Klinefelter Syndrome Complicated with Diabetes Mellitus, Hypothyroidism and Cryptorchidism: Case Report and Literature Review
Wei Zhu1, Shiliang Wang2, Shaogang Ma3, Liuxue Yang4, Yali Qiu5
1 Department of Internal Medicine, Caiji Town Hospital, No. 1 Suwang Road, Suqian 223800, Jiangsu Province, China.
2 Department of Internal Medicine, Caiji Town Hospital, No. 1 Suwang Road, Suqian 223800, Jiangsu Province, China.
3 Department of Endocrinology and Metabolism, Suqian First Hospital, No. 120 Suzhi Road, Suqian 223800, Jiangsu Province, China.
4 Department of Endocrinology and Metabolism, the Second Affiliated Hospital of Guilin Medical University, No. 212 Renmin Road, Lingui District, Guilin, Guangxi Zhuang Autonomous Region, China.
5 Department of Neonatal Screening and Care, Women and Children’s Hospital of Suqian, No. 9 Ping’an Road, Suqian 223800, Jiangsu Province, China.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shaogang Ma, Department of Endocrinology and Metabolism, Suqian First Hospital, No. 120 Suzhi Road, Suqian City-223800, Jiangsu Province, China.
E-mail: mashaogang@163.com
Klinefelter Syndrome (KS) remains underdiagnosed due to its complex clinical presentation. Here, the authors present the case of a 48-year-old of KS complicated with Type 2 Diabetes Mellitus (DM), hypothyroidism and cryptorchidism as well as perform a literature review. The patient first visited the hospital for diabetes. Male sexual characteristics were missing, complicated with cryptorchidism. Laboratory and chromosome tests were performed to confirm the diagnosis. The patient demonstrated low testosterone and high gonadotropin levels, with the karyotype of 47, XXY. Thus, for diabetes patients who lack male sexual characteristics, gonadal function and chromosome-related examinations should be performed for analysis and differential diagnosis. Based on existing data, there is a pressing need to generate better evidence for KS early diagnosis and comprehensive treatment.
Analysis, Complication, Sex chromosome
Case Report
A 48-year-old male patient came with a chief complaint of vision loss and blurred vision without obvious cause for two months. The patient was diagnosed with Type 2 diabetes three years earlier. He was on medication with oral gliclazide and metformin tablets. The patient had no history of diplopia, double vision, dizziness or headache. The parents of the patient too had a history of diabetes. Bilateral testicles were not observed since childhood. The patient had little body hair during puberty and had no beard. The patient could not perform a normal sex life while he was married and subsequently got divorced.
Physical examination at admission revealed the blood pressure was 130/86 mmHg, height was 170 cm, weight was 65 kg, and Body Mass Index (BMI) was 22.49. He had equal length of height and fingertip-to-fingertip distance, smooth and delicate skin, no beard and axillary hair, sparse pubic hair, small Adam’s apple, and a high voice. His neck was symmetrical, the thyroid was not enlarged and the heart and both lungs were normal. The liver and spleen were not enlarged. Bilateral testicles were not palpated, while 1.5 cm × 0.5 cm and 2.0 cm × 0.5 cm masses were found in the left and right groin areas, respectively, with a medium texture, smooth edge, low movability, and no tenderness. The penis was short, and the scrotum was small with thin skin. The bony abnormality, personality or behaviour wasn’t observed.
Biochemical tests revealed that his blood glucose level was poorly controlled. Glycated haemoglobin A1c (HbA1c) levels were measured using an HbA1c meter from Bio-Rad Laboratories, Ltd., (Shanghai, China). Levels of HbA1c were 11.9%, fasting blood glucose was 9.17 mmol/L, 2 hour postprandial blood glucose was 14.50 mmol/L by glucose oxidase method. The level of haemoglobin was 96.00 g/L, urine microalbumin was 328.00 mg/L. Levels of liver and kidney function, blood lipids and electrolytes were normal.
Related hormones of the case are shown in [Table/Fig-1]. He had normal level of parathyroid hormone. Levels of TSH were slightly elevated and free triiodothyronine was slightly declined. The antibodies of thyroid peroxidase and thyroglobulin were negative. However, he had very low level of testosterone and largely elevated levels of follicle-stimulating hormone and luteinizing hormone.
Demonstration of the related hormones when diagnosed.
| Variables | Normal range | Results |
|---|
| Parathyroid hormone | 15.00-65.00 pg/L | 38.24 |
| Thyrotropin | 0.27-4.20 mIU/L | 5.24 |
| Free thyroxine | 12.00-22.00 pmol/L | 14.74 |
| Free triiodothyronine | 3.10-6.80 pmol/L | 3.09 |
| Testosterone | 8.64-29.00 nmol/L | 0.45 |
| Prolactin | 86.00-324.00 mIU/L | 177.3 |
| Follicle-stimulating hormone | 1.50-12.40 IU/L | 51.31 |
| Luteinizing hormone | 1.70-8.60 IU/L | 23.58 |
| Estradiol | 28.00-156.00 pmol/L | 82.88 |
| Progesterone | 0.16-0.50 nmol/L | 0.64 |
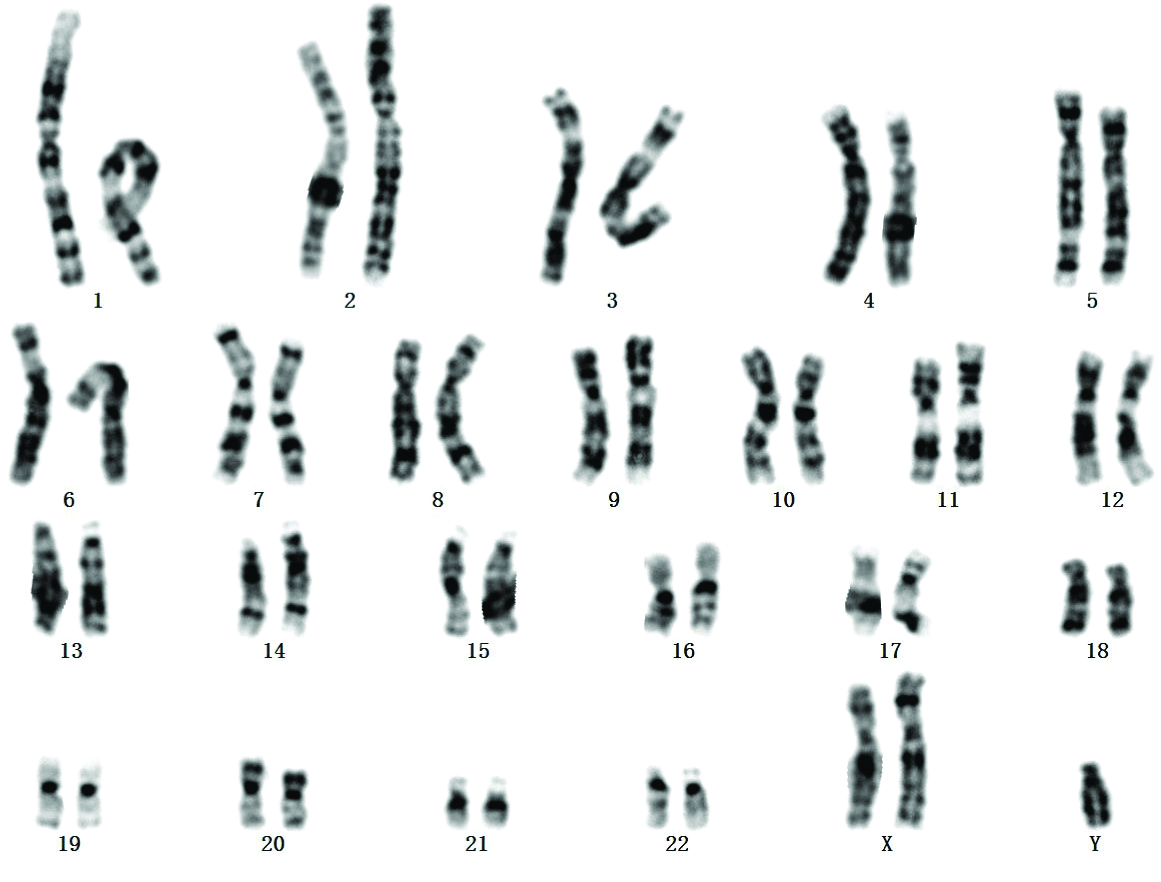
Colour Doppler ultrasound showed no testicular echo in the bilateral scrotum, and a 12.6 mm × 5.5 mm testicle-like echo was detected in the left groin area, with a thickened and unevenly distributed internal parenchymal echo and sparse blood flow signal; an 18.0 mm × 7.0 mm testicle-like echo was detected in the right groin area, with a thickened and unevenly distributed internal parenchymal echo and sparse blood flow signal; no abnormality was detected in the thyroid ultrasound. And more importantly, karyotype analysis showed 47, XXY pattern [Table/Fig-2].
Karyotype analysis of the patient shows the 47, XXY pattern.
The patient was treated with recombinant insulin glargine, 14 U subcutaneous injected Qd; metformin sustained-release tablet, 0.5 TID; acarbose, 50 mg chewed with the first bite of the meal TID; and testosterone undecanoate soft capsule, 40 mg BID. The patient refused surgery to correct cryptorchidism. After six months of follow-up, his blood glucose control gradually improved. Levels of HbA1c were 6.9%, fasting blood glucose was 6.17 mmol/L, 2 hour postprandial blood glucose was 6.50 mmol/L. The patient felt good and was more motivated to learn and work.
Discussion
The most common karyotype of KS is 47, XXY. The incidence in newborn male infants is 0.1% to 0.2%, and the incidence in infertile patients is 10% to 15%. Most patients are diagnosed when they are assessed for infertility or male breast development [1,2]. According to a karyotype analysis of 44 cases of KS, the classical 47 XXY karyotype was detected in 38 (86.4%) subjects and 6 (13.6%) had karyotype consistent with Klinefelter variants [3]. Therefore, extensive cytogenetic diagnostic analysis can accurately detect KS, which is of great significance for the diagnosis of clinical diseases.
The preferred treatment is male hormone replacement to promote the development of secondary sexual characteristics and recovery of sexual function. Infertility is currently a problem that is difficult to solve [4]. KS is prone to complications with other diseases, for example, the incidence of diabetes is as high as 15% to 50% [5]. The index case was KS complicated with diabetes; the patient’s HbA1c level was as high as 11.9%, indicating very poor blood glucose control. Insulin therapy or basal insulin combined with oral hypoglycemic agents should be administered in a timely manner, and treatment efficacy should be determined at regular follow-ups. The incidence of diabetes in these patients is high, and thus, these patients often visit the endocrinologists due to prevailing diabetes. Patients with KS may be prone to abnormal glucose metabolism because of age, low testosterone level, high follicle stimulating hormone level, high oestrogen/testosterone ratio, insulin resistance, and abnormal number of X chromosomes [6].
It has been reported that in addition to diabetes, this disease may also be complicated with hypothyroidism, although with a low probability [7], and may also be complicated with lupus encephalitis and retroperitoneal teratoma [8]. This patient was complicated with mild hypothyroidism. Autoimmune hypothyroidism was excluded. The etiological mechanism of hypothyroidism in the patient was unknown but may have been caused by hypoplasia of the thyroid gland itself or by congenital defects of the pituitary-thyroid axis. The clinical pathological features of hypothyroidism were not specific, which may be due to the relatively mild hypothyroidism symptoms.
The clinical situation of this patient was relatively complicated because, in addition to diabetes and hypothyroidism, the patient also had bilateral cryptorchidism, which led to further reduced testosterone levels. Therefore, cryptorchidism should be appropriately managed to prevent malignant transformation. However, the issue of infertility is more difficult to address. According to literature reports, KS combined with cryptorchidism or hypospadias is not uncommon [9]. These observations indicate that clinicians should pay attention to birth management and perform comprehensive and detailed physical examinations of newborn male infants to screen, diagnose, and treat this disease at an early stage.
Conclusion(s)
Through the analysis of this case, the present authors recognise the importance of the differential diagnosis of special types of diabetes, the complexity of KS, and the urgency of comprehensive treatment of various endocrine diseases.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 05, 2019
Manual Googling: Dec 17, 2019
iThenticate Software: Dec 30, 2019 (11%)
[1]. Chang S, Skakkebæk A, Gravholt CH, Klinefelter Syndrome and medical treatment: hypogonadism and beyondHormones (Athens) 2015 14(4):531-48.10.14310/horm.2002.162226732150 [Google Scholar] [CrossRef] [PubMed]
[2]. Asirvatham AR, Pavithran PV, Pankaj A, Bhavani N, Menon U, Menon A, Klinefelter syndrome: clinical spectrum based on 44 consecutive cases from a south Indian tertiary care centerIndian J Endocrinol Metab 2019 23(2):263-67.10.4103/ijem.IJEM_582_1831161115 [Google Scholar] [CrossRef] [PubMed]
[3]. Wei L, Liu Y, Sun S, Tang Y, Chen S, Song G, Case report of 49,XXXXY syndrome with cleft palate, diabetes, hypothyroidism, and cataractsMedicine (Baltimore) 2019 98(39):e1734210.1097/MD.000000000001734231574874 [Google Scholar] [CrossRef] [PubMed]
[4]. Høst C, Bojesen A, Erlandsen M, Groth KA, Kritstensen K, Jurik AG, A placebo-controlled randomized study with testosterone in Klinefelter syndrome-beneficial effects on body compositionEndocr Connect 2019 Aug 1 [Epubahead of print]10.1530/EC-19-032331394497 [Google Scholar] [CrossRef] [PubMed]
[5]. O’Connor MJ, Snyder EA, Hayes FJ, Klinefelter Syndrome and DiabetesCurr Diab Rep 2019 19(9):7110.1007/s11892-019-1197-331367971 [Google Scholar] [CrossRef] [PubMed]
[6]. Salzano A, D’Assante R, Heaney LM, Monaco F, Rengo G, Valente P, Klinefelter syndrome, insulin resistance, metabolic syndrome, and diabetes: review of literature and clinical perspectivesEndocrine 2018 61(2):194-203.10.1007/s12020-018-1584-629572708 [Google Scholar] [CrossRef] [PubMed]
[7]. Balercia G, Bonomi M, Giagulli VA, Lanfranco F, Rochira V, Giambersio A, Thyroid function in Klinefelter syndrome: a multicentre study from KING groupJ Endocrinol Invest 2019 42(10):1199-204.10.1007/s40618-019-01037-230912057 [Google Scholar] [CrossRef] [PubMed]
[8]. Wq CN, Eide SE, Huang J, Khor YM, Klinefelter’s syndrome with lupus encephalitis and retroperitoneal teratomaLupus 2018 27(9):1559-61.10.1177/096120331877610729759049 [Google Scholar] [CrossRef] [PubMed]
[9]. Shiraishi K, Matsuyama H, Klinefelter syndrome: From pediatrics to geriatricsReprod Med Biol 2018 18(2):140-50.10.1002/rmb2.1226130996677 [Google Scholar] [CrossRef] [PubMed]