Initial resuscitation and management of trauma patients with cervical spine injury is of utmost importance. These patients usually land up in cervical cord injury as complication. Incidence of cervical spine injury is approximately 40 to 80 new cases per million populations per year as estimated by WHO [1]. Patients with cervical spine injury usually lands up in securing the airway as an emergency basis or electively during the surgical procedure. Hence, anaesthesiologist and the trauma team should be familiar in techniques which minimises the cervical cord injury.
The traditional way of intubation involves almost full extension of atlanto-occipital and atlanto-axial joint and flexion of lower cervical spine. This movement can disrupt the spinal cord with patients having cervical spine injury [2]. Hauswald M et al., have demonstrated that nasal intubation was the least in causing cervical spine displacement (1.20 mm) followed by the traditional oral intubation (1.65 mm). Avoid mask ventilation in these type of patient which is prone to cause maximum displacement (2.93 mm) [3]. Various manoeuvres have been suggested to prevent or reduce displacement during airway management which includes natural position using collars, manual inline stabilisation, hardboard with sandbags, and traction pins. Manual In Line Stabilisation (MILS) [4] otherwise known as “manual in-line axial traction is found to be ideal for preventing fracture displacement during mask ventilation as well as during laryngoscopy and intubation. This manoeuvre stabilises patient’s occiput and mastoid process. Even though MILS is suitable to prevent displacement; it increases difficult intubation score by avoiding oral and pharyngeal axis in one line. Nolan JP and Wilson ME in his study found that manual inline stabilisation makes laryngoscopic view difficult and out of his total study population, 22% of people had grade 3 laryngoscopic view with usage of conventional laryngoscopic method [5].
Historically, surgical airway, cricothyrotomy or awake fibreoptic intubation were considered as the preferred route for securing the airway over laryngoscopy assisted oro tracheal intubation. However, advent of Video Laryngoscopes (VL) has changed the scenario in difficult airway situation [6]. VL has been demonstrated to provide an improved Cormack-Lehane grade view over direct laryngoscopy. However, this does not necessarily translate to a higher success rate or decreased time to intubation. Most of the previous studies are either on manikin with MILS or on difficult airway scenarios without MILS or using first generation video laryngoscopes [7-9].
Hence this study was conducted to assess the efficacy of C-MAC D blade (second generation VL) versus MC Coy blade laryngoscopes for intubation in simulated MILS [Table/Fig-1].
Materials and Methods
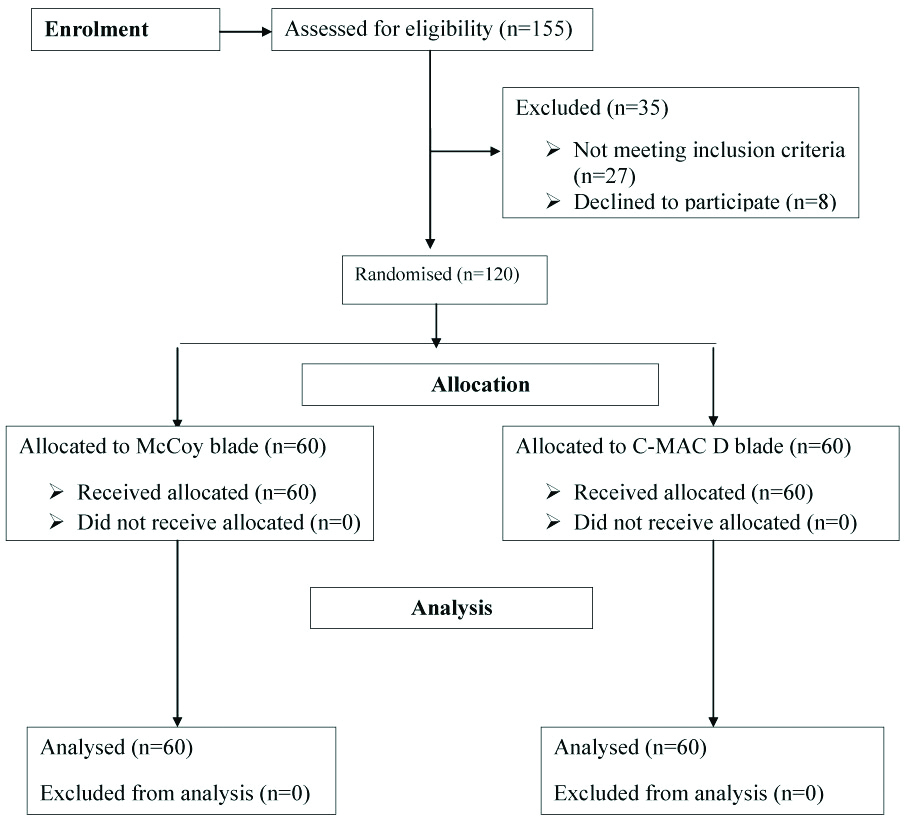
A Randomised Clinical Trial was done after approval by the ethical and scientific committee (RC/15/17) and the period of the study was from September 2015 to August 2017. The protocol was registered at ClinicalTrial.gov (CTRI Reg. No-REF/2016/07/011890). Total of 120 patients were enrolled in the study after taking informed and written consent [Table/Fig-2]. Power analysis was performed to determine the sample size needed. Based on standard deviation of time to successful intubation of 30 seconds, analysis indicated a sample size of 55 patients in each group, thus provides 80% power and 5% level of significance to detect 6s difference between devices. A decision was made to recruit 60 patients per group to allow dropouts.
Primary aim was to determine the time taken for tracheal tube insertion between C-MAC D blade versus McCoy blade with manual inline axial stabilisation.
Secondary aim was to identify the need for airway adjuncts like Bougie or requirement of optimisation manoeuvre between both the blades and to monitor Haemodynamic Changes (Heart rate, Blood pressure) between the blades.
Inclusion Criteria
Patients with (ASA) physical status of I and II, between 18-60 years of age, of either sex, with BMI of less than 30 kg/m2, undergoing elective surgical procedures requiring endotracheal intubation were selected for the study.
Exclusion Criteria
Obesity (body mass index >30) and neck circumference >42 cm, anticipated difficult airway, airway trauma/distortion, patients with cardiac disease, patients undergoing emergency life saving procedures, pregnant patients were excluded from the study.
Patients were randomised by computer-generated block randomisation into two groups: Group A (n=60) for McCoy blade and group B (n=60) for C-MAC D blade.
Methods
Preanaesthetic assessment was done prior to the day of surgery. All patients were kept nil per oral for 8 hours prior to surgery. Routine monitoring modalities included 3 lead ECG, pulse oximetry, Non-invasive Blood pressure. A peripheral venous access was secured using 18G venflon. All Patients were pre-oxygenated with 100% oxygen for 3 minutes. All the patients were induced with 2 μg/kg of Fentanyl, 2.5 mg/kg of Propofol, and muscle relaxation was achieved with 0.1 mg/kg of Vecuronium. Patients were manually ventilated with Sevoflurane 2% in oxygen for 3 minutes. After neuromuscular blocking agent was given, neck was immobilised using MIAS which reduces the movements of the cervical spine.
Laryngoscopy was performed using C-MAC D or McCoy blade by an experienced anaesthesiologist who had done at least 30 intubations, with each device. Following parameters were noted during the study; Cormack and Lehane grading, external manipulation if required, Use of Bougie if required. Trachea was intubated with appropriate size endotracheal tube. External manipulation was applied if Cormack and Lehane grading was equal or more than 2b. Bougie was used if Cormack and Lehane grading was equal or more than 2b even after external manipulation. If the intubation was not possible or if it required more than 3 attempts for intubation or intubation time was more than 90 seconds with episodes of desaturation (spO2 <92%), then intubation was considered as a failure. In such situations, MIAS were removed and patients were intubated using standard intubation practice.
The time from the removal of facemask, to connection of endotracheal tube to the circuit with the appearance of normal ETCO2 curve were noted and was taken as the intubating time.
Statistical Analysis
Statistical analysis was performed using SPSS v20 (IBM® SPSS® Statistics V20). Time for successful intubation and haemodynamic parameters were analysed using Z-test. The chi-square test was used for Cormack lehane and IDS grading. Patients’ characteristics like age, gender, BMI and ASA were analysed using Z and chi-square test wherever required. p<0.05 was considered significant.
Results
Demographic data were matched in both the study groups. There was no statistically significant difference between both groups as regards to the demographic data [Table/Fig-3].
Patients demographic data compared between the two groups.
| Data | McCoy group (n-60) | C-MAC D group (n-60) | Test | p-value | Significance |
|---|
| Age (years) | 37.67±12.71 | 36.38±12.519 | Z-test | 0.578 | Not significant |
| Sex | M-37; F-23 | M-29; F-31 | Chi-square test | 0.142 | Not significant |
| BMI | 23.93±2.20 | 23.84±2.20 | Z-test | 0.833 | Not significant |
| ASA grading | ASA 1-32ASA 2-28 | ASA 1-30ASA 2-30 | Chi-square test | 0.715 | Not Significant |
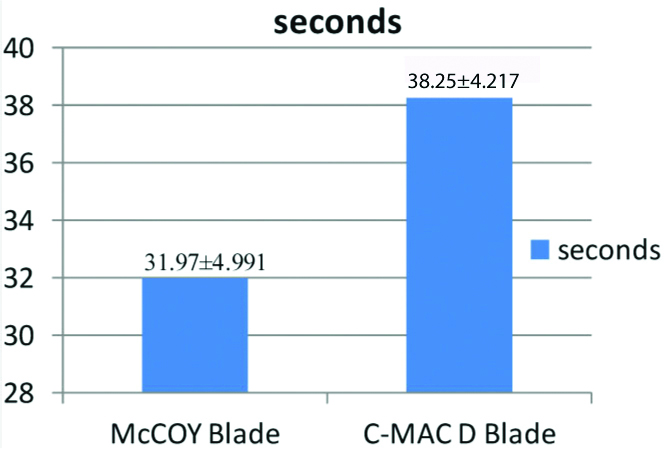
The time taken for intubation using McCoy laryngoscope was significantly shorter compared to C-MAC D blade [Table/Fig-4]. There was no significant difference in C-L grading between the two groups [Table/Fig-5].
Mean time taken for intubation between the two groups.
Distribution of cormack lehane grading among study participants.
| Grading | Blade | Total |
|---|
| McCoy blade | C-Mac D blade |
|---|
| CormackLehaneGrading | 1 | 33 | 32 | 65 |
| 2a2b3a | 15120 | 16102 | 31222 |
| Total | 60 | 60 | 120 |
Chi-square test; DOF=2; p-value=0.976
There was an increase in heart rate at 1, 2 minutes after intubation in both the groups which came back to baseline after 5 minutes of intubation. However, it was not statistically significant [Table/Fig-6].
Mean heart rate of study participants during baseline, induction and postintubation compared between the two groups.
| Heart rate | Blade | N | Mean | Standard deviation | p-value* |
|---|
| Preinduction Hr | McCoy blade | 60 | 85.13 | 8.313 | |
| C-Mac D blade | 60 | 84.08 | 7.351 | 0.465 |
| Intubation Hr | McCoy blade | 60 | 82.70 | 9.917 | |
| C-Mac D blade | 60 | 81.07 | 9.822 | 0.367 |
| Post Intubation Hr (1 Min) | McCoy blade | 60 | 92.45 | 8.666 | |
| C-Mac D blade | 60 | 95.00 | 6.214 | 0.067 |
| Post Intubation Hr (2 Min) | McCoy blade | 60 | 90.27 | 8.647 | |
| C-Mac D blade | 60 | 92.17 | 6.473 | 0.175 |
| Post Intubation Hr (3 Min) | McCoy blade | 60 | 84.50 | 7.892 | |
| C-Mac D blade | 60 | 86.78 | 6.376 | 0.084 |
| Post Intubation Hr (5 Min) | McCoy blade | 60 | 78.50 | 7.494 | |
| C-Mac D blade | 60 | 80.84 | 6.779 | 0.075 |
There was an increase in Mean Arterial Pressure (MAP) at 1, 2 minute after intubation in both the groups which came back to baseline after 5 minutes of intubation. However, it was not statistically significant [Table/Fig-7].
Mean MAP of study participants during baseline, on intubation and post intubation are compared between the two groups.
| Blade | N | mean | SD | p-value |
|---|
| Preinduction | McCoy blade | 60 | 83.50 | 12.90 | 0.868 |
| C-MAC D blade | 60 | 83.01 | 13.04 | |
| intubation | McCoy blade | 60 | 76.20 | 13.06 | 0.670 |
| C-MAC D blade | 60 | 77.63 | 12.21 | |
| Postintubation 1 minute | McCoy blade | 60 | 83.57 | 12.97 | 0.447 |
| C-MAC D blade | 60 | 85.80 | 11.43 | |
| Postintubation 2 minute | McCoy blade | 60 | 81.30 | 11.16 | 0.420 |
| C-MAC D blade | 60 | 83.03 | 13.06 | |
| Postintubation 3 minute | McCoy blade | 60 | 76.70 | 13.22 | 0.267 |
| C-MAC D blade | 60 | 80.11 | 11.50 | |
| Postintubation 5 minute | McCoy blade | 60 | 78.80 | 09.41 | 0.920 |
| C-MAC D blade | 60 | 79.10 | 10.80 | |
There was no significant difference in saturation between both the two groups [Table/Fig-8].
Mean saturation of study participants during baseline, on intubation and post-intubation were compared between the two groups.
| Saturation | Blade | N | Mean | Std. deviation | p-value* |
|---|
| Preinduction saturation | McCoy blade | 60 | 98.87 | 0.911 | |
| C-MAC D blade | 60 | 98.93 | 0.756 | 0.663 |
| Intubation saturation | McCoy blade | 60 | 98.57 | 0.909 | |
| C-MAC D blade | 60 | 98.50 | 1.066 | 0.713 |
| Post intubation saturation (1 Min) | McCoy blade | 60 | 98.52 | 1.225 | |
| C-MAC D blade | 60 | 98.62 | 1.263 | 0.660 |
| Post intubation saturation (2 Mins) | McCoy blade | 60 | 98.12 | 0.739 | |
| C-MAC D blade | 60 | 98.15 | 0.685 | 0.798 |
| Post intubation saturation (3 Mins) | McCoy blade | 60 | 98.18 | 0.748 | |
| C-MAC D blade | 60 | 98.28 | 0.640 | 0.433 |
| Post intubation saturation (5 Mins) | McCoy blade | 60 | 97.05 | 11.607 | |
| C-MAC D blade | 60 | 98.77 | 0.673 | 0.257 |
There was no significant difference in requirement of bougie or external manipulation for intubation between both the two groups [Table/Fig-9,10].
Distribution of study participants based on the requirement of bougie.
| Blade | Total |
|---|
| McCOY blade | C-MAC D blade |
|---|
| Requirement of bougie | Yes | 0 | 2 | 2 |
| No | 60 | 58 | 118 |
| Total | 60 | 60 | 120 |
Fisher’s-exact test; p-value=1.000
Distribution of study participants based on the requirement of external manipulation.
| External manipulation | Blade | Total |
|---|
| McCOY blade | C-MAC D blade |
|---|
| Requirement of external manipulation | Yes | 12 | 12 | 24 |
| No | 48 | 48 | 96 |
| Total | 60 | 60 | 120 |
Yate’s corrected Chi-square test; p-value=1.000
Discussion
This study was done to compare the time taken for intubation in patients with simulated cervical spine injury with application of manual inline axial stabilisation using C-MAC D blade versus McCoy blade. Of one hundred and twenty patients, sixty patients were randomised into two groups. The basic parameters which include age, sex and American society of Anaesthesiologist status were comparable between the two groups.
The laryngoscopic views between the two groups were not significantly different. A study conducted by Laila AS and Shaarawy SS revealed some significant difference between both the groups in Cormack-Lehane class 1 while there was no significant difference between the two groups in C-L class 2b and 3 suggesting that C-MAC D blade and McCoy blade didn’t show much difference in C-L grading [10].
External laryngeal manipulation was given for patients with grade >2b. Twelve patients in McCoy group and twelve patients in C-MAC D blade required external manipulation. A study conducted by Aziz MF et al., revealed less requirement of manipulation in C-MAC intubation compared with direct laryngoscopy [11].
Optimisation maneuver were not used in McCoy blade group and was used in two patients in C-MAC D blade group. A study conducted by Hodgetts V et al., compared between C-MAC and Macintosh and concluded that use of bougie was higher with C-MAC than with Macintosh but there was no significant difference between the two groups [12].
The time taken for intubation in this study for C-MAC D blade group was much higher compared with McCoy blade group. A study conducted by Bag SK et al., compared between Truview and Macintosh laryngoscopes and concluded that Truview laryngoscopes took a longer time compared with Macintosh [13].
The haemodynamic responses were noted with both the two groups in this study and there was no statistically significant difference between the two groups. A study conducted by Hiteshi A et al., compared the haemodynamic responses for orotracheal intubation between Macintosh, McCoy and C-MAC VL and concluded that McCoy blade had less responses compared with other two blades [14].
Limitation(s)
More patients were recruited in the study in view of unanticipated patients with Modified Cormack Lehane grading 4, an exclusion criterion after randomisation. This post randomisation was a limitation to the study. However, none of the patients had grade 4 and hence the results were not affected. Another limitation to the study was anaesthetist recording the laryngoscopic view could not be blinded to the device being used. Hence the observer bias could not be eliminated.
Conclusion(s)
C-MAC D blade as well as McCoy blade forms an effective tool for the airway management of suspected cervical spine injured patients with cervical immobilisation.
Chi-square test; DOF=2; p-value=0.976
Fisher’s-exact test; p-value=1.000
Yate’s corrected Chi-square test; p-value=1.000