Infective Endocarditis (IE) in cancer is not very frequently reported. We report an interesting case of a 27-year-old primigravida with 30 weeks pregnancy, who presented with high grade fever with severe anaemia and thrombocytopenia. Twenty days before this presentation, she was evaluated for a gingivobuccal sulcus mass in this hospital, oral examination had revealed a soft, bluish, non-tender patch on her left gingivobuccal sulcus; as per her old document (clinical picture was retrieved from Department of Oral and Maxillofacial Surgery) for which a biopsy was done. Biopsy revealed chronic sialadenitis with metaplastic changes of mucoepidermoid carcinoma. In search of the cause of her fever with anaemia and thrombocytopenia, exhaustive investigations were done but were inconclusive. Dilemma occurred, when she developed preterm labour at 32 weeks and post-delivery, she went into respiratory distress. Embolism was kept as a differential but CT Pulmonary angiography was negative. Then, 2D-ECHO showed a vegetation on the mitral valve. Three sets of blood cultures obtained from different venipuncture sites at 12 hourly intervals were negative however, she responded to intravenous antibiotics. We presume that the chronic sialadenitis associated with malignancy lead to the blood stream dissemination of organisms from oral cavity to native valves causing endocarditis.
Case Report
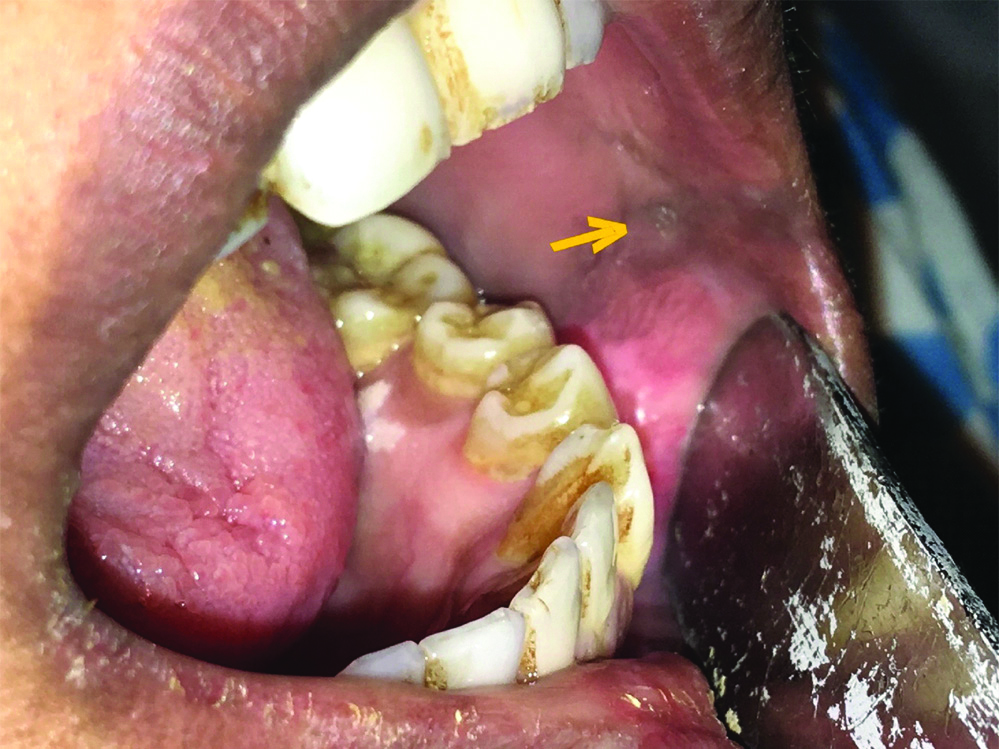
A 27-year-old primigravida with 30 weeks pregnancy presented to the antenatal clinic with high grade fever spikes associated with severe pallor, generalised fatigue and exertional breathlessness. She was chronic tobacco chewer for 10 years. Her vitals were normal at presentation. Twenty days earlier she had presented to the dental OPD in this institute with complaints of feeling of a small lump inside the left mouth with mild left jaw pain. Her oral examination had revealed poor dental and oral hygiene, caries and a soft, bluish, non-tender patchy lesion [Table/Fig-1] (retrieved from Department of Oral and Maxillofacial Surgery) on her left gingivobuccal sulcus, which was suspicious for malignancy and a biopsy was obtained. She was asked for follow-up for the biopsy report, but she didn’t comply. Later, she presented in the antenatal clinics.
Bluish soft patch on left gingivobuccal sulcus (arrow).
In this admission; her abdominal examination revealed 30 weeks gravid uterus with normal Fetal Heart Sound (FHS). General examination: Pulse 110/min, regular, all the peripheral pulses were well felt. Blood pressure was 118/78 mm of Hg in right arm. Pallor was present. Jugular Venous Pulse (JVP) was normal. There was no clubbing and there were no signs of IE visible.
Cardiovascular system examination revealed normal S1 and S2. There was no S3/S4 or murmurs. Respiratory system examination: bilateral air entry was normal, vesicular type. There were no crackles or ronchi. Central nervous system examination revealed normal higher functions, cranial nerves were intact, there were no focal neurological deficits and sensory examination was normal.
Routine labs in this admission revealed; Hb-4.6gm%, MCV-87 fL, TLC-13,400/mm3, Platelets-59000/mm3. Peripheral smear showed normocytic normochromic with mild anisopoikilocytosis showing few microcytes, tear drop cells with reduced platelets. Possibility of haemolysis was ruled out by normal reticulocyte count, Lactate dehydrogenase, normal bilirubin and negative Direct Coomb Test (DCT) and Indirect Coomb Test (ICT). Autoimmune profile was negative which included Antinuclear Antibodies (ANA) and Antiphospholipid Antibodies (APLA) work up. Sickling was also negative with normal Hb electrophoresis. International Normalised Ratio (INR), activated Partial Thromboplastin Time (aPTT) was normal. Peripheral smear for malarial parasite, dengue NS1and IgM, HIV, HbsAg, anti HCV was negative. Possibility was Hemolysis, Elevated Liver Enzymes, Low Platelet Syndrome (HELLP) syndrome was ruled out by normal Blood pressure, normal Liver function test and negative urinary dipstick. She was stabilised with blood transfusions and foetal monitoring was done. Subsequently, her haemoglobin and platelets stabilised and she was monitored in the hospital.
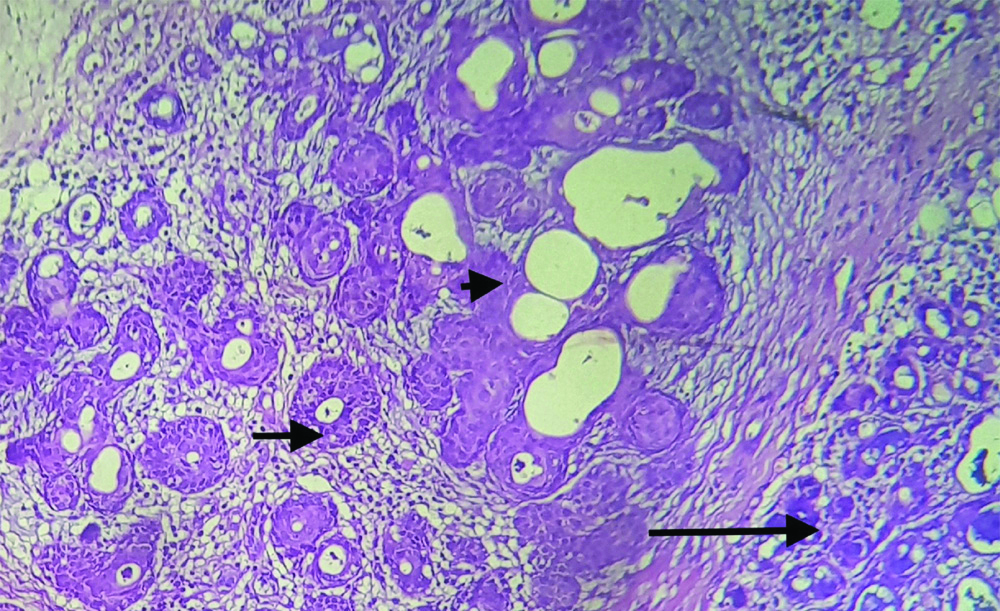
Her medical record was retrieved. Ultrasound of the neck and of her oral lesion revealed the lesion to be hypoechoic with hypervascularity at Doppler with enlarged left submental, submandibular and jugulodigastric node. Biopsy report retrieved showed features suggestive of chronic sialadenitis with metaplastic changes of mucoepidermoid carcinoma [Table/Fig-2].
H&E stained histopathology slide 40x view showing salivary gland tissue, with evidence of chronic sialadenitis (long arrow) along with acinar and ductal structures showing evidence of squamous metaplastic changes (short arrow), with central focus showing the development of mucoepidermoid carcinoma (arrow head) on histopathological examination.
After 2 days, her fever spikes continued and her TLC increased to 17800/mm3. She was started on iv antibiotics. Her counts remained high as 37,100/mm3 with neutrophilic leukocytosis on smear. She was monitored in this hospital. At 32 weeks of her pregnancy, she developed pre-term labour and delivered a preterm female baby by normal vaginal delivery. Baby was managed in NICU.
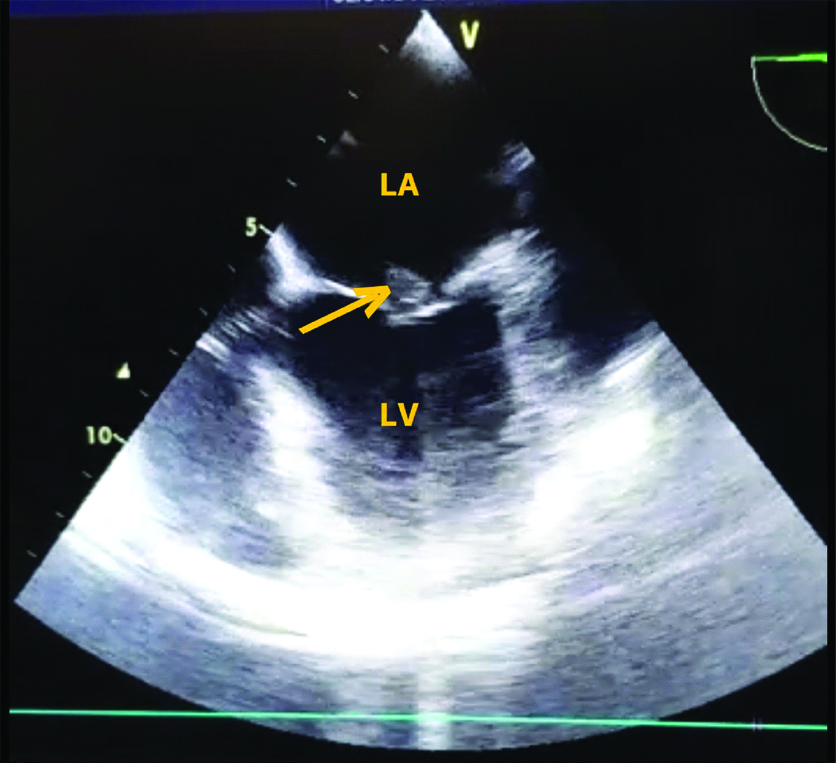
However, eight hours after delivery, she developed sudden respiratory distress. She was intubated prophylactically and kept on ventilator support in Continuous Positive Airway Pressure (CPAP) mode. Possibility of pulmonary embolism was kept when her D-dimer was positive and she was started on Low Molecular Weight Heparin (LMWH). A CT Pulmonary angiography was done which was negative for pulmonary embolism. Her ECG showed inverted t waves in lead I, aVL and deep negative t waves in V2, V3 and V4. Clinically, cardiovascular examination was unremarkable. Troponin I and Creatine Kinase-MB (CK-MB) was negative. A 2D-ECHO showed a vegetation on anterior mitral leaflet with moderate mitral regurgitation which was confirmed by Transoesophageal Echocardiography (TEE) [Table/Fig-3]. Three sets of blood cultures obtained from different venipuncture sites 12 hours apart were negative for any organism. She was started on i.v ceftriaxone and vancomycin. Her two times, three site blood culture revealed no growth. However, she responded to the antibiotics and her condition stabilised, fever settled and counts were also normalised.
Transoesophageal view showing LA with echogenic mass on anterior mitral leaflet (arrow).
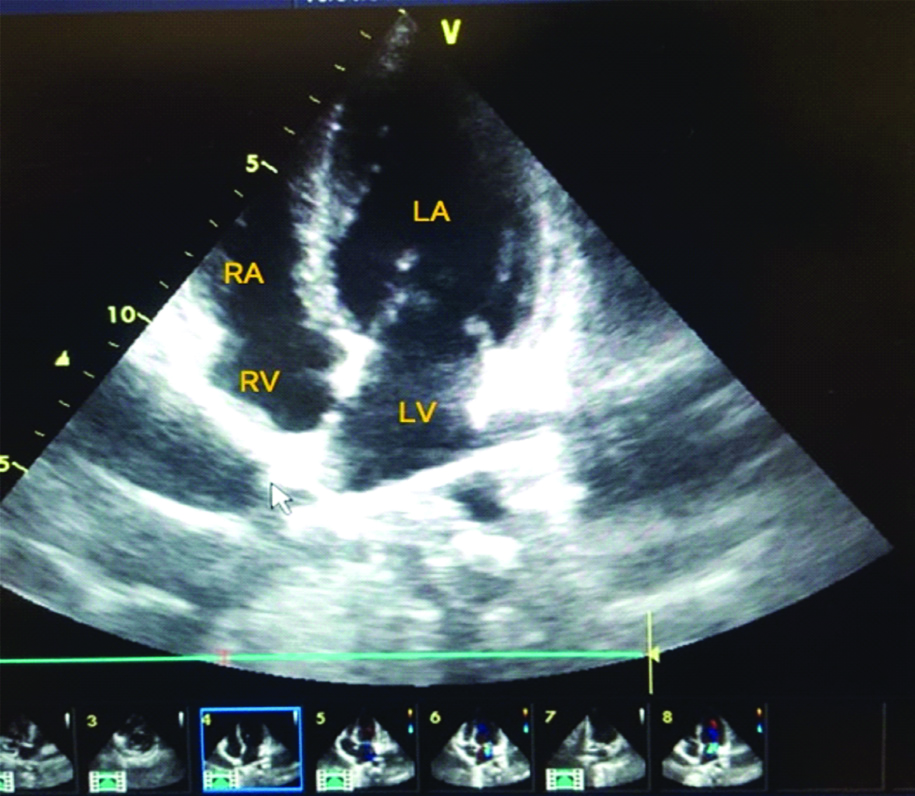
After 4 weeks course of antibiotics, repeat 2D-ECHO was done which showed the resolution of vegetation [Table/Fig-4]. She was then transferred to oral and maxillofacial surgery department for further management of oral mucoepidermoid carcinoma.
Transthoracic four chamber view showing resolution of the vegetation on mitral valve.
Discussion
Infective Endocarditis (IE) is one of the deadly infections known and is associated with large morbidity. Endocarditis is an inflammation of the endocardium and heart valves. McCoy WC and Mason JM in the year 1951, suggested the association of IE with colon cancer [1]. Still, there is scarcity of the data, explaining the association and possible mechanisms.
We report one of the rarest case of a primigravida with 30 weeks pregnancy presenting with high grade fever, clinical examination led to the discovery of her oral mucoepidermoid cancer and further, the exhaustive search of the cause of her fever, lead to the diagnosis of IE. Luckily, she responded well to antibiotics and the vegetation got completely resolved within three weeks.
The changing trend in incidence shows more frequency in elderly and overall incidence of IE is between 2 and 10 episodes per 100,000 person-years in most population-based studies [2-4]. IE most commonly involves mitral valve, followed by the aortic valve, followed by multivalvular disease [5,6].
Earlier, rheumatic heart disease with mitral stenosis was most commonly associated with IE but now more common lesions are mitral regurgitation, aortic valve disease (stenosis and regurgitation), and congenital heart disease [7,8]. Besides, structural heart disease and prosthetic valves, risk factors include previous history of IE, dental procedures, other invasive medical procedures and injection drug abuse. Recently, diabetes mellitus and kidney disease have emerged as potential risk factors as well [9].
Malignancy being a hypercoagulable state, non-bacterial thrombotic endocarditis is frequently seen. But, the association between cancer and IE is also not a new entity. The aetiological relation between Streptococcus bovis and colon cancer has been well described in literature [10]. Infact, the recent European guidelines suggest ruling out of cancer in every patient of IE caused by S. bovis (gallolyticus) [11].
Poor oral hygiene and oral bacteria are well related to onset of IE. Kawamata H et al., in their study of 47 patients with IE, showed that 57.4% of bacteria from blood cultures of the patients were commonly existing bacteria in oral cavity [12]. Similarly, Chocolatewala N et al., in their study have implicated the role of oral bacteria in oral cancer [13].
Occurrence of IE in pregnancy is extremely rare, the incidence being around 0.006% [14]. The index patient did not have any evidence of prior rheumatic affection of valves. In this case mucoepidermoid carcinoma with superadded sialadenitis and poor orodental hygiene may have contributed to IE. It is also possible that the malignancy was a chance coincidental finding which was incidentally discovered on clinical examination although she was asymptomatic. The only possible source for development of IE was sialadenitis which might have been an association or; it existed prior to development of malignancy. Though, she was a tobacco chewer, interestingly, her malignancy was unrelated. Biopsy proved it to be chronic sialadenitis with metaplastic changes of mucoepidermoid carcinoma.
Conclusion(s)
We report an unusual case of IE in a 27-year-old primigravida with 30 weeks pregnancy who presented with high grade fever spikes with anaemia and thrombocytopenia. Diagnostic work-up unveiled her silent oral gingivobuccal malignancy (mucoepidermoid carcinoma) which was due to chronic sialadenitis. This case adds on to the association between IE and cancer and strengthens the fact that IE can be a prelude to malignancy. Still, more research is required to prove the possible linkage.
[1]. McCoy WC, Mason JM, Enterococcal endocarditis associated with carcinoma of the sigmoid: Report of a caseJ Med Assoc Stat Alab 1951 21(6):162-66. [Google Scholar]
[2]. Berlin JA, Abrutyn E, Strom BL, Kinman JL, Levison ME, Korzeniowski OM, Incidence of infective endocarditis in the Delaware Valley, 1988-1990Am J Cardiol 1995 76(12):933-36.10.1016/S0002-9149(99)80264-1 [Google Scholar] [CrossRef]
[3]. Moreillon P, Que YA, Infective endocarditisLancet 2004 363(9403):139-49.10.1016/S0140-6736(03)15266-X [Google Scholar] [CrossRef]
[4]. Cabell CH, Fowler VG, Engemann JJ, McClellan M, Heidenreich P, Endocarditis in the elderly: Incidence, surgery, and survival in 16,921 patients over 12 yearsCirculation 2002 106(19):547 [Google Scholar]
[5]. Miro JM, Anguera I, Cabell CH, Chen AY, Stafford JA, Corey GR, Staphylococcus aureus native valve infective endocarditis: Report of 566 episodes from the International Collabouration on Endocarditis Merged DatabaseClin Infect Dis 2005 41(4):507-14.10.1086/43197916028160 [Google Scholar] [CrossRef] [PubMed]
[6]. McDonald JR, Olaison L, Anderson DJ, Hoen B, Miro JM, Eykyn S, Enterococcal native valve endocarditis: Report of 107 episodes from the International Collabouration on Endocarditis Merged DatabaseAm J Med 2005 118(7):759-66.10.1016/j.amjmed.2005.02.02015989910 [Google Scholar] [CrossRef] [PubMed]
[7]. Michel PL, Acar J, Native cardiac disease predisposing to infective endocarditisEur Heart J 1995 16(SupplB):2-6.10.1093/eurheartj/16.suppl_B.27671919 [Google Scholar] [CrossRef] [PubMed]
[8]. Weinberger I, Rotenberg Z, Zacharovitch D, Fuchs J, Davidson E, Agmon J, Native valve infective endocarditis in the 1970s versus the 1980s: Underlying cardiac lesions and infecting organismsClin Cardiol 1990 13(2):94-98.10.1002/clc.49601302062407399 [Google Scholar] [CrossRef] [PubMed]
[9]. Strom BL, Abrutyn E, Berlin JA, Feldman RS, Stolley PD, Levison ME, Risk factors for infective endocarditis: Oral hygiene and nondental exposuresCirculation 2000 102:2842-48.10.1161/01.CIR.102.23.284211104742 [Google Scholar] [CrossRef] [PubMed]
[10]. Boleij A, van Gelder MM, Swinkels DW, Tjalsma H, Clinical importance of Streptococcus gallolyticus infection among colorectal cancer patients: Systematic review and meta-analysisClin Infect Dis 2011 53(9):870-78.10.1093/cid/cir60921960713 [Google Scholar] [CrossRef] [PubMed]
[11]. Habib G, Lancellotti P, Antunes MJ, Bongiomi MG, Casalta JP, Del Zotti F, 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM)Eur Heart J 2015 36(44):3075-128.10.1093/eurheartj/ehv31926320109 [Google Scholar] [CrossRef] [PubMed]
[12]. Kawamata H, Hakata K, Okubo M, Uchida D, Association of the oral bacteria with onset of the infective endocarditisInternational Journal of Oral and Maxillofacial Surgery 2015 44(Supplement 1):e24010.1016/j.ijom.2015.08.169 [Google Scholar] [CrossRef]
[13]. Chocolatewala N, Chaturvedi P, Desale R, The role of bacteria in oral cancerIndian Journal of Medical and Paediatric Oncology: Official Journal of Indian Society of Medical & Paediatric Oncology 2010 31(4):126-31.10.4103/0971-5851.7619521584217 [Google Scholar] [CrossRef] [PubMed]
[14]. Montoya ME, Karnath BM, Ahmed M, Endocarditis during pregnancySouth Med J 2003 96(11):1156-57.10.1097/01.SMJ.0000054503.18393.1E14632369 [Google Scholar] [CrossRef] [PubMed]