Decompressive Craniectomy for Traumatic Acute Extradural Haematoma: Decision Making and Outcomes
Paresh Anil Korde1, Sandeep W Iratwar2, Akshay Patil3, Vijay M Mundhe4, Chetan Tukaram Rathod5
1 Assistant Professor, Department of Neurosurgery, AVBRH, JNMC, Sawangi Meghe, Wardha, Maharashtra, India.
2 Professor and Head, Department of Neurosurgery, AVBRH, JNMC, Sawangi Meghe, Wardha, Maharashtra, India.
3 Associate Professor, Department of Neurosurgery, AVBRH, JNMC, Sawangi Meghe, Wardha, Maharashtra, India.
4 Assistant Professor, Department of Neurosurgery, AVBRH, JNMC, Sawangi Meghe, Wardha, Maharashtra, India.
5 Assistant Professor, Department of Neurosurgery, AVBRH, JNMC, Sawangi Meghe, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sandeep W Iratwar, Professor and Head, Department of Neurosurgery, AVBRH, JNMC, Sawangi (MEGHE)-442001, Wardha, Maharashtra, India.
E-mail: s.iratwar@gmail.com
Extradural Haematoma (EDH) in neurosurgery needs no introduction. It is the most commonly encountered and dealt traumatic pathology in neurosurgery. Operative indications for the same has been in the literature and followed unchecked. Evacuating haematoma and repositioning the bone flap back has been a usual protocol. But decision for Decompressive Craniectomy (DC) in EDH and their outcomes have less vividly thought of. In the present case series the authors shared their experience of 10 patients, of traumatic EDH, who presented with Glasgow Coma Scale (GCS) of <5 and underwent DC with haematoma evacuation in first sitting itself. Based on the experience it is proposed that DC in traumatic EDH patients bring about better outcome in these patients.
Neurosurgery, Non-pulsatile dura, Shock, Swril sign
Case Series
The EDH accounts for 21.5-50% of traumatic intracranial haematomas. The usual protocol of putting the bone flap back after evacuation of the haematoma may actually be the only hindering factor in good outcome of certain patients. Certain patients encountered at the institute and the details are presented herein, which can help determine a criteria to offer DC as primary surgical intervention for EDH [Table/Fig-1].
Patients and their clinico-radiological presentations.
| Case No. | Age (years) | Gender | Preop GCS | Pupils | EDH volume (>100 mL) | Duration of shock (>30 min) |
|---|
| 1 | 35 | M | 4/15 | Anisocoria | Yes | Yes |
| 2 | 44 | F | 4/15 | Anisocoria | Yes | Yes |
| 3 | 33 | M | 3/15 | Bilateral mydriasis | Yes | - |
| 4 | 29 | M | 4/15 | Anisocoria | Yes | Yes |
| 5 | 39 | M | 4/15 | Anisocoria | Yes | Yes |
| 6 | 42 | M | 4/15 | Anisocoria | Yes | Yes |
| 7 | 25 | F | 3/15 | Bilateral mydriasis | Yes | - |
| 8 | 19 | M | 4/15 | Anisocoria | Yes | Yes |
| 9 | 36 | F | 4/15 | Anisocoria | Yes | Yes |
| 10 | 37 | M | 4/15 | Anisocoria | Yes | Yes |
All the patients once received in emergency department were examined neurologically and evaluated with preliminary with CT brain. They were resuscitated, intubated, ventilated and optimised for surgery. After taking informed consent from the relatives patient underwent DC with evacuation of EDH. After surgery patients were kept knocked down on Injection vecuronium and midazolam infusion and ventilated electively for 24 hours. Follow-up CT brain were taken after 24 hours of surgery as per the institutional protocol. All the patients who survived required tracheostomy during their hospital stay which was weaned off in due course. Patients were managed on Antibiotics, Antiepileptics and Antioedema measures. Outcome of the patients were measured based on extended GCS both at the time of discharge and after one year.
Some of the case findings are detailed here, which showed certain important features regarding the radiographic findings and the treatment outcome:
Case 1
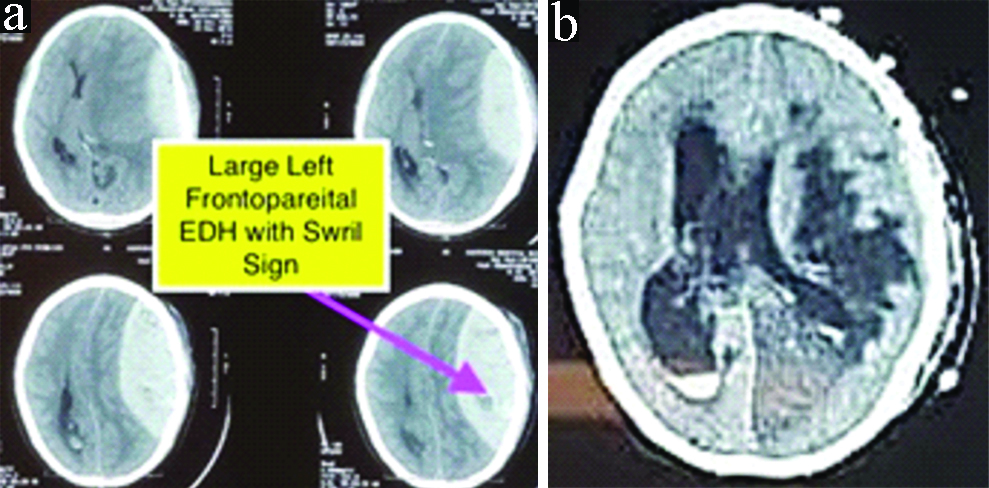
Patient CT brain showed large frontoparietal EDH on Left side with mass effect, midline shift and oedema [Table/Fig-2a]. He underwent left frontoparietal craniotomy and evacuation of EDH. Post evacuation of EDH dura got lax but no transmitting pulsations of the brain could be appreciated even till the time of closure. Dural tenting sutures were taken and bone flap was repositioned back. As per the institutional protocol patient was sedated and ventilated for 24 hours and follow-up CT brain was done after 24 hours. CT showed Left Posterior Cerebral Artery (PCA) territory infarct with oedema, Intraventricular haemorrhage and hydrocephalus with midline shift towards right [Table/Fig-2b]. Patient was again posted for surgery. This time he underwent left fronto-temporo-parietal decompressive craniectomy. Intraoperatively, brain was found tense and bulging. Inspite of all the attempts patient could not survive and succumbed on next day of surgery.
a) Preoperative CT showing left frontoparietal EDH with swirl sign; b) Postoperative CT after 24 hours of surgery showing left PCA territory infarct with oedema and IVH and Hydrocephalus.
Case 2
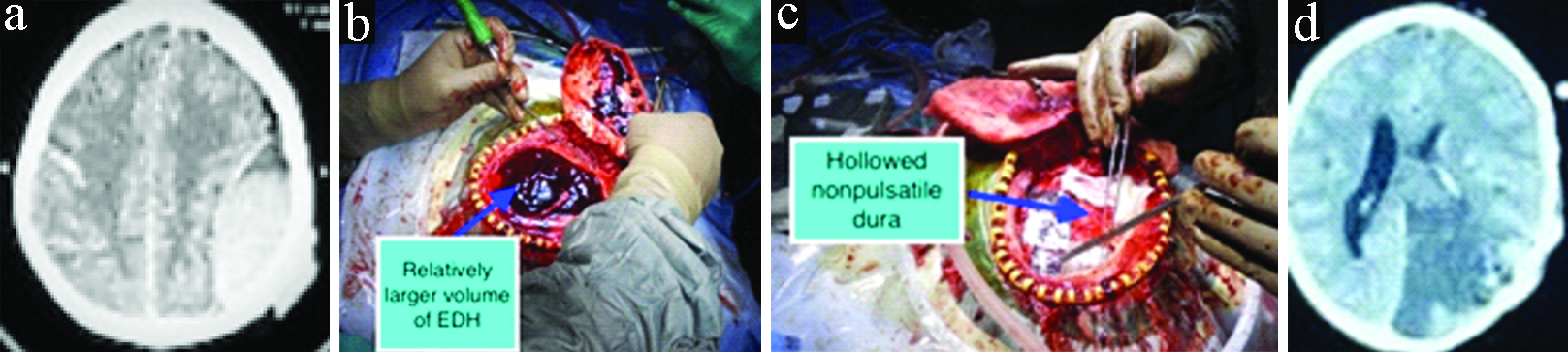
CT showed left parietal EDH with swirl sign [Table/Fig-3a]. Left frontoparietal craniotomy was done to evacuate haematoma. But after craniotomy a relatively larger volume of EDH was found [Table/Fig-3b] and following its evacuation dura was hollowed and was non pulsatile [Table/Fig-3c]. Routine closure of craniotomy done as in previously discussed case and patient was ventilated overnight. Follow-up CT brain after six hours coming morning showed left PCA territory infarct with gross cerebral oedema with midline shift [Table/Fig-3d]. Patient was again posted for emergency DC. Post DC was managed in neurosurgical ICU. Patient needed tracheostomy later and before discharge improved to a GCS of E2VtM4 with pupillary anisocoria. This patient at follow-up of one year had improved to E4V3M5.
a) Preoperative CT done at outside institute in early period of traumatic brain injury showing Left Parietal EDH. Patient got operated almost 6-8 hours after this CT scan; b) Relatively larger volume of EDH found intraoperatively; c) Post evacuation of EDH dura was hollowed and non-pulsatile; d) Follow-up CT scan done after 6 hours which Lt PCA infarct and gross cerebral oedema with midline shift. Patient was posted for emergency decompressive craniectomy.
Remaining eight patients who presented with enlisted clinical and radiological grounds, they opted for DC in addition to EDH evacuation as primary surgical management. Out of eight patients, two patient died in later dates due to ventilatory associated pneumonia and ARDS and rest survived with Extended-Glasgow Outcome Score (E-GOS) of 4 at the time of discharge. Out of the discharged six patients four patients improved to the E-GOS of 7 at the end of one year. Remaining two patients were followed for one year and showed neurological improvement with E-GOS of 6 [Table/Fig-4].
Hospital stay and outcome of the patients.
| Case no. | Days of ventilatory support | Tracheostomy | Days of hospital stay | E-GOS at discharge | E-GOS at 1 year follow-up |
|---|
| 1 | 1 | No | 2 | 1 | - |
| 2 | 14 | Yes | 44 | 3 | 5 |
| 3 | 19 | Yes | 56 | 4 | 7 |
| 4 | 35 | Yes | 37 | 1 | - |
| 5 | 13 | Yes | 32 | 4 | 6 |
| 6 | 10 | Yes | 40 | 4 | 7 |
| 7 | 12 | Yes | 42 | 4 | 7 |
| 8 | 23 | Yes | 25 | 1 | - |
| 9 | 11 | Yes | 34 | 4 | 6 |
| 10 | 8 | Yes | 27 | 4 | 7 |
Discussion
Acute traumatic EDH in neurosurgery do not need any introduction. EDH when dealt in time has shown good neurological outcome with mean hospital stay less than seven days [1]. Brain herniation can occur within 3-24 hours of trauma depending on the volume of EDH [2] which eventually leads to decreased cerebral blood flow, cerebral oedema, ischemia and infracts. Raised intracranial pressure contributes to the pathophysiology of post traumatic massive cerebral infarction.
Overall mortality in these patients is about 76-80% with standard medical care [3]. Such patient needs aggressive antioedema measures and inevitably DC. DC along with lax duraplasty will help oedematous and infarcted brain to expand. This will help to reduce harmful intracranial hypertension [4]. It is a well-known fact that with increased number of surgeries patient undergoes chances of infection and poor prognosis increases [5]. Moreover, DC in EDH is difficult to digest concept for orthodox teaching. Also, DC can be a double edged sword if it results in syndrome of trephined [6]. So, decision regarding EDH evacuation and DC in same sitting in certain patients requires formulation of some guiding criteria.
The present case series encountered certain independent important factors which can prompt one in deciding regarding opting for DC. Poor GCS patient with score <5 with anisocoria for more than two hours from the time of first examination or bilaterally mydriatic pupil at the time of presentation contribute independently to post-traumatic massive cerebral infarct and oedema. Patients who land up in state of shock in emergency department due to raised Intra Cranial Pressure (ICP) for approximately 30 minutes or more can be direct indicator for secondary brain injury resulting infarcts and oedema and poorer prognosis.
Radiologically, factors predictive of indication for DC are volume of EDH more than 100 mL with or without presence of swirl sign. Swril sign is indicator of ongoing active bleed which can be seen as hypodense area in an hyperdense area of haematoma [7-9]. Swril Sign is an independent predictor of poor outcome in the form of mortality and morbidity [8]. Evidence of evolving infract in the territory of Middle Cerebral Artery (MCA) or PCA can also serve as an indicator for need of DC. CT brain revealing midline shift itself is a definitive indicator for raised ICT which is known to lead the vicious cycle of low cerebral perfusion, ischemia, oedema and eventually infarction. But midline shift more than 1.5 cm and corresponding positively fitting criteria like poor GCS, large volume EDH, state of shock, etc., can prove to be a strong supporting factor for decision making. In circumstances where only EDH evacuation was performed and follow-up CT showed gross oedema and midline shift more than 5 mm, patient needed DC. Patient with midline shift <5 mm post EDH evacuation can be managed conservatively [10].
Not only clinical and radiological factors have influence on decision making, but also intraoperative findings and operating surgeon’s experience can. In authors’ experience, a patient with large EDH has temporary hollowing of the brain due to mass effect of haematoma which reflects as depression on the dural surface after immediate removal of the haematoma. Such patients will have brain pulsations transmitted through the hollowed dura which is a good sign. But no evidence of such pulsations or surfacing of the dura or dura becoming tense by the time of closure of the craniotomy should also tickle the thought of opting for DC in such patients [5]. There are instances when patient are posted for EDH evacuation with a CT scan done at early period of Traumatic Brain Injury (TBI) showing average size EDH, but on table surgeon discovers a huge haematoma. Such an out of proportion haematoma size compared to the preoperative CT scan can be a supplement to other independent factors for deciding on DC. Any other site for EDH other than temporoparietal EDH/transtemporal EDH was not encountered. Transtemporal EDH are more associated with poor GCS [5,11].
With the experience which authors had through the study, it can be said that decision making regarding some cases with large supratentorial EDH with poor score, can be tricky. We hereby, suggest a criteria that could help in decision making of DC in supratentorial traumatic EDH patients.
Clinical aspect:
1) GCS <5
2) Pupillary asymmetry/anisocoria for >2 hours
3) Bilateral mydriasis
4) Shock >30 mins
Radiological aspects:
1) Volume of EDH > 100 mL calculated by (width×length×breadth)/2 with or without swirl sign
2) Midline shift >1.5 cm
3) e/o territorial infract (e.g., MCA, PCA)
4) Follow-up CT suggestive of gross cerebral oedema and midline shift post haematoma evacuation.
Intraoperative aspects:
1) Significantly larger volume of EDH as compared to preoperative CT scan
2) Bulging brain/tense dura at the time of closure during surgery
3) Lax brain with no brain pulsations transmitted through the dura.
Even after the above given criteria surgeon may experience ambiguity while making decision. This is because most of these patients are electively ventilated and pupillary anisocoria may not always resolve immediately after evacuation of haematoma alone. In such circumstances every 6 hourly follow-up CT brain is suggested to detect need for DC early. Though the suggestions out of the authors experience are based on sample size of 10 cases only but need for the decision of DC in acute traumatic EDH is pressing. So formulating criteria for the same will require bigger sample size study.
Conclusion(s)
Decompressive craniectomy in certain traumatic EDH patients chosen according to the proposed guidelines can bring favourable outcomes and thus can form basis for formulating definite indications for DC as primary surgical management in EDH.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 31, 2019
Manual Googling: Dec 30, 2019
iThenticate Software: Dec 31, 2019 (11%)
[1]. Araujo JL, Aguiar Udo P, Todeschini AB, Saade N, Veiga JC, Epidemiological analysis of 210 cases of surgically treated traumatic extradural hematomaRev Col Bras Cir 2012 39(4):268-71.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2293622410.1590/S0100-6991201200040000522936224 [Google Scholar] [CrossRef] [PubMed]
[2]. Mangla R, Ekhom S, Jahromi BS, Almast J, Mangla M, Westesson PL, CT perfusion in acute stroke: Know the mimics, potential pitfalls, artifacts, and technical errorsEmerg Radiol 2014 21(1):49-65.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2377160510.1007/s10140-013-1125-923771605 [Google Scholar] [CrossRef] [PubMed]
[3]. Subramaniam S, Hill MD, Massive cerebral infarctionNeurologist 2005 11(3):150-60.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1586013710.1097/01.nrl.0000159987.70461.d715860137 [Google Scholar] [CrossRef] [PubMed]
[4]. Mori K, Nakao Y, Yamamoto T, Maeda M, Early external decompressive craniectomy with duroplasty improves functional recovery in patients with massive hemispheric embolic infarctionSurg Neurol 2004 62(5):420-29.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1551885010.1016/j.surneu.2003.12.01715518850 [Google Scholar] [CrossRef] [PubMed]
[5]. Wang W, Hu L, Lin H, Li J, Luo F, Huang W, Risk factors for post-traumatic massive cerebral infarction secondary to space-occupying epidural hematomaJ Neurotrauma 2014 31(16):1444-50.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2477355910.1089/neu.2013.314224773559 [Google Scholar] [CrossRef] [PubMed]
[6]. Okamoto T, Umezawa K, Ogita S, Kurosaki K, Takegami T, Kimura S, Two cases of difficult-to-treat acute epidural hematoma and a review of decompressive craniectomy with hematoma evacuationNo Shinkei Geka 2018 46(3):227-34.Available from: http://www.ncbi.nlm.nih.gov/pubmed/29567873 [Google Scholar]
[7]. Xiong X, Li Q, Yang W-S, Wei X, Hu X, Wang XC, Comparison of swirl sign and black hole sign in predicting early hematoma growth in patients with spontaneous intracerebral hemorrhageMed Sci Monit 2018 24:567-73.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2937511810.12659/MSM.90670829375118 [Google Scholar] [CrossRef] [PubMed]
[8]. Guo C, Liu L, Wang B, Wang Z, Swirl sign in traumatic acute epidural hematoma: Prognostic value and surgical managementNeurol Sci 2017 38(12):2111-16.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2889494310.1007/s10072-017-3121-428894943 [Google Scholar] [CrossRef] [PubMed]
[9]. Ng D, Churilov L, Mitchell P, Dowling R, Yan B, The CT Swirl Sign is associated with Hematoma Expansion in Intracerebral HemorrhageAm J Neuroradiol 2018 39(2):232-37.Available from: http://www.ajnr.org/lookup/doi/10.3174/ajnr.A546510.3174/ajnr.A546529217744 [Google Scholar] [CrossRef] [PubMed]
[10]. Tu PH, Liu ZH, Chuang CC, Yang TC, Wu CT, Lee ST, Postoperative midline shift as secondary screening for the long-term outcomes of surgical decompression of malignant middle cerebral artery infarctsJ Clin Neurosci 2012 19(5):661-64.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2237763710.1016/j.jocn.2011.07.04522377637 [Google Scholar] [CrossRef] [PubMed]
[11]. Otani N, Takasato Y, Masaoka H, Hayakawa T, Yoshino Y, Yatsushige H, Surgical outcome following a decompressive craniectomy for acute epidural hematoma patients presenting with associated massive brain swellingIn: Acta neurochirurgica Supplement 2010 106:261-64.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1981296110.1007/978-3-211-98811-4_4919812961 [Google Scholar] [CrossRef] [PubMed]