Cavernous haemangioma of the maxillary sinus often presents with recurrent epistaxis and nasal obstruction. Clinical features usually mimics sinonasal mass or antrochoanal polyp. We report this case of a 13 years old female patient with unilateral maxillary sinus cavernous haemangioma which was managed successfully by both endoscopic and Caldwell Luc approach. The patient presented with features of antrochoanal polyp. Radiologically, it was suspected to be an Angiomatous Antrochoanal polyp and histologically proved to be a cavernous haemangioma. Postoperative period was uneventful.
Caldwell luc, Sinonasal tract, Vascular tumour
Case Report
A 13-year-old female patient presented with complaints of epistaxis from left nasal cavity, for 20 days that was associated with left-sided nasal obstruction. There was no history of nasal trauma or surgery or any other nasal complaints. On physical examination, external osseocartilagenous framework and vestibule were normal. Anterior rhinoscopy revealed a pale polyp filling the entire left nasal cavity that was non-tender and did not bleed on touch and it could be probed all around except laterally. No paranasal sinuses tenderness was present. It was diagnosed to be left antrochoanal polyp clinically. Medical examination was essentially negative.
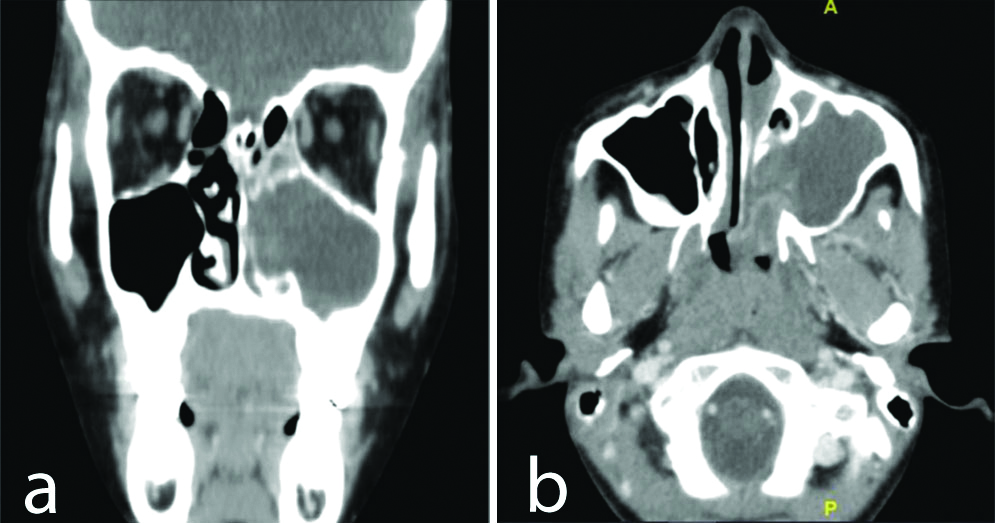
Contrast enhanced computerised tomography of the paranasal sinuses (2 mm coronal cuts) showed mucosal thickening with complete obliteration of left maxillary sinus with few hyperdense components and extending into left nasal cavity with widening of ethmoid infundibulum. The mass reached nasopharynx also on left side with few well enhancing areas in the choanal component suspecting angiomatous antrochoanal polyp. Remaining sinuses on left side showed soft tissue attenuating mucosal thickening with right side normal sinuses [Table/Fig-1a,b].
a) Left maxillary sinus showing mucosal thickening and complete obliteration with few hyperdense components with extension to left nasal cavity with widening of ethmoid infundibulum; b) Extension of left nasal mass into nasopharynx with well enhancing areas within the lesion.
The patient was planned for endoscopic polypectomy under general anaesthesia. Nasal endoscopy showed pinkish polypoidal mass arising from left middle meatus extending into choana. Endoscopic removal of mass was done. In view of mass arising from the anterolateral wall of left maxillary sinus, which could not be completely removed endoscopically, we proceeded to do Caldwell Luc approach and complete removal of mass was achieved.
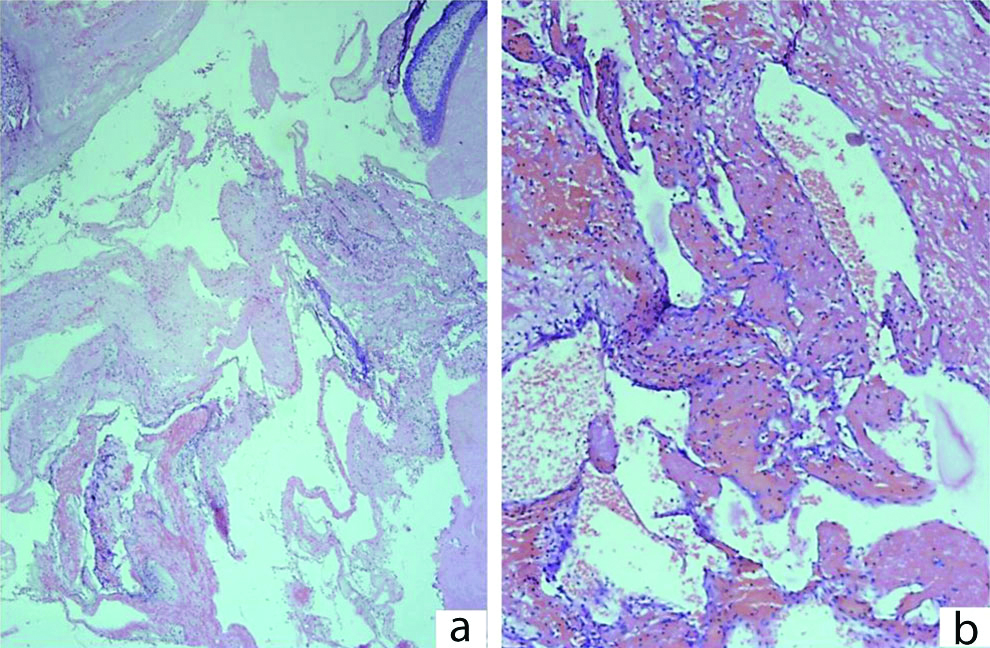
Histologically, it showed cavernous haemangioma with ecstatically dilated thin walled vascular channels with haemorrhage and fibrin thrombi [Table/Fig-2]. Thus, the final diagnosis was consistent with cavernous haemangioma of left maxillary sinus.
a) Section showing a polypoid fragment lined by respiratory epithelium with underlying subepithelial tissue showing ecstatically dilated vascular channel, H&E stain, 40X; b) Section showing a cavernous haemangioma with ecstatically dilated thin walled vascular channels with haemorrhage and fibrin thrombi, H&E stain, 400X.
Discussion
Haemangiomas are the most common vascular tumours of head and neck. But they are very rare entity to occur in paranasal sinuses [1]. Batsakis classified them as capillary, cavernous, mixed and proliferative [2]. They are benign non-epithelial vascular tumour composed of endothelial proliferation of blood vessels viz., benign, slow growing, non epithelial. They usually arise from turbinates and lateral wall of nasal cavity that grow in lateral direction [3]. They can arise from mucosal, ossesous or submucosal tissues of the nasal cavity or sinuses. The propensity of these tumours to cause bone erosion makes it difficult to differentiate them from more common malignant epithelial tumours on basis of radiology [3-7].
Evidence at birth is more than 75% but spontaneous involution occurs before adulthood. Haemangiomas involving nose and paranasal sinuses present typically in adults with 40 years as mean age at presentation with no sex prelediction [8,9]. Pathogenesis of haemangiomas is poorly understood. Rapid proliferation of pericytes and endothelial cell hyperplasia plays an important role followed by a steady regression phase [10].
Capillary haemangiomas occur mostly in children [7]. It involves mostly mucosal and submucosal tissues involving either nasal septum or vestibule [6]. Microscopically, capillary type is composed of lobules of capillary channels lined with flattened epithelium [1].
The International Society for the Study of Vascular Anomalies (ISSVA) describes cavernous haemangioma as pseudotumour anomalies [11]. Sinonasal cavernous haemangiomas occur predominatly in adults [7]. These can arise either from osseous tissue or mucosa. Non osseous are also reported involving either lateral wall of nasal cavity or medial wall of the maxillary sinus [7]. Macroscopically, they are well demarcated solitary lesions arising from medial wall of maxillary sinus or osteomeatal complex extending laterally [12]. Histologically, they are composed of large flattened endothelial lined vascular spaces in a lobular or diffuse pattern [12].
Engels T et al., was the first to describe such an entity and since then in literature, reported cases of maxillary sinus cavernous haemangioma are only few [13]. Hellquist HB stated that cavernous haemangiomas tend to arise from bony tissue of sinonasal tract and is enclosed by bony trabeculae [14]. Fu YS and Perzin KH described only five cases of cavernous haemangiomas out of 85 cases of vascular tumours involving nasal cavity, paranasal sinus and nasopharynx but none of them was located in maxillary sinus [15].
Clinical Presentation: Usually the clinical presentation include nasal obstruction, epistaxis and occasionally visible mass [16], cheek swelling [7], loosening of the maxillary teeth [17], epiphora [18], ear ache [19] and proptosis [6]. Clinically, they are locally aggressive and destructive by virtue of its pressure effect. They are not known to undergo malignant transformation. In this case, patient presented with epistaxis and nasal obstruction without any obvious erosion of sinus walls. So the diagnosis was made as antrochoanal polyp because of clinical signs and symptoms.
Kim HJ et al., reported erosion of wall of maxillary sinus, nasal turbinate and orbit in two cases of cavernous haemangioma [5]. There has been a report of cavernous haemangioma of sphenoid sinus and from infra orbital nerve canal [20].
Radiology: Contrast enhanced computed tomography shows non-homogenous enhancement due to local areas of necrosis and bleeding with focal areas of bone lysis. Bone destruction may be misinterpreted as a sign of malignancy [21]. Dystrophic calcification can also occur following intravascular thrombosis that results in the formation of phleboliths [22]. Weiss SW et al., reported amorphous or curvilinear calcification and phlebolith formation as non-specific and specific findings of cavernous haemangioma respectively [23].
Magnetic resonance imaging shows extensively dilated vessels and isointense on T1 and predominantly hyperintense on T2, compatible with low flow vascular structures [24].
Angiography is both a diagnostic and therapeutic investigation that reveals a hypervascular lesion with dilated feeding arteries and draining veins but stagnation of contrast agent and persistence of blush on late film are present with regular contour [6]. In this case, radiological diagnosis was made as angiomatous antrochoanal polyp because of hyperdense components and well enhancing areas in the nasal mass.
Differential Diagnosis: Since this patient presented with short history of unilateral epistaxis and nasal obstruction, it was diagnosed as antrochoanal polyp with exposure changes. This diagnosis was confirmed with radiology but with additional features of angiomatous changes.
Other differential diagnosis includes long standing sinonasal polyps [7], neuroma, inverted papilloma, polypoid cystic masses, mucoceles, pyogenic granuloma, organised haematoma, bacillary angiomatosis, Kaposi sarcoma and other vascular tumours of paranasal sinuses like angiosarcoma [6].
Treatment: Treatment includes complete removal of the mass with open or endoscopic method [25]. Open methods include medial maxillectomy using lateral rhinotomy or Weber Fergusson or Caldwell Luc surgery [26]. Both endoscopic and open methods had been used in this case for the complete removal.
Biopsy is contraindicated but it should be done with great care and appropriate preoperative planning under general anaesthesia [27]. Kim HJ et al., presented two cases with minimal bleeding because haemangiomas are venous malformations of small to medium sized vessels with low or non-arterial circulation [5]. Preoperative transarterial embolisation helps in decreasing the tumour size and haemorrhage during surgery. But in order to preserve adjacent vital structures, partial resection may also be accepted [6,25]. Laser excision, radiotherapy and steroid therapy have no role in the management of cavernous haemangioma [9].
Conclusion(s)
Cavernous haemangioma, though rare, usually presents with epistaxis and nasal obstruction. Haemangiomas in children may be confused with antrochoanal polyp as happened in the index case. Radiology, though helpful to some extent in making the diagnosis, histopathological examination gives the conclusive report. A high index of suspicion is needed to avoid extensive surgery and unnecessary morbidity. Though highly vascular tumours require embolisation preoperatively, endonasal resection without embolisation can be considered in selective cases of cavernous haemangioma. Treatment is the complete excision of the tumour and no recurrence has been reported following surgery.
Author Declaration:
Financial or Other Competing Interests: No
Was Ethics Committee Approval obtained for this study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 22, 2018
Manual Googling: Dec 03, 2019
iThenticate Software: Dec 24, 2019 (16%)
[1]. Jung WS, Yoo CY, Park YJ, Ihn YK, Hemangioma of the maxillary sinus presenting as a mass: CT and MR featuresIran J Radiol Q J Publ Iran Radiol Soc 2015 12(2):e692310.5812/iranjradiol.6923 [Google Scholar] [CrossRef]
[2]. Batsakis JG, Tumors of the head and neck: Clinical and pathological considerations 1979 BaltimoreWilliams & Wilkins:291-312. [Google Scholar]
[3]. Raboso E, Rosell A, Plaza G, Martinez-Vidal A, Haemangioma of the maxillary sinusJ Laryngol Otol 1997 111(7):638-40.10.1017/S00222151001381869282203 [Google Scholar] [CrossRef] [PubMed]
[4]. Kurihara K, Saiki T, Takeda K, Kobayashi J, Epithelioid hemangioma of the maxillary sinus: A case reportJ Oral Maxillofac Surg 1995 53(10):1221-23.10.1016/0278-2391(95)90641-X [Google Scholar] [CrossRef]
[5]. Kim HJ, Kim JH, Kim JH, Hwang EG, Bone erosion caused by sinonasal cavernous hemangioma: CT findings in two patientsAJNR Am J Neuroradiol 1995 16(5):1176-78. [Google Scholar]
[6]. Jammal H, Barakat F, Hadi U, Maxillary sinus cavernous hemangioma: A rare entityActa Otolaryngol (Stockh) 2004 124(3):331-33.10.1080/0001648031001568715141765 [Google Scholar] [CrossRef] [PubMed]
[7]. Vargas MC, Castillo M, Sinonasal cavernous haemangioma: A case reportDento Maxillo Facial Radiol 2012 41(4):340-41.10.1259/dmfr/8960156922517999 [Google Scholar] [CrossRef] [PubMed]
[8]. Osborn DA, Haemangiomas of the noseJ Laryngol Otol 1959 73(3):174-79.10.1017/S002221510005513413641866 [Google Scholar] [CrossRef] [PubMed]
[9]. Singhal SK, Singh C, Kumar R, Mohan H, Capillary hemangioma of the maxillary sinus: A case report review of literatureClin Rhinol Int J 2010 3(2):107-10.10.5005/jp-journals-10013-1039 [Google Scholar] [CrossRef]
[10]. Marchuk DA, Pathogenesis of hemangiomaJ Clin Invest 2001 107(6):665-66.10.1172/JCI1247011254664 [Google Scholar] [CrossRef] [PubMed]
[11]. Enjiolras O, Mulliken JB, Vascular tumors and vascular malformations (new issues)Adv Dermatol 1997 13:375-423. [Google Scholar]
[12]. Hamdan AL, Kahwaji G, Mahfoud L, Husseini S, Cavernous hemagioma of the maxillary sinus: A rare cause of epistaxisMiddle East J Anaesthesiol 2012 21(5):757-60. [Google Scholar]
[13]. Engels T, Schörner W, Felix R, Witt H, Jahnke V, Cavernous hemangioma of the maxillary sinusHNO 1990 38(9):342-44. [Google Scholar]
[14]. Hellquist HB, Pathology of the nose and paranasal sinuses 1990 LondonButterworth and Co. Ltd:136-42. [Google Scholar]
[15]. Fu YS, Perzin KH, Nonepithelial tumors of the nasal cavity, paranasal sinuses, and nasopharynx: A clinicopathologic studyCancer 1974 33(5):1275-88.10.1002/1097-0142(197405)33:5<1275::AID-CNCR2820330513>3.0.CO;2-4 [Google Scholar] [CrossRef]
[16]. Song CE, Cho JH, Kim SY, Kim SW, Kim BG, Kang JM, Endoscopic resection of haemangiomas in the sinonasal cavityJ Laryngol Otol 2009 123(8):868-72.10.1017/S002221510900486119275780 [Google Scholar] [CrossRef] [PubMed]
[17]. Cansiz H, Yener M, Kalekoglu N, Dalkiliç O, Arteriovenous malformation of the maxillary sinus and mandible: A case reportEar Nose Throat J 2003 82(8):608-10.:612:61410.1177/014556130308200816 [Google Scholar] [CrossRef]
[18]. Naraghi A, Keene M, Maxillary intraosseous vascular malformation: A case report and literature reviewJ Laryngol Otol 2007 121(4):404-07.10.1017/S002221510700456217403266 [Google Scholar] [CrossRef] [PubMed]
[19]. Mussak E, Lin J, Prasad M, Cavernous hemangioma of the maxillary sinus with bone erosionEar Nose Throat J 2007 86(9):565-66.10.1177/01455613070860091217970148 [Google Scholar] [CrossRef] [PubMed]
[20]. Walch C, Anderhuber W, Luxenberger W, Humer-Fuchs U, Cavernous haemangioma in the infraorbital nerve canal- An unusual expansion in the maxillary sinusJ Laryngol Otol 1998 112(9):872-74.10.1017/S00222151001419339876381 [Google Scholar] [CrossRef] [PubMed]
[21]. Kargi E, Babuccu O, Hoşnuter M, Babuccu B, Hemangioma of the nasal bone: A case reportKulak Burun Bogaz Ihtis Derg KBB J Ear Nose Throat 2005 14(1-2):32-34. [Google Scholar]
[22]. Bektas D, Ural A, Cobanoglu U, Arslan S, Caylan R, Cavernous hemangioma of maxillary sinus in an adult mimicking carcinoma: A case reportKBB-Forum 2008 7(1):43-45. [Google Scholar]
[23]. Weiss SW, Enzinger FM, Goldblum JR, Enzinger and weiss’s soft tissue tumors 2008 305th ed(6)LouisMosby:75410.1097/01.shk.0000336211.13924.d4 [Google Scholar] [CrossRef]
[24]. Zaki Z, Ouattassi N, Oudidi A, Cavernous haemangioma of the maxillary sinusOtolaryngol 2008 94:387-90. [Google Scholar]
[25]. Sciarretta V, Pasquini E, Farneti G, Frank G, Mazzatenta D, Calbucci F, Endoscopic sinus surgery for the treatment of vascular tumorsAm J Rhinol 2006 20(4):426-31.10.2500/ajr.2006.20.288816955773 [Google Scholar] [CrossRef] [PubMed]
[26]. Kanazawa T, Inoue R, Ohta Y, Watanabe Y, Iino Y, Maxillary haemangioma successfully resected by endoscopic approachJ Laryngol Otol 2009 123(7):793-95.10.1017/S002221510800307118577272 [Google Scholar] [CrossRef] [PubMed]
[27]. Lightbody KA, Wilkie MD, Luff DA, Capillary haemangioma of the ethmoid sinusBMJ Case Rep 2013 2013:bcr201300869510.1136/bcr-2013-00869523580674 [Google Scholar] [CrossRef] [PubMed]