Bilateral Endogenous Cryptococcal Endophthalmitis in an Immunocompetent Host Treated with Two Different Tailored Approaches
Luigi Sborgia1, Alfredo Niro2, Giancarlo Sborgia3, Alessandra Sborgia4, Giovanni Alessio5
1 Department of Medical Science, Neuroscience and Sense Organs, University of Bari, Bari, Puglia, Italy.
2 ASL Taranto, Eye Clinic, Hospital “S. G. MOSCATI”, Taranto, Puglia, Italy.
3 Department of Medical Science, Neuroscience and Sense Organs, University of Bari, Bari, Puglia, Italy.
4 ASL Taranto, Eye Clinic, Hospital “S. G. MOSCATI”, Taranto, Puglia, Italy.
5 Department of Medical Science, Neuroscience and Sense Organs, University of Bari, Bari, Puglia, Italy.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Alfredo Niro, Strada per Martina, Statte, Taranto, Puglia, Italy.
E-mail: alfred.nir@tiscali.it
Endogenous fungal endophthalmitis is one of the most severe and rare ocular pathologies. Rarely, it occurs in healthy and immunocompetent people and is observed in both eyes. This case report describes diagnosis and treatment of a rare case of bilateral endogenous fungal endophthalmitis with different degree of severity. Smear and culture of vitreous samples were not helpful in confirming the aetiology but blood samples revealed Cryptococcus neoformans antigen. Systemic therapy was set up with voriconazole. Vitrectomy with intravitreal injection of voriconazole was performed in left eye as it was clincally worst, while only intravitreal injection of antifungal drug was performed in right eye. After 3 months of follow-up, a relevant functional and morphologic improvement was reported in both eyes. Cryptococcal endogenous endophthalmitis is a challenge for ophthalmologists. Prompt aggressive treatments tailored to the known aetiology and clinical conditions are imperative to achieve good morpho-functional recovery in case of bilateral involvement with different degree of severity.
Cryptococcus neoformans, Endogenous endophthalmitis, Intravitreal injection, Vitrectomy, Voriconazole
Case Report
An 86-year-old female presented to the clinic complaining of bilateral blurred vision and floaters for over 3 weeks, prior to the presentation. She underwent hemicolectomy for adenocarcinoma two months earlier and did not receive chemotherapy. She had no fever or neurological symptoms.
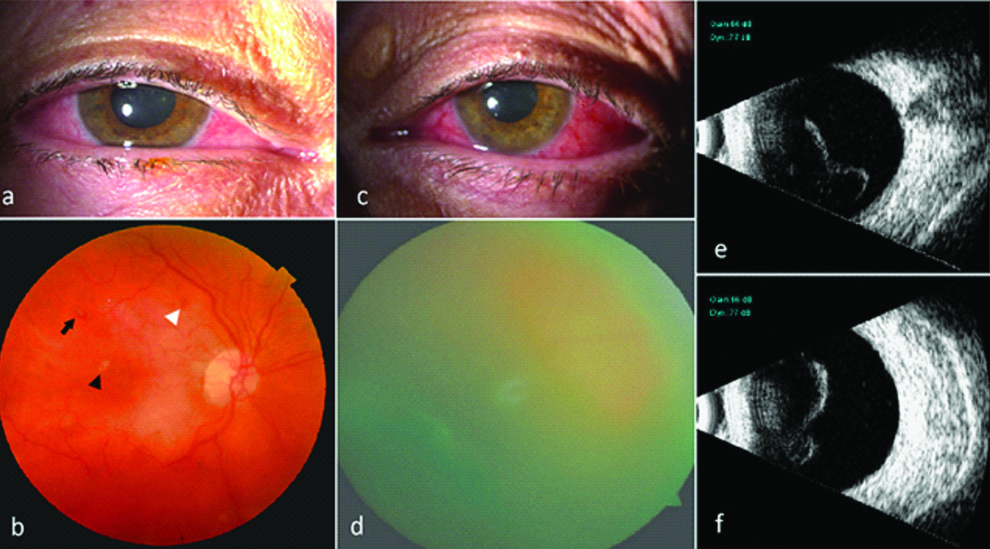
Visual acuity was 20/40 in the right eye and hand motions in the left eye. Ophthalmic examination revealed cataract, vitreous cells, retinal haemorrhages, cotton wool spots and white-centre retinal haemorrhages like Roth spots in the right eye, corneal oedema, anterior chamber cells, opacification of posterior chamber intraocular lens, vitreous cells and severe vitreous haze in the left eye. Ocular ultrasonography showed dense opacities and membranes in the vitreous of the left eye [Table/Fig-1].
Bilateral Endogenous Cryptococcus neoformans endophthalmitis.
Right eye: a) Slit-lamp photography; b) Retinography showing vitreous cells 1+, rare retinal haemorrhages (white arrowhead), cotton wool spots (black arrowhead) and Roth spots (black arrow).
Left eye: c) Slit-lamp photography; d) Retinography showing vitreous cells 4+ with Grade 4 vitreous haze hindering retinal visualisation; e-f) ultrasonography B-scans reveal dense hyper-reflective opacities as dots and membranes in the vitreous cavity.
Leukocytosis (14300/μL) with a left shift (neutrophil count: 76.8%) was found. CD3 T-cells, CD19 B-cells, CD4 helper/inducer cells, CD8 suppressor/cytotoxic cells, and CD4/CD8 ratio were normal confirming immunocompetent status. Rapid plasma regained, anti-Toxoplasma IgM and IgG, HIV and HLA-B27 were negative. Erythrocyte sedimentation rate and C-reactive protein were elevated and Antinuclear Antibody (ANA) was negative.
Oral, faecal and urine cultures did not reveal microbial growth, but blood samples were positive for Cryptococcus neoformans antigen (blood titer 1:530). Abdominal echography and whole body CT did not reveal any source of infection.
Systemic voriconazole was administered (400 mg twice a day for the first day, tapered to 200 mg twice a day for 20 days), serum levels were monitored to avoid toxicity and the patient was sent to the surgeon. After obtaining informed consent, surgery was performed in left eye. Explantation of the intraocular lens was performed. Vitreous was aspirated before starting the infusion to get an undiluted sample. A “core” vitrectomy was performed followed by induction of posterior vitreous detachment. Vitreous and membranes were removed with low suction and high cut-rate. At the intraoperative examination, mild oedema was observed involving the posterior pole, retinal haemorrhages and Roth spots. After an extensive vitrectomy, the patient received intravitreal injection of voriconazole 100 μg/0.1 mL followed by silicone oil injection. In the right eye an intravitreal injection of voriconazole 100 μg/0.1 mL was performed after a vitreous tap.
Smears and cultures of vitreous samples were negative for any agents. Histological evaluation of vitreous samples revealed granulomatous inflammation. Polymerase Chain Reaction (PCR) was not done.
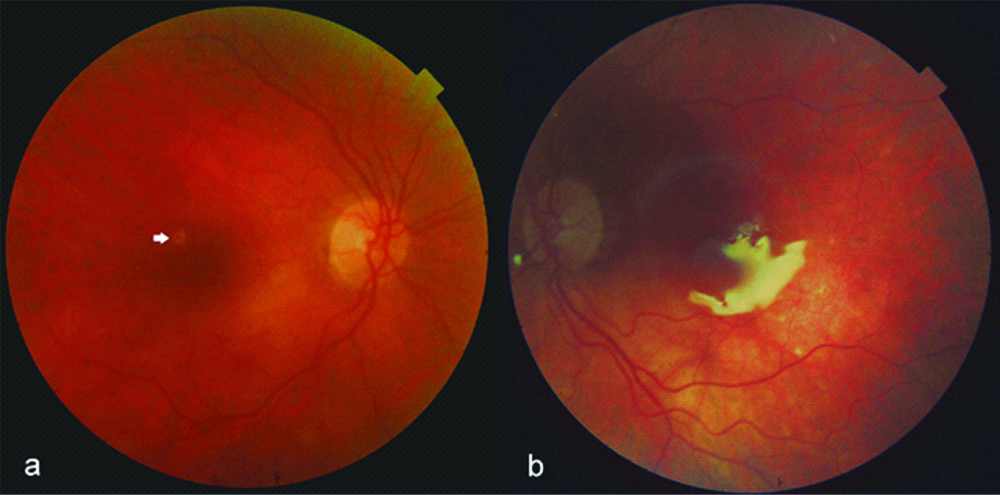
After 3 months without recurrence, visual acuity improved to 20/25 in right eye and 20/40 in left eye. Intraocular pressure was normal in both eyes. A complete resolution of inflammation signs, retinal haemorrhages and exudates were observed in both eyes [Table/Fig-2]. Cryptococcal antigen of blood was 1:50. Silicone oil removal and intraocular lens implantation in left eye were scheduled.
Bilateral Endogenous Cryptococcus neoformans endophthalmitis after treatment.
a) Retinography showing resolution of vitreous cells, haemorrhages and cotton wool sposts in right eye and at 3 months after treatment, extrafoveal retinal atrophy occurred after resolution of an exudate. (white arrow); b) silicone oil-filled left eye.
Discussion
Endogenous Endophthalmitis (EE) is one of the most severe ocular pathologies and comprises about 2-8% of all endophthalmitis [1]. It rarely occurs in healthy and immunocompetent people [1] and is often associated with a medical condition, including diabetes, liver disease, cardiac disease, malignancy, in-dwelling catheters, recent surgery and intravenous drug abuse [2]. It originates when a hematogenous agent passes the blood-ocular barrier and fungal organisms account for the majority of the cases [2,3]. Cryptococcus neoformans is an opportunistic yeast. Bilateral cryptococcal EE is rare and can appear as granulomatous inflammation with varying degree of severity [1-4]. Many patients with Fungal EE (FEE) are misdiagnosed and the prognosis is poor [3].
The PCR testing is rapid and sensitive in diagnosing fungal endophthalmitis [1,2] but was not available at this centre. Aqueous humour or vitreous smear and culture can suffer from poor sensitivity which could make diagnosis difficult and time consuming [5]. In the index case, smear and culture were not helpful in confirming an aetiological agent and granulomatous inflammation revealed was not pathognomonic. Dubbels M et al., found that Cryptococcus was not identified in culture or by histopathology in 47.4% of patients with positive antigen [6].
So identification of extraocular infection is particularly important in case where vitreous cultures are negative [1], as occurred in this patient. Systemic voriconazole which is effective and with good safety profile was administered [4]. However, a systemic approach alone might not be enough in EE, so intravitreal injection with or without vitrectomy should be considered. The present authors performed a single intravitreal antifungal injection in the RE that presented better clinical findings, obtaining good results. The use of vitrectomy is recommended for severe and sight-threatening endophthalmitis [1]. Retrospective series reported better outcomes with vitrectomy in postoperative endophthalmitis, including cases presenting with better than light perception visual acuity [7,8]. Early vitrectomy for FEE has been associated with better prognosis [9,10]. Sadiq MA et al., confirmed the effectiveness of intravitreal injection alone or combined to vitrectomy related to systemic debility, ocular findings and visual acuity [1]. The explantation of the intraocular lens, the induction of vitreous detachment beyond the equator and a more extensive vitrectomy could lead to better outcomes [8-10]. However, oil tamponade limiting the movements of aqueous humour and the penetration of microorganisms can favour better outcomes [11].
Conclusion(s)
Bilateral FEE is a challenge for ophthalmologists and the time span for intervention is limited. In this case, treatment was first guided by the identification of the blood antigen and by the different degree of severity of ocular findings and visual impairment. Good recovery of both eyes suggested the efficacy of systemic therapy combined with a local approach, tailored to the clinical conditions.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 28, 2019
Manual Googling: Oct 09, 2019
iThenticate Software: Nov 29, 2019 (8%)
[1]. Sadiq MA, Hassan M, Agarwal A, Sarwar S, Toufeeq S, Soliman MK, Endogenous endophthalmitis: Diagnosis, management, and prognosisJournal of Ophthalmic Inflammation and Infection 2015 5:3210.1186/s12348-015-0063-y26525563 [Google Scholar] [CrossRef] [PubMed]
[2]. Connell PP, O’Neill EC, Fabinyi D, Islam FMA, Buttery R, McCombe M, Endogenous endophthalmitis: 10-year experience at a tertiary referral centreEye (Lond) 2011 25(1):66-72.10.1038/eye.2010.14520966972 [Google Scholar] [CrossRef] [PubMed]
[3]. Sridhar J, Flynn HW Jr, Kuriyan AE, Miller D, Albini T, Endogenous fungal endophthalmitis: Risk factors, clinical features, and treatment outcomes in mold and yeast infectionsJ Ophthalmic Inflamm Infect 2013 3(1):6010.1186/1869-5760-3-6024053550 [Google Scholar] [CrossRef] [PubMed]
[4]. Vela JI, Díaz-Cascajosa J, Sanchez F, Roselló N, Buil JA, Management of endogenous cryptococcal endophthalmitis with voriconazoleCan J Ophthalmol 2009 44(6):61-62.10.3129/i09-15320051999 [Google Scholar] [CrossRef] [PubMed]
[5]. Sharma S, Jalali S, Adiraju MV, Gopinathan U, Das T, Sensitivity and predictability of vitreous cytology, biopsy, and membrane filter culture in endophthalmitisRetina 1996 16:525-29.10.1097/00006982-199616060-000109002137 [Google Scholar] [CrossRef] [PubMed]
[6]. Dubbels M, Granger D, Theel ES, Low cryptococcus antigen titers as determined by lateral flow assay should be interpreted cautiously in patients without prior diagnosis of cryptococcal infectionJ Clin Microbiol 2017 55(8):2472-79.10.1128/JCM.00751-1728566315 [Google Scholar] [CrossRef] [PubMed]
[7]. Shen X, Xu G, Vitrectomy for endogenous fungal endophthalmitisOcul Immunol Inflamm 2009 17(3):148-52.10.1080/0927394080268939619585356 [Google Scholar] [CrossRef] [PubMed]
[8]. Kuhn F, Gini G, Complete and early vitrectomy for endophthalmitis (CEVE) as today’s alternative to the Endophthalmitis vitrectomy studyVitreo retinal surgery: Essentials in ophthalmology 2007 Chapter 5:53-68.10.1007/978-3-540-33670-9_5 [Google Scholar] [CrossRef]
[9]. Behera UC, Budhwani M, Das T, Basu S, Padhi TR, Barik MR, Role of early vitrectomy in the treatment of fungal endophthalmitisRetina 2018 38(7):1385-92.10.1097/IAE.000000000000172728541964 [Google Scholar] [CrossRef] [PubMed]
[10]. Chee YE, Eliott D, The role of vitrectomy in the management of fungal endophthalmitisSemin Ophthalmol 2017 32(1):29-35.10.1080/08820538.2016.122839627792412 [Google Scholar] [CrossRef] [PubMed]
[11]. Nagpal M, Jain P, Nagpal K, Pars Plana Vitrectomy with or without Silicone Oil Endotamponade in Surgical Management of EndophthalmitisAsia Pac J Ophthalmol (Phila) 2012 1(4):216-21.10.1097/APO.0b013e31826000cd26107476 [Google Scholar] [CrossRef] [PubMed]