Introduction
Periodontitis is an infectious inflammatory disease destroying the tooth-supporting tissues, and if untreated, leading to the tooth loss [1]. Periodontal diseases are very common and cause remarkable costs. Some 5% to 20% of adults suffer from severe generalised periodontitis depending on how the disease is defined and how old they are [2,3]. The disease also occurs in adolescents, even 10% to 15% of 15-16-year-old can suffer from subclinical periodontitis [4,5]. Subclinical periodontitis corresponds to stage I periodontitis, according to the new classification of periodontal diseases [6]. The relationship between oral health and systemic diseases has been studied. There is an increased prevalence of certain systemic cardiovascular and autoimmune diseases among patients with periodontitis, notably diabetes mellitus is a risk factor for periodontitis [7-9].
Oral fluids (saliva, gingival crevicular fluid, mouth rinse) contains secretion of small and large salivary glands, large amounts of microbial metabolites and enzymes, host tissue and cell degradation products [10,11]. Analysis of oral fluid mirror the periodontal diseases very well [12-15]. It is possible to detect biomarkers for oral diseases within saliva and mouth rinse samples [12,15,16].
Matrix Metalloproteinases (MMPs) are a group of genetically distinct but structurally related proteolytic enzymes which increase significantly in various pathological inflammatory and malignant conditions. MMP-8 or collagenase-2 is a major collagenolytic protease in periodontitis affecting gingival tissues and oral fluids [10,17]. MMP-1 and MMP-13 are also found among periodontal tissue matrix [18]. Polymorphonuclear leukocytes (PMNs) upon degranulation, released collagenase-2, and especially its active form of MMP-8 (aMMP-8), has been shown to be a biomarker and a risk factor for periodontitis in both the adults [13,15] and the adolescents [4,14,19-23]. Periodontal treatment decreases the MMP-8 levels in oral fluids [15,19,24,25].
The aMMP-8 chairside mouth rinse test has shown to be useful in diagnostics, screening, predicting, treatment and follow-up of periodontal diseases [15,16,25-27]. Heikkinen AM et al., found promising results to predict first signs and even the genetic receptivity of early stage of periodontitis in adolescents [14,20-22]. This low-cost chairside Point-Of-Care (POC) lateral-flow immuno-test is practical, sensitive, specific, inexpensive, non-invasive and rapid. It never causes bacteremia differing from bleeding on probing [16,25]. The result is provided in 5 minutes and graded by eye as positive or negative. The test also functions quantitatively [25,28]. The test can differentiate healthy and gingivitis sites from periodontitis sites [24,29].
In adolescents, health behaviour such as eating habits, oral hygiene habits as well as smoking and snuff use, also impact oral diseases, such as periodontitis development and progression [4,19,23,30-33]. All pupils in eighth class in Finland are invited to an oral examination and prevention according to Government Act (380/2009) [34]. In the city of Hämeenlinna, these pupils visit oral hygienists, and if necessary, they forward the adolescent for further treatment to a dentist. Oral hygienist has targeted education in prevention.
The hypothesis of the present study was that aMMP-8 chairside mouth rinse test can identify and predict subclinical periodontitis in adolescents and monitor the effect of treatment. The aim was to study whether adolescents at risk for early stage of periodontitis could be identified using an aMMP-8 chairside mouth rinse test, and thus strengthen earlier studies. Furthermore, to study if health behaviour and oral health is linked to the test result in Finnish adolescents.
Materials and Methods
This study was carried out at the Hämeenlinna Health Center in South Finland in 2017-2018. All pupils in first, fifth and eighth class in Finland are invited to an oral examination according to Government Act. First and fifth class pupils were too young, so eighth class was selected. Eighth class adolescents (14-15-year-old) were compared to controls. It was assumed that in normal group, the prevalence of subclinical periodontitis is 15% and in test group 32%, p-value (Type I error) was set to 5%, and power 80%. Using these assumptions, sample size was N=94 in both groups. There were 211 eighth class pupils at school at Jukola area in Hämeenlinna (the whole birth cohort). Of them 21 were not invited to the examination because they had just visited the dentist or the oral hygienist. Thus, 190 adolescents were invited. Of them 65 did not come to the examination or we did not get consents to the study. Thus, 125 participants at Jukola school area gave their consents to the study. In Finland, consents are needed from adolescents and their parents if participants are under 15 years of age. Adolescents were randomly divided to control group (n=55, 27 girls and 28 boys) and test group (n=70, 29 girls and 41 boys). The participants were arranged in alphabetical order. Every second participant was picked up to the test group and every other to the control group.
This study was approved by the city of Hämeenlinna and by the Ethical Committee of the Helsinki and Uusimaa Hospital District (HUS 1770/2017). Altogether there were 125 participants who gave their consents for the study and mouth rinse analyses.
Chairside mouth rinse test for aMMP-8 was performed for the test group. The test has a diagnostic sensitivity and specificity of 76-83% and 96%, respectively [14,25,28]. In this study, sensitivity (PD≥2: 33.3%, PD≥3: 50.0%) and specificity (65.6%) for deepened periodontal pockets ≥4 mm were low because the study participants were young, and not many deepened periodontal pockets were found. They were at risk for subclinical periodontitis but without visible manifestations of illness.
Inclusion criteria: Eighth class pupils (aged 14-15-year-old) at Jukola school area.
Exclusion criteria: Lack of consent from adolescent or parents (one of them).
Participants were asked to fill a questionnaire which consisted of questions concerning oral hygiene habits, tobacco products, alcohol, drug and snuff use. Snacking habits were also asked but not reported in this study. Questionnaires [5] were sent together with appointment time so they were filled at home and were checked before examination.
Mouth rinse samples were analysed by method for chair-side diagnostic testing: The aMMP-8 specific lateral-flow POC/chair-side test (PerioSafe®, Dentognostics GmbH, Jena, Germany). Participants rinsed with tap water for 30 seconds and spat it out before waiting for one minute. They rinsed with 5 mL of the test solution for 30 seconds. This sample was split back to the specimen cup and sampled solution was taken with a syringe. Three drops of the sample solution were dropped to the test draw. The result was provided in five minutes and was graded as positive or negative was graded visually as positive or negative. One line means that the test is negative but successfully done and two lines, the test is positive. Cut-off point was 20 ng/mL [25]. Mouth rinse sampling and scoring of results was performed by oral hygienist. The results of test were recorded. Collected samples were frozen.
All patients were examined and findings were recorded. Information was collected of Decayed, Missed and Filled teeth (DMF), decayed teeth (D), initial caries (i) and the highest number and number of health sextants of Community Periodontal Index of Treatment Need (CPITN). CPITN consist of values: 0=healthy, 1=bleeding gingiva, 2=calculus, 3=periodontal pockets 4 mm-5 mm, 4=periodontal pockets ≥6 mm [35]. Probing Pocket Depth (PPD) was measured from six sites. Probing pockets deeper than 4 mm were registered. Bleeding On Probing (BOP) and Visible Plaque Index (VPI) were recorded along with Root Calculus (RC). Periodontal measurements were recorded at four sites of teeth. Adolescents on orthodontic treatment also took part in the study. In present study, 25 participants (20%) were in an active phase in orthodontic treatment (fixed or removable appliances).
The test group participants received intensified oral hygiene instructions. Oral hygienist showed the test result for motivation and informed about periodontal diseases. The intervention of the effect of tobacco products and alcohol use as well as counselling for teeth cleaning and snacking was also enhanced. Periodontal treatment involved scaling and professional cleaning. Follow-up time for test positives participants was four months. If found test positive after first follow-up session with prevention, the test was taken after four months again.
Statistical Analysis
Oral health habits, usage of tobacco products, alcohol and drugs were compared between the test and control groups, and between boys and girls by Fisher’s-Exact Test. Differences in periodontal parameters between the test and control groups and between the aMMP-8 mouth rinse test positives and negatives were tested using the Mann Whitney U test. The Friedman’s test was used for comparing the treatment effect in three points of time (Base, four months, eighth months). Pairwise post-hoc testing was calculated by the Dunn-Bonferroni test. The treatment effect among the participants with two visits (Base, four months) were tested by the Wilcoxon test. Data analysis was performed by IBM SPSS Statistics Version 25. Significance was considered for p<0.05 (2-sided).
Results
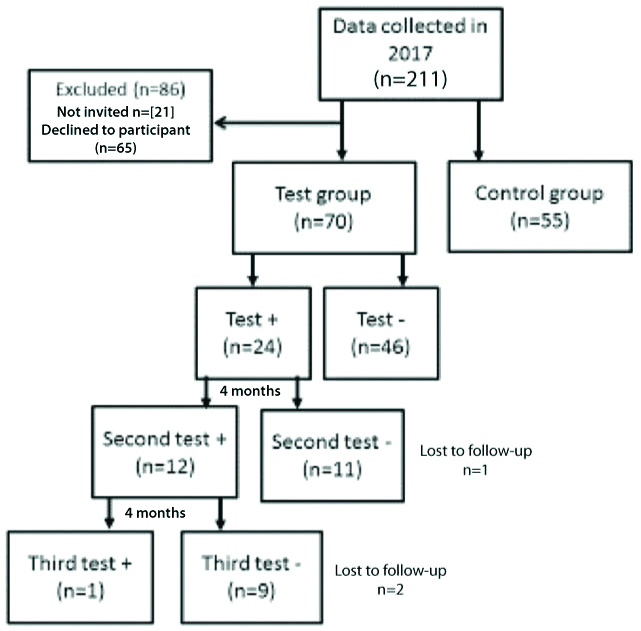
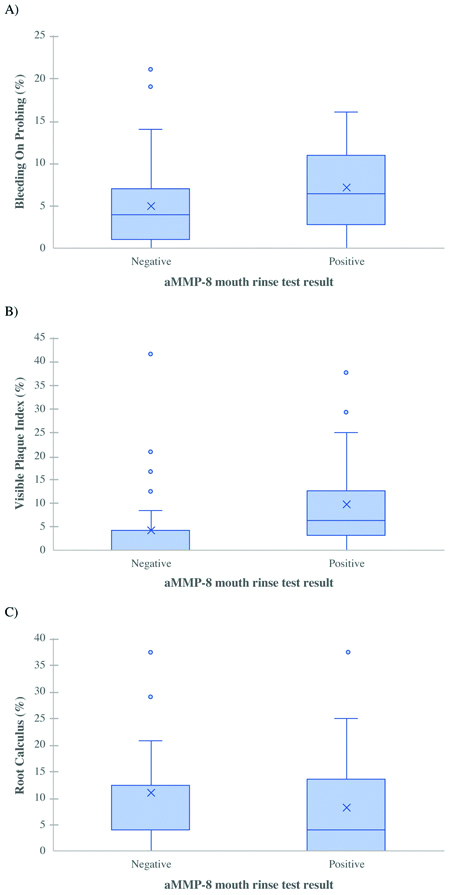
Of the 70 adolescents in test group, 24 were tested positive (34%) [Table/Fig-1]. Visible Plaque Index Percentage (VPI%) was significantly higher in test positives (p=0.005). Bleeding On Probing Percentage (BOP%) was also higher in test positives but not statistically significant (p=0.052). Root Calculus Percentage (RC%) did not differ significantly (p=0.131) [Table/Fig-2]. Deepened periodontal pockets did not differ significantly (p=0.895) between the groups.
Study profile of aMMP-8 chairside mouth rinse test results.
Box plots of mean a) Bleeding On Probing (BOP%), b) Visible Plaque Index (VPI%) and c) Root Calculus (RC%) Percentages among adolescents with positive or negative aMMP-8 chairside mouth rinse test results. The box plots denote the median, mean (x), quartiles, and extreme values.
Periodontal parameters between groups are shown in [Table/Fig-3]. Five adolescents in test group and two in control group had deepened periodontal pockets. Two in test group had one ≥4 mm deepened periodontal pocket and one had two ≥4 mm deepened periodontal pockets. Two in test group as well as in control group had three or more ≥4 mm deepened periodontal pockets. Of them in test group two had a positive and three a negative test outcome.
| Test group | Control group | |
|---|
| n | Min | Max | Median (IQR) | Missing (n) | n | Min | Max | Median (IQR) | Missing (n) | p-value |
|---|
| BOP % | 69 | 0 | 21 | 3.57 (1.79-10.27) | 1 | 55 | 0 | 100 | 14.29 (4.46-25.00) | 0 | <0.001 |
| VPI % | 69 | 0 | 41.67 | 4.17 (0.00-8.33) | 1 | 55 | 0 | 100 | 8.33 (0.00-20.83) | 0 | 0.062 |
| RC % | 69 | 0 | 37.50 | 12.50 (0.00-12.50) | 1 | 55 | 0 | 100 | 12.50 (0.00-16.67) | 0 | 0.801 |
| PPD | 69 | 0 | 3 | 0 (0) | 1 | 55 | 0 | 6 | 0 (0) | 0 | 0.461 |
| CPITN max | 68 | 0 | 3 | 2 (1-2) | 2 | 53 | 0 | 3 | 2 (1-2) | 2 | 0.188 |
IQR: Interquartile range; BOP%: Bleeding On Probing; VPI%: Visible Plaque Index; RC%: Root Calculus Percentages. PPD: Number of at least 4 mm deepened periodontal pockets. CPITN max: patient’s highest CPITN score in six sextants; p-value: Mann Whitney U test (2-sided).
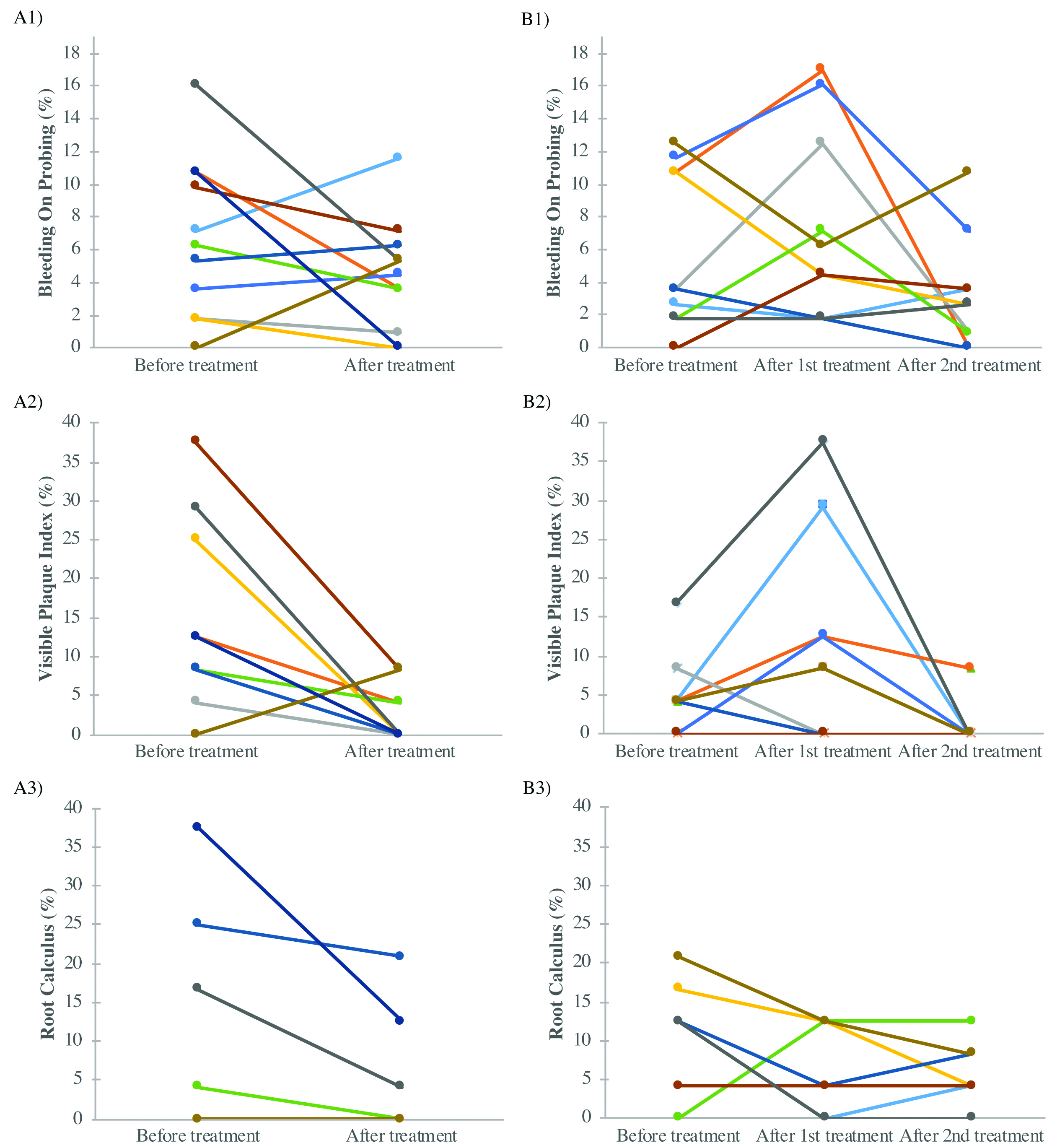
Altogether 11 of the 24 (46%) positive tested had one treatment period and 9 (38%) two treatment periods before their test result turned negative. Three adolescents skipped oral hygienist visits after examination. Only one patient was test positive after two treatment periods. The effect of treatment in BOP, VPI and RC Percentages are shown in [Table/Fig-4]. Patients that had only one visit to oral hygienist had significantly lower levels of VPI and RC after the treatment period (p=0.011 and 0.031, respectively). Likewise, VPI and RC levels were lower among two visit patients after their treatment was finished, but not statistically significantly. Finally, BOP levels were also reduced, but not significantly, in both groups (one and two visits). Of participants 25 (15 in test group and 10 in control group) were in active orthodontic treatment (fixed or removable appliances) during this study. Of the test group five of them were test positives but changed to negative during periodontal treatment.
The effect of treatment on Bleeding On Probing (BOP%), Visible Plaque Index (VPI%) and Root Calculus (RC%) Percentages related to the aMMP-8 chairside test outcomes (±) before and after a) one or b) two oral hygienist intervention treatment period.
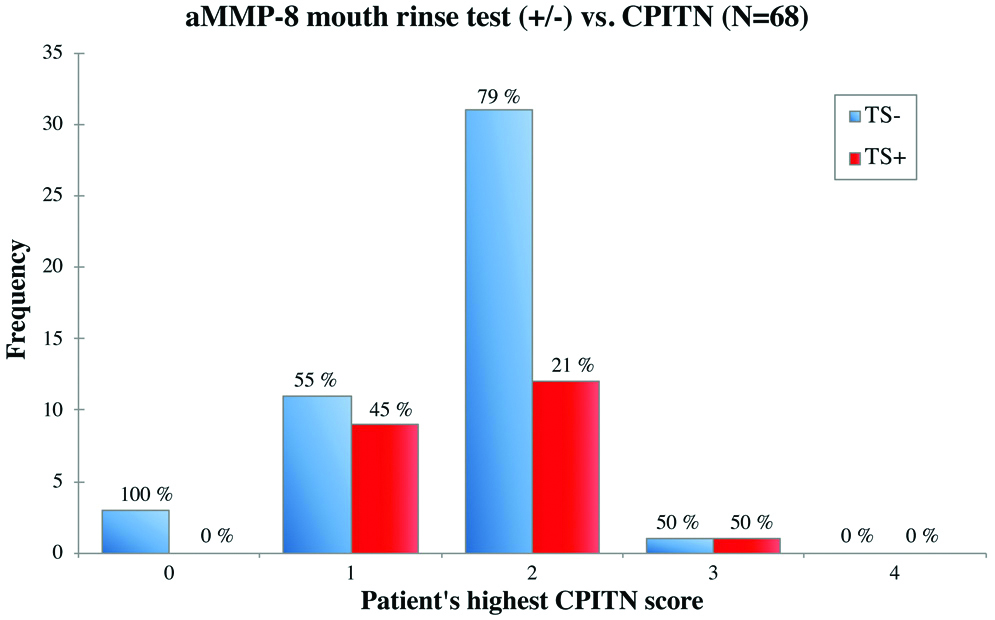
One to two carious lesions were recorded in 18.4% of the participants, 73.6% did not have any. DMF score was 0 in 48.0% of adolescents. CPITN was mostly 1 to 2 (88.8%). Girls had significantly more healthy sextants than boys (p=0.001) instead there were no significant difference between test or control group nor between test positives or test negatives. Highest CPITN score did not differ between test positives or test negatives (p=0.278) [Table/Fig-5]. Girls brushed their teeth significantly more often than boys (p=0.002). Interdental spaces were cleaned quite random.
The aMMP-8 chairside mouth rinse test results according to adolescents’ highest CPITN score found in six sextants. TS−=negative aMMP-8 mouth rinse test result, TS+ =positive aMMP-8 mouth rinse test result, CPITN=Community Periodontal Index of Treatment Needs. Missing n=2.
Of all participants, most were non-smokers, 90.0% in test group and 87.3% in control group. No one smoked electro-tobacco, seven had experimented it. In test group 88.6% and in control group 87.3% did not drink alcohol. Only one girl was snuff-user in test group. No one used drugs.
Discussion
In this study, aMMP-8 test could find adolescents with risk for subclinical periodontitis and with poor oral hygiene. This is in line with previous studies among adolescents predisposed to early stage of periodontitis by study group of Heikkinen [14,21-23]. Nwhator SO et al., found a very strong correlation between aMMP-8 test and oral hygiene index among Nigerian adult males [13]. Räisänen IT et al., showed that the test had stronger association with or alarmed more precisely subclinical periodontitis than bleeding on probing [16]. It has been recently shown that childhood oral infections are associated with and eventually may even predict the subclinical carotid atherosclerosis in adulthood [36]. Regarding this article Umeizudike K et al., and Merchant AT and Virani SS additionally pointed that the main oral problem may, in fact, be the poor oral health behaviour rather than oral infections or periodontal diseases in this cohort [37,38]. As in the present study, they both pointed the importance of enough early diagnosis and preventive intervention for the adolescents with the early signs of periodontal oral diseases.
Periodontitis has been associated with elevation of aMMP-8 in oral fluids [15,39]. Nearly half of the participants in the test group were positive (aMMP-8 >20 ng/mL). The elevated amount is alarming but is in line with studies by Heikkinen AM et al., [14]. In the present study, oral health prevention intervention (oral health habits and oral health care instructions) and periodontal treatment decreased aMMP-8 levels as monitored by changes in test stick results from positive to negative during follow-up time. By intervention, plaque accumulation and bleeding reduced at the same time as test result turned negative. The reduction of aMMP-8 as a consequence of intervention has also been demonstrated in other studies with this test [15,19,24,25]. The aMMP-8 test had no false positives when related to CPITN. A positive aMMP-8 test result occurred only if adolescents were in need of treatment (CPITN=1, 2 or 3). Only seven patients had deepened periodontal pockets (≥4 mm). So, there was just a few with visible or detectable signs of periodontitis. Thus, aMMP-8 test is useful for monitoring as well as following the effect of preventive interventions and treatment of subclinical periodontitis [40].
Most of adolescents brushed their teeth twice a day. Same outcome has been found with Spanish adolescents [41]. Tooth brushing score is often higher for girls [4,14,41,42]. Bacterial dental plaque is considered to be the major risk factor for the development of periodontal oral diseases [10,17]. Heikkinen AM et al., suggested that the main risk factor for subclinical periodontitis in adolescents is the partly calcified, dysbiotic bacterial biofilm, which inductively can interact with the immune defences of the host [23]. Using tobacco products and alcohol consumption was of minor importance in the present study, in this age-cohort, although alcohol consumption seems to be common among European adolescents [43] as is smoking, too [44].
Ongoing orthodontic treatment may complicate the result causing false positive results. Orthodontic force can increase the levels of aMMP-8 in oral fluids after fixed appliance treatment [45,46]. All test positives in active orthodontics phase turned negative during periodontal treatment so we did not interpret them as false positives.
More attention should be paid to oral health prevention and early diagnostic and treatment of periodontitis because its treatment by specialists is expensive especially in respect of national healthcare economics. Its divination would save money of the whole society. Young risk patients with periodontal inflammation could be recognised even earlier so that prevention and early treatment can be focused and timed enough early before subclinical periodontitis by the aMMP-8 chairside mouth rinse test. The aMMP-8 test may even be used also by physicians to detect periodontitis [47]. Socioeconomic status may have an impact on adolescents’ life activity [48]. The strength of this study is an exact oral health examination and a whole age cohort adolescent group to be in focus.
Limitation(s)
As a limitation of this study, the sample size was quite small. In Finland we need permission from adolescents and their parents which is a challenge. Additional limitation is that we did not ask any questions of family socioeconomic status.
Conclusion(s)
The aMMP-8 chairside mouth rinse test exerts potential to identify and alarm adolescents with poor oral hygiene at risk for subclinical periodontitis without visible manifestations of illness, such as deepened periodontal pockets. Thus, young risk patients could be recognised for preventive intervention and the test negativity followed by a MMP-8 chairside mouth rinse test. However, further studies are needed with longer follow-up time and larger sample of adolescents.
IQR: Interquartile range; BOP%: Bleeding On Probing; VPI%: Visible Plaque Index; RC%: Root Calculus Percentages. PPD: Number of at least 4 mm deepened periodontal pockets. CPITN max: patient’s highest CPITN score in six sextants; p-value: Mann Whitney U test (2-sided).
[1]. Ramseier CA, Anerud A, Dulac M, Lulic M, Cullinan MP, Seymour GJ, Natural history of periodontitis: Disease progression and tooth loss over 40 yearsJ Clin Periodontol 2017 44(12):1182-91.10.1111/jcpe.1278228733997 [Google Scholar] [CrossRef] [PubMed]
[2]. Burt B, Research, Science and Therapy Committee of the American Academy of Periodontology. Position paper: epidemiology of periodontal diseasesJ Periodontol 2005 76(8):1406-19.10.1902/jop.2005.76.8.140616101377 [Google Scholar] [CrossRef] [PubMed]
[3]. Kassebaum NJ, Bernabe E, Dahiya M, Bhandari B, Murray CJL, Marcenes W, Global burden of severe periodontitis in 1990-2010: A systematic review and meta-regressionJ Dent Res 2014 93(11):1045-53.10.1177/002203451455249125261053 [Google Scholar] [CrossRef] [PubMed]
[4]. Heikkinen AM, Pajukanta R, Pitkäniemi J, Broms U, Sorsa T, Koskenvuo M, The effect of smoking on periodontal health of 15- to 16-year-old adolescentsJ Periodontol 2008 79(11):2042-47.10.1902/jop.2008.08020518980511 [Google Scholar] [CrossRef] [PubMed]
[5]. Heikkinen AM. Oral health, smoking and adolescence. University of Helsinki, Faculty of Medicine, Institute of Dentistry. 2011. Available from: http://urn.fi/ URN:ISBN:978-952-10-7250-55 [Google Scholar]
[6]. Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS, A new classification scheme for periodontal and peri-implant diseases and conditions- Introduction and key changes from the 1999 classificationJ Clin Periodontol 2018 45(Suppl 20):S1-S8./10.1111/jcpe.1293529926489 [Google Scholar] [CrossRef] [PubMed]
[7]. Nesse W, Dijkstra PU, Abbas F, Spijkervet FK, Stijger A, Tromp JA, Increased prevalence of cardiovascular and autoimmune diseases in periodontitis patients: a cross-sectional studyJ Periodontol 2010 81(11):1622-28.10.1902/jop.2010.10005820583916 [Google Scholar] [CrossRef] [PubMed]
[8]. Lalla E, Papapanou PN, Diabetes mellitus and periodontitis: a tale of two common interrelated diseasesNat Rev Endocrinol 2011 7(12):738-48.10.1038/nrendo.2011.10621709707 [Google Scholar] [CrossRef] [PubMed]
[9]. Liccardo D, Cannavo A, Spagnuolo G, Ferrara N, Cittadini A, Rengo C, Periodontal disease: A risk factor for diabetes and cardiovascular diseaseInt J Mol Sci 2019 20(6):pii:E141410.3390/ijms2006141430897827 [Google Scholar] [CrossRef] [PubMed]
[10]. Sorsa T, Tjäderhane L, Salo T, Matrix metalloproteinases (MMPs) in oral diseasesOral Dis 2004 10(6):311-18.10.1111/j.1601-0825.2004.01038.x15533204 [Google Scholar] [CrossRef] [PubMed]
[11]. Boelen GJ, Boute L, d’Hoop J, EzEldeen M, Lambrichts I, Opdenakker G, Matrix metalloproteinases and inhibitors in dentistryClin Oral Investiq 2019 23(7):2823-35.10.1007/s00784-019-02915-y31093743 [Google Scholar] [CrossRef] [PubMed]
[12]. Rathnayake N, Akerman S, Klinge B, Lundegren N, Jansson H, Tryselius Y, Salivary biomarkers of oral health: a cross-sectional studyJ Clin Periodontol 2013 40(2):140-47.10.1111/jcpe.1203823174014 [Google Scholar] [CrossRef] [PubMed]
[13]. Nwhator SO, Ayanbadejo PO, Umeizudike KA, Opeodu OI, Agbelusi GA, Olamijulo JA, Clinical correlates of a lateral-flow immunoassay oral risk indicatorJ Periodontol 2014 85(1):188-94.23600996 [Google Scholar] [PubMed]
[14]. Heikkinen AM, Nwhator SO, Rathnayake N, Mäntylä P, Vatanen P, Sorsa T, Pilot study on oral health status as assessed by an active matrix metalloproteinase-8 chairside mouthrinse test in adolescentsJ Periodontol 2016 87(1):36-40.10.1902/jop.2015.15037726430926 [Google Scholar] [CrossRef] [PubMed]
[15]. Sorsa T, Gursoy UK, Nwhator S, Hernández M, Tervahartiala T, Leppilahti J, Analysis of matrix metalloproteinases, especially MMP-8, in gingival crevicular fluid, mouthrinse and saliva for monitoring periodontal diseasesPeriodontol 2000 2016 70(1):142-63.10.1111/prd.1210126662488 [Google Scholar] [CrossRef] [PubMed]
[16]. Räisänen IT, Sorsa T, van der Schoor GJ, Tervahartiala T, van der Schoor P, Gieselmann DR, Active matrix metalloproteinase-8 point of care (PoC)/chairside mouthrinse test vs. bleeding on probing in diagnosing subclinical periodontitis in adolescentsDiagnostics (Basel) 2019 9(1):3410.3390/diagnostics901003430909530 [Google Scholar] [CrossRef] [PubMed]
[17]. Sorsa T, Tjäderhane L, Konttinen YT, Lauhio A, Salo T, Lee HM, Matrix metalloproteinases: Contribution to pathogenesis, diagnosis and treatment of periodontal inflammationAnn Med 2006 38(5):306-21.10.1080/0785389060080010316938801 [Google Scholar] [CrossRef] [PubMed]
[18]. Gonçalves PF, Huang H, McAninley S, Alfant B, Harrison P, Aukhil I, Periodonal treatment reduces matrix metalloproteinase levels in localized aggressive periodontitisJ Periodontol 2013 84(12):1801-08.10.1902/jop.2013.13000223537121 [Google Scholar] [CrossRef] [PubMed]
[19]. Heikkinen AM, Sorsa T, Pitkäniemi J, Tervahartiala T, Kari K, Broms U, Smoking Affects Diagnostic Salivary Periodontal Disease Biomarker Levels in AdolescentsJ Periodontol 2010 9:1299-307.10.1902/jop.2010.09060820450405 [Google Scholar] [CrossRef] [PubMed]
[20]. Heikkinen AM, Kettunen K, Kovanen L, Haukka J, Elg J, Husu H, Inflammatory mediator polymorphisms associate with initial periodontitis in adolescentsClin Exp Dent Res 2016 2(3):208-15.10.1002/cre2.4029744169 [Google Scholar] [CrossRef] [PubMed]
[21]. Heikkinen AM, Raivisto T, Kettunen K, Kovanen L, Haukka J, Esmaeili EP, Pilot Study on the Genetic Background of an Active Matrix Metalloproteinase-8 Test in Finnish AdolescentsJ Periodontol 2017 88(5):464-72.10.1902/jop.2016.16044127989222 [Google Scholar] [CrossRef] [PubMed]
[22]. Heikkinen AM, Pakpaznejad Esmaeili E, Kovanen L, Ruokonen H, Kettunen K, Haukka J, Periodontal initial radiological findings of genetically predisposed finnish adolescentsJ Clin Diagn Res 2017 11(7):ZC25-28.10.7860/JCDR/2017/25850.1016828893037 [Google Scholar] [CrossRef] [PubMed]
[23]. Heikkinen AM, Räisänen IT, Tervahartiala T, Sorsa T, Cross-sectional analysis of risk factors for subclinical periodontitis; active matrix metalloproteinase-8 as a potential indicator in initial periodontitis in adolescentsJ Periodontol 2019 90(5):484-92.10.1002/JPER.18-045030397915 [Google Scholar] [CrossRef] [PubMed]
[24]. Mäntylä P, Stenman M, Kinane DF, Tikanoja S, Luoto H, Salo T, Gingival crevicular fluid collagenase-2 (MMP-8) test stick for chair-side monitoring of periodontitisJ Periodont Res 2003 38(4):436-39.10.1034/j.1600-0765.2003.00677.x12828663 [Google Scholar] [CrossRef] [PubMed]
[25]. Alassiri S, Parnanen P, Rathnayake N, Johannsen G, Heikkinen AM, Lazzara R, The Ability of Quantitative, Specific, and Sensitive Point-of-Care/Chairside Oral Fluid Immunotests for aMMP-8 to Detect Periodontal and Peri-Implant DiseasesDis Markers 2018 2018:130639610.1155/2018/130639630154936 [Google Scholar] [CrossRef] [PubMed]
[26]. Leppilahti JM, Harjunmaa U, Järnstedt J, Mangani C, Hernández M, Tervahartiala T, Diagnosis of newly delivered mothers for periodontitis with a novel oral rinse aMMP-8 Point-of-Care test in a rural Malawian populationDiagnostics (Basel) 2018 8(3):E6710.3390/diagnostics803006730223547 [Google Scholar] [CrossRef] [PubMed]
[27]. Räisänen IT, Heikkinen AM, Siren E, Tervahartiala T, Gieselmann DR, van der Schoor GJ, Point-of Care/Chairside aMMP-8 analytics of periodontal diseases’ activity and episodic progressionDiagnostics (Basel) 2018 8(4):E7410.3390/diagnostics804007430360358 [Google Scholar] [CrossRef] [PubMed]
[28]. Sorsa T, Gieselmann D, Arweiler NB, Hernández M, A quantitative point-of-care test for periodontal and dental peri-implant diseasesNat Rev Dis Primers 2017 3:1706910.1038/nrdp.2017.6928905941 [Google Scholar] [CrossRef] [PubMed]
[29]. Al-Majid A, Alassiri S, Rathnayake N, Tervahartiala T, Gieselmann DR, Sorsa T, Matrix Metalloproteinase-8 as an Inflammatory and Prevention Biomarker in Periodontal and Peri-Implant DiseasesInt J Dent 2018 2018:789132310.1155/2018/789132330305812 [Google Scholar] [CrossRef] [PubMed]
[30]. Kumar S, Tadakamadla J, Johnson NW, Effect of toothbrushing frequency on incidence and increment of dental caries: A systematic review and meta AnalysisJ Dent Res 2016 95(11):1230-36.10.1177/002203451665531527334438 [Google Scholar] [CrossRef] [PubMed]
[31]. Mäntylä P, Stenman M, Kinane DF, Salo T, Suomalainen K, Tikanoja S, Monitoring periodontal disease status in smokers and nonsmokers using a gingival crevicular fluid matrix metalloproteinase-8-specific chars-side testJ Periodont Res 2006 41(6):503-12.10.1111/j.1600-0765.2006.00897.x17076774 [Google Scholar] [CrossRef] [PubMed]
[32]. Johannsen A, Susin C, Gustafsson A, Smoking and inflammation: evidence for a synergistic role in chronic diseasePeriodontol 2000 2014 64(1):111-26.10.1111/j.1600-0757.2012.00456.x24320959 [Google Scholar] [CrossRef] [PubMed]
[33]. Leite FRM, Nascimento GG, Scheutz F, López R, Effect of smoking on periodontitis: a systematic review and meta-regressionAm J Prev Med 2018 54(6):831-41.10.1016/j.amepre.2018.02.01429656920 [Google Scholar] [CrossRef] [PubMed]
[34]. Government Decree (380/2009) on maternity and child welfare clinics, school and student health care and preventive oral health care for children and young people. https://www.finlex.fi/fi/laki/alkup/2011/20110338 [Google Scholar]
[35]. Ainamo J, Bay I, Problems and proposals for recording gingivitis and plaqueInt Dent J 1975 25(4):229-35. [Google Scholar]
[36]. Pussinen PJ, Paju S, Koponen J, Viikari JSA, Taittonen L, Laitinen T, Association of childhood oral infections with cardiovascular risk factors and subclinical atherosclerosis in adulthoodJAMA Netw Open 2019 2(4):e19252310.1001/jamanetworkopen.2019.252331026022 [Google Scholar] [CrossRef] [PubMed]
[37]. Umeizudike K, Nwhator S, Heikkinen AM, Sorsa T, Comment on article “Association of Childhood Oral Infections with Cardiovascular Risk Factors and Subclinical Atherosclerosis in Adulthood”JAMA Netw Open 2019 2(4):e192523(May 11,2019)10.1001/jamanetworkopen.2019.252331026022 [Google Scholar] [CrossRef] [PubMed]
[38]. Merchant AT, Virani SS, Childhood Oral Infections and Subclinical Atherosclerosis in Adulthood: Should We Wait for Causality or Just Treat? JAMA Netw Open 2019 2(4):e19248910.1001/jamanetworkopen.2019.248931026019 [Google Scholar] [CrossRef] [PubMed]
[39]. Majeed ZN, Philip K, Alabsi AM, Pushparajan S, Swaminathan D, Identification of gingival crevicular fluid sampling, Analytical methods, and oral biomarkers for the diagnosis and monitoring of periodontal diseases: A systemic review. Hindawi Publishing CorporationDis Markers 2016 2016:180472710.1155/2016/180472728074077 [Google Scholar] [CrossRef] [PubMed]
[40]. Sorsa T, Tervahartiala T, Leppilahti J, Hernandez M, Gamonal J, Tuomainen AM, Collagenase-2 (MMP-8) as a point-of-care biomarker in periodontitis and cardiovascular diseases. Therapeutic response to non-antimicrobial properties of tetracyclinesPharmacol Res 2011 63(2):108-13.10.1016/j.phrs.2010.10.00520937384 [Google Scholar] [CrossRef] [PubMed]
[41]. Costa-Tutusaus L, Guerra-Balic M, Relationship between healthy lifestyle and sociodemographic factors in adolescents in Catalonia: Application of VISATEEN questionnairePLoS One 2016 11(9):e016338110.1371/journal.pone.016338127684476 [Google Scholar] [CrossRef] [PubMed]
[42]. Maes L, Vereecken C, Vanobbergen J, Honkala S, Tooth brushing and social characteristics of families in 32 countriesInt Dent J 2006 56(3):159-67.10.1111/j.1875-595X.2006.tb00089.x16826883 [Google Scholar] [CrossRef] [PubMed]
[43]. Samuelson G, Dietary habits and nutritional status in adolescents over Europe. An overview of current studies in the Nordic countriesEur J Clin Nutr 2000 1:S21-S28.10.1038/sj.ejcn.160098010805034 [Google Scholar] [CrossRef] [PubMed]
[44]. Banzer R, Haring C, Buchheim A, Oehler S, Carli V, Wasserman C, Factors associated with different smoking status in European adolescents: Results of the SEYLE studyEur Child Adolesc Psychiatry 2017 26(11):1319-29.10.1007/s00787-017-0980-428386649 [Google Scholar] [CrossRef] [PubMed]
[45]. Apajalahti S, Sorsa T, Railavos S, Ingman T, The in vivo levels of matrix metalloproteinase-1 and -8 in gingival crevicular fluid during initial orthodontic tooth movementJ Dent Res 2003 82(12):1018-22.10.1177/15440591030820121614630906 [Google Scholar] [CrossRef] [PubMed]
[46]. Ingman T, Apajalahti S, Mäntylä P, Savolainen P, Sorsa T, Matrix metalloproteinase-1 and -8 in gingival crevicular fluid during orthodontic tooth movement: a pilot study during 1 month of follow-up after fixed appliance activationEur J Orthod 2005 27(2):202-07.10.1093/ejo/cjh09715817630 [Google Scholar] [CrossRef] [PubMed]
[47]. Borujeni SI, Mayer M, Eickholz P, Activated matrix metalloproteinase-8 in saliva as diagnostic test for periodontal disease? A case-control studyMed Microbiol Immunol 2015 204(6):665-72.10.1007/s00430-015-0413-225841875 [Google Scholar] [CrossRef] [PubMed]
[48]. Telama R, Laakso L, Nupponen H, Rimpelä A, Pere L, Secular trends in youth physical activity and parents’ socioeconomic status from 1977 to 2005Pediatr Exerc Sci 2009 21(4):462-74.10.1123/pes.21.4.46220128365 [Google Scholar] [CrossRef] [PubMed]