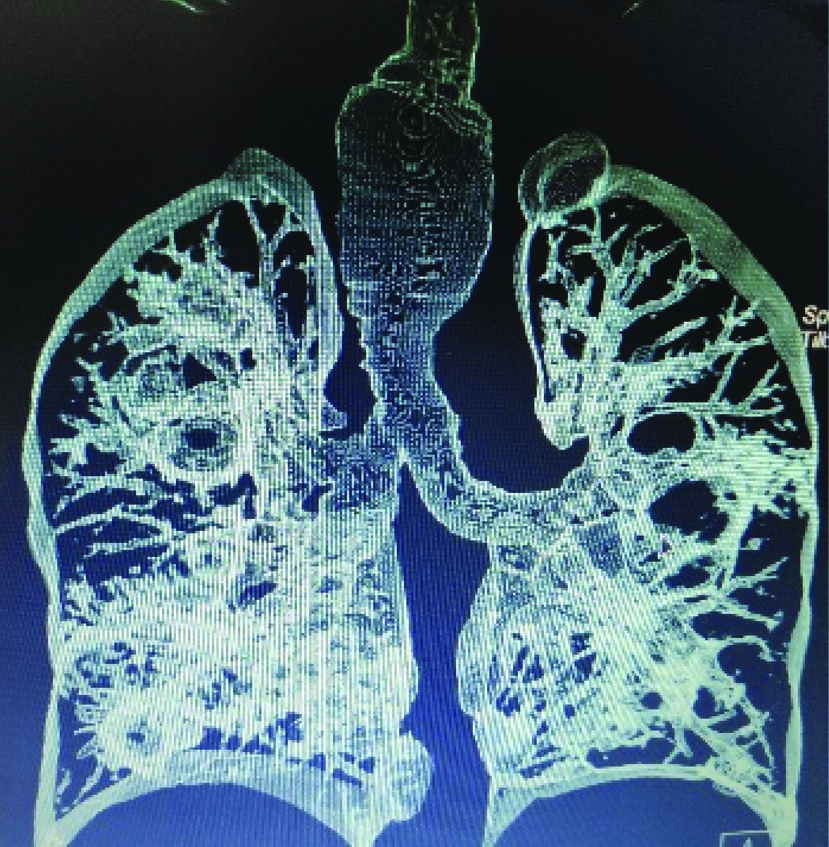
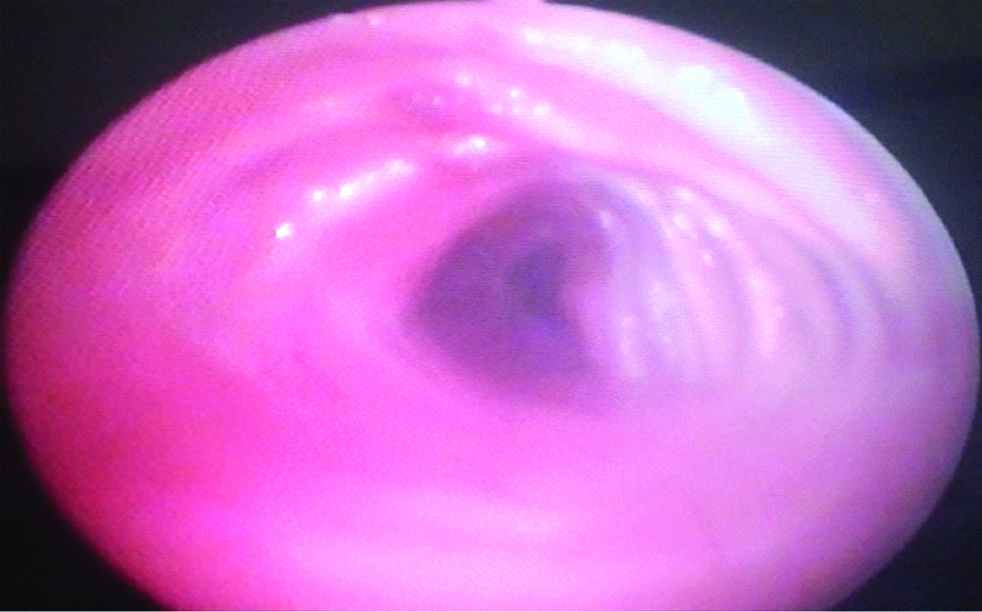
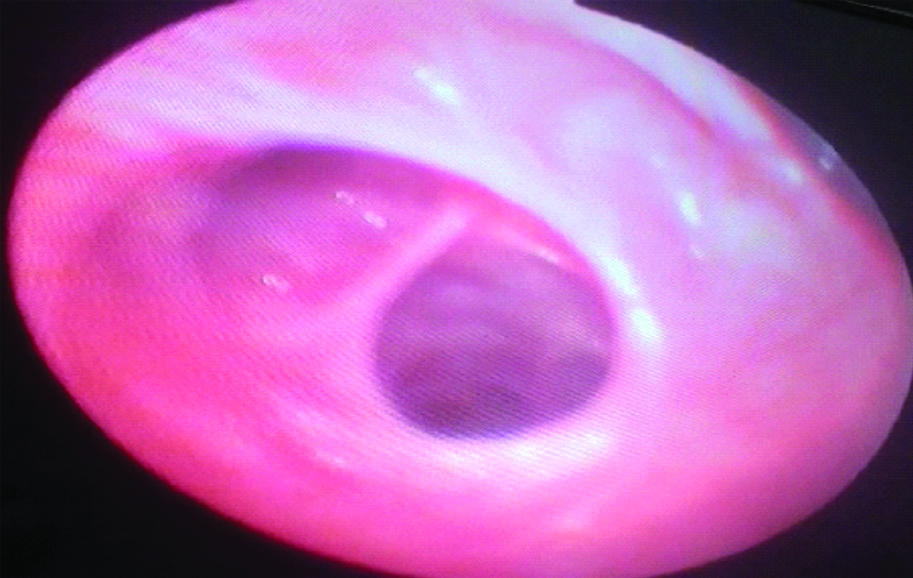
A 3D reconstruction of HRCT also showed bilateral bronchiectasis with tracheomegaly with left apical bulla [Table/Fig-5]. Fibreoptic bronchoscopy revealed dilated trachea [Table/Fig-6] with prominent tracheal rings with tracheal diverticulum and widening of the bronchial tree bilaterally and dilatation of sub-segments [Table/Fig-7] with mucopurulent secretions in bilateral lower lobes and right middle lobe.
3D reconstructed image of HRCT showing bilateral bronchiectasis with tracheomegaly with left apical bulla.
Fibreoptic bronchoscopy showing Dilated trachea with prominent tracheal rings.
Fibreoptic bronchoscopy showing Dilated sub segments.
A diagnosis of Mounier-Kuhn syndrome was established and the patient was started on antibiotics as per culture sensitivity report and Long Acting Muscarinic Antagonist (LAMA) + Long Acting Beta Agonist (LABA) combination. His clinical condition improved and he was discharged with the advice for pneumococcal and influenza vaccination on follow-up. Though all the family members were asymptomatic, they were screened by detailed clinical examination and X-ray chest which were found to be normal.
Discussion
Mounier-Kuhn Syndrome (MKS) is a rare disease characterised by tracheobronchial dilatation which occurs due to absence or atrophy of smooth muscle cell fibres and elastic fibres [1-3]. Involvement can occur from trachea down to fourth order branches. It is seen more commonly in males and is usually diagnosed in third-fourth decade [3,4]. As in this case, it was diagnosed in fourth decade. This patient had mixed ventilatory defect with poor bronchodilator reversibility. Mostafa G et al., had presented a case of Mounier-Kuhn syndrome with normal Pulmonary Function Tests (PFTs) [5].
Clinical presentation of the disease varies from minimal disease with preserved lung function to severe respiratory failure and death. Most cases are sporadic however the autosomal recessive pattern of inheritance has also been reported by some authors [6]. MKS has been classified into three subtypes- Type 1 is characterised by symmetric dilatation of trachea and main bronchi, in Type 2 both dilatation and diverticula are distinct and Type 3 is the most severe type in which diverticula and saccular structures extend up to the distal bronchi [4].
The present case is an example of type-2 MKS. Pathological dilatation and decreased mucociliary function lead to an ineffective cough. This leads to difficulty in the expectoration of secretions and hence patients present with recurrent Lower Respiratory Tract Infection (LRTI) [6].
Radiological features are diagnostic for MKS. A dynamic CT allows direct measurement of tracheobronchial tree in inspiration and as well as expiration and differentiates between TBM and Tracheobronchomalacia which has different line of management as in latter there is a collapse of varying degrees on expiratory scan [7]. Vorakunthada Y and Lilitwat W, presented a case of post-intubation tracheobronchomalacia with recurrent infections [8]. It also demonstrates secondary features like sacculation, bronchiectasis, and scarring. Accepted criteria for diagnosis of tracheabronchomegaly on CT are tracheal diameter >30 mm, right main bronchus diameter >20 mm and left main bronchus diameter >18 mm [4]. The current case had tracheal diameter of 31 mm with right and left main bronchus diameter of 21 mm and 22 mm, respectively. Chest X-ray (CXR) also demonstrates TBM and the criteria for diagnosis on CXR are the tracheal diameter of 30 mm right bronchial tree diameter of 24 mm and left bronchial tree diameter 23 mm [9].
Bronchography is an excellent investigation for demonstration of the extent of disease; however, it is obsolete now. Fibreoptic bronchoscopy can detect tracheal and bronchial dilatation on inspiration and constriction or even collapse during expiration or coughing hence, can differentiate it from trachebronchomalacia [1,6]. Some connective tissue disorders are also associated with TBM like cutis laxa, Ehler-Danlos syndrome, Marfan syndrome, Kenney Caffey syndrome, Brachmann-de Lange syndrome, etc., however, all connective tissue disorders were ruled out in this case [9,10].
Treatment is based on severity. All patients should be advised smoking cessation and avoiding other indoor and outdoor irritants and pollution to prevent further damage to the airway. No specific treatment is required in asymptomatic individuals. In asymptomatic individuals, LAMA+LABA controls breathlessness and chest physiotherapy drains the secretions. Antibiotics are required for infective exacerbation. Though medical management is the mainstay to control symptoms and exacerbations, as in present case who was given optimal medical management and was followed-up every monthly, tracheal stenting can be done in very severe cases. However, lung transplantation and other surgeries have no proven benefit [11].
Conclusion(s)
TBM presents with signs and symptoms of bronchiectasis, however, it can be easily overlooked particularly with plain films. Dynamic CT scan is necessary for differentiating TBM from Tracheobronchomalacia.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 08, 2019
Manual Googling: Dec 02, 2019
iThenticate Software: Jan 11, 2020 (15%)
[1]. Sarper A, Oz N, Demircan A, Isin E, Mounier-Kuhn syndrome: case report [in Turkish]Turk J Thorac Cardiovasc Surg 2002 10(2):116-17. [Google Scholar]
[2]. Ciftci B, Yilmaz A, Erdogan Y, Biber C, Turay UY, Ergun P, Mounier-Kuhn syndrome: a case report and review of the literature [in Turkish]Solunum Hastaliklari Dergisi 2007 18(2):79-83. [Google Scholar]
[3]. Karalezli A, Yurdakul M, Misirli F, Mounier-Kuhn syndrome: A case report (tracheobronchomegaly) [in Turkish]Turkiye Klinikleri J Med Sci 1999 19(1):37-39. [Google Scholar]
[4]. Dunne MG, Reiner B, CT features of tracheobronchomegalyJ Comput Assist Tomogr 1988 12(3):388-91.10.1097/00004728-198805010-000043366947 [Google Scholar] [CrossRef] [PubMed]
[5]. Mostafa G, Mohammadreza P, Jafar A, Noe Z, Mounier Kuhn syndrome: a rare cause of severe bronchial dilatation with normal pulmonary function test: a case reportRespir Med 2007 101(8):1836-39.10.1016/j.rmed.2007.02.00517428651 [Google Scholar] [CrossRef] [PubMed]
[6]. Damgaci L, Durmus S, Pasaoglu E, Mounier-Kuhn syndrome (tracheobronchomegaly)Diagn Interv Radiol 2002 8:165-66. [Google Scholar]
[7]. Kudela O, Kocova E, Sedlak V, Koblizek V, Novotna B, Balzek M, Dynamic CT in diagnostics of tracheomalaciaEuropean Respiratory Journal 2015 46(suppl 59):PA374410.1183/13993003.congress-2015.PA3744 [Google Scholar] [CrossRef]
[8]. Vorakunthada Y, Lilitwat W, Post-intubation tracheobronchomalacia in a young adult: A rare case reportRespir Med Case Rep 2017 23:66-67.10.1016/j.rmcr.2017.12.00729487785 [Google Scholar] [CrossRef] [PubMed]
[9]. Katz I, Levine M, Herman P, Tracheobronchiomegaly. The Mounier-Kuhn syndromeAm J Roentgenol Radium Ther Nucl Med 1962 88:1084-94. [Google Scholar]
[10]. Menon B, Aggarwal B, Iqbal A, Mounier-Kuhn syndrome: Report of 8 cases of tracheobronchomegaly with associated complicationsSouth Med J 2008 101(1):83-87.10.1097/SMJ.0b013e31815d425918176298 [Google Scholar] [CrossRef] [PubMed]
[11]. Ernst A, Majid A, Feller-Kopman D, Guerrero J, Boiselle P, Loring SH, Airway stabilization with silicone stents for treating adult tracheobronchomalacia: A prospective observational studyChest 2007 132(2):609-16.10.1378/chest.06-270817699133 [Google Scholar] [CrossRef] [PubMed]