Hyponatremia-Associated Troublesome Hiccups: A Report of Rare Manifestation: A Review
Kuan Yee Lim1, Khairul Najmi Muhammad Nawawi2
1 Department of Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Cheras, Kuala Lumpur, Malaysia.
2 Gastroenterology Unit, Department of Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Cheras, Kuala Lumpur, Malaysia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Khairul Najmi Muhammad Nawawi, Level 8, Clinical Block, Universiti Kebangsaan Malaysia Medical Centre, Cheras, Kuala Lumpur, Malaysia.
E-mail: khairulnajmi84@gmail.com
Hiccup is an intermittent spasmodic contraction of the diaphragm, which is usually a benign and self-limiting condition. However, persistent hiccups may indicate a more sinister underlying pathology. Hiccups have been reported in the literature as an unusual manifestation in hyponatremia. Some literature had linked the severity of hiccups to the level of serum sodium. Present case report is of persistent hiccups, seen in a 60-year-old male patient who presented with serum sodium of 100 mmol/L. Apart from the troublesome hiccups, he had associated dizziness, unsteady gait and poor oral intake. His hiccups resolved after correction of serum sodium above 124 mmol/L. The dose-response relationship between hyponatremia and hiccups vary in different individuals. A fluoroscopic examination can be considered in cases of hiccups or hyponatremia to conclude the association between both.
Hydrochlorothiazide, Sodium, Symptomatic
Case Report
A 60-year-old male patient presented with a three day history of dizziness, unsteady gait, nausea and vomiting, and poor oral intake. He was noted to have unusually troublesome hiccups since two days prior to the admission, which occurred every minute, continuously throughout the day and affecting his appetite.
He was hypertensive and on hydrochlorothiazide for past one year, type 2 diabetes mellitus with retinopathy and nephropathy, and dyslipidemia. He had evisceration of left eye due to industrial injury many years ago.
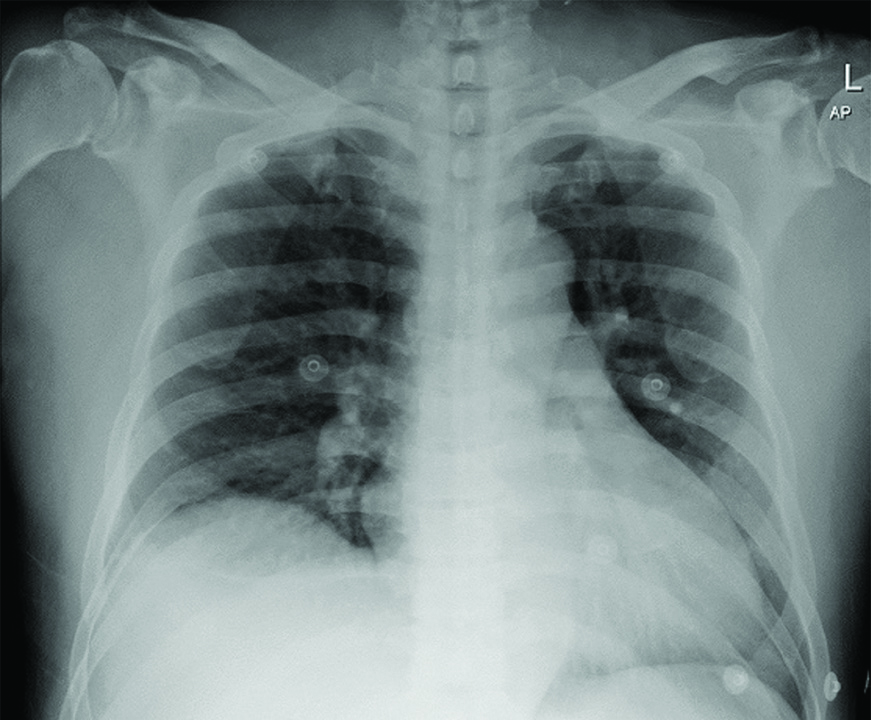
Upon presentation, his conscious level was full and orientated (Glasgow Coma Scale of 15), with normal vital signs. His respiratory examination revealed normal vesicular sounds with mild reduction of breath sounds over the right lower zone. The rest of the physical examination was normal. Chest radiograph showed raised right hemidiaphragm with clear lungs field [Table/Fig-1]. Baseline blood investigations, full blood count and renal profile were done. The renal profile showed severe hyponatremia with a sodium level of 100 mmol/L. Otherwise, the full blood count was normal.
Plain chest radiography on admission showing raised right hemidiaphragm.
His hydrochlorothiazide was withheld during the admission. Hypertonic saline 3% infusion was given over three hours and he was then put on intravenous infusion of normal saline 0.9% as maintenance for another four days with frequent monitoring of serum sodium daily. Dizziness and unsteady gait resolved on day three of admission, however, he had persistent troublesome hiccups in the ward, not resolving despite intravenous metoclopramide and oral itopride.
In view of persistent hiccups in the ward and the chest radiograph finding, ultrasonography of the abdomen was done on day three of admission to look for structural abnormalities of the diaphragm. The amplitude of movement over right diaphragm was noted to be lower compared to the left. Otherwise, there was no mass or lesion noted. Computed tomography and magnetic resonance imaging of the brain were also done. These were performed in order to rule out posterior circulation infarct in view of giddiness with mild ataxic gait, which showed no abnormality with no evidence of posterior circulation infarct or demyelination.
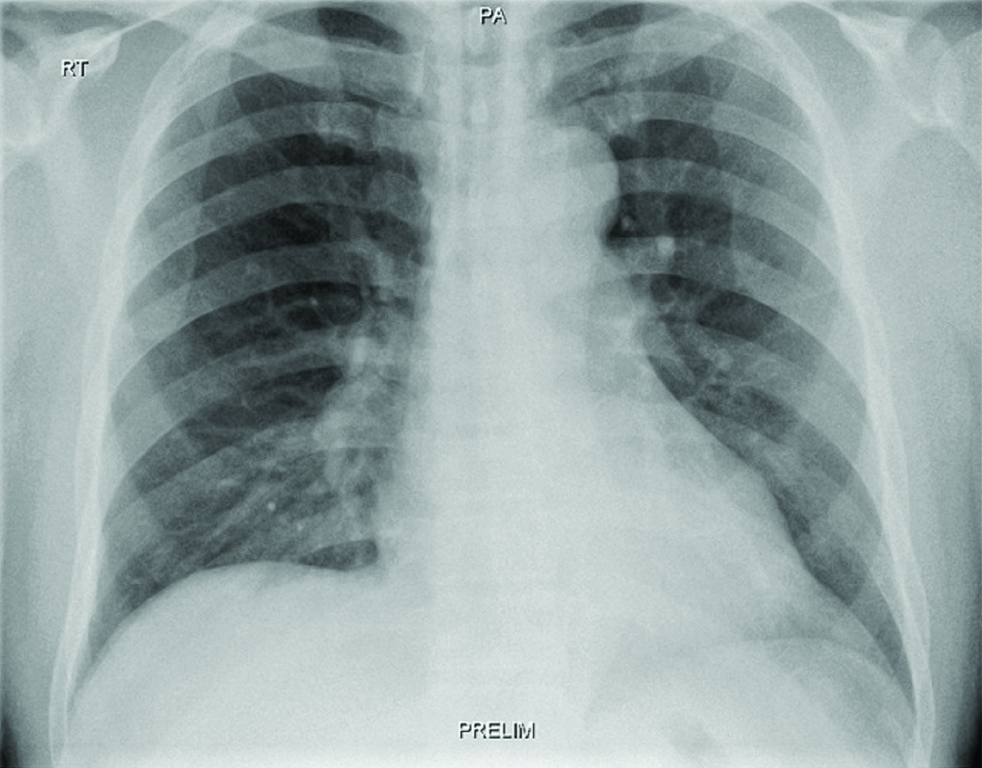
Serum sodium was increased by 3-4 mmol/L per day for the first two days, then 8-9 mmol/L per day subsequently [Table/Fig-2]. On day four of normal saline 0.9% maintenance, his hiccups had resolved, and serum sodium was noted to be 124 mmol/L. Upon discharge, his serum sodium was 130 mmol/L. He was planned for a fluoroscopic diaphragmatic sniff test two weeks later which was reported as normal [Table/Fig-3].
Serial chart for serum sodium monitoring.
| Day of admission | Serum Sodium (mmol/L) | Remarks |
|---|
| Day 1 | 100103 | Bolus Hypertonic Saline 3%Normal Saline 0.9% |
| Day 2 | 105107 | Normal Saline 0.9% |
| Day 3 | 110 | Normal Saline 0.9% |
| Day 4 | 115 | Normal Saline 0.9% |
| Day 5 | 124 | Hiccups resolved |
| Day 6 | 128 | |
| Day 7 | 130 | |
Chest fluoroscopy 2 weeks after discharge showing normal diaphragm.
Discussion
Hiccup is an intermittent spasmodic contraction of the diaphragm, often accompanied by similar contraction of the accessory muscles of inspiration [1]. Hiccups can be more precisely defined by noting the episode’s duration as described by Kolodzik PW and Eilers MA, into hiccup bouts, persistent or protracted hiccups, and intractable hiccups. Hiccup bout is an episode of several hiccups in less than 48 hours. Persistent or protracted hiccups last more than 48 hours. Hiccups lasting longer than one month are considered intractable [2,3]. Benign self-limited hiccups are usually precipitated by gastric distention without organic disease. However, persistent or intractable hiccups, on the other hand, suggest an underlying organic cause [4].
Hyponatremia is defined as serum sodium <135 meq/L, and usually manifests when serum sodium level <120 mmol/L, as neurological symptoms such as headache, nausea, vomiting, drowsiness and seizures [5]. Hiccups is a rare manifestation of hyponatremia and a few cases had been reported previously [6-10].
Hyponatremia is commonly presented with lethargy, headache, nausea, vomiting, or seizures/coma in severe cases. A study by Patni M et al., involving 100 patients with hyponatremia admitted to an intensive care unit, found that the severity of hyponatremia correlated with the severity of symptoms. The severity was classified into severe (<114 mmol/L), moderate (115-124 mmol/L), and mild (>125 mmol/L). The study also revealed that hiccups contributed to 10% of the symptoms for hyponatremia, besides drowsiness, vomiting and seizure [11].
Possible causes of hiccups include psychogenic and organic causes involving different major organs. Simple irritations such as gastric distension may occasionally produce brief, transient hiccups; however, more intense stimuli from myocardial infarction, peritonitis, metabolic disorders may produce persistent or intractable hiccups [12]. In this case of discussion, possible organic causes such as sub-phrenic collection or irritation and posterior cerebral circulation infarct were ruled out with radiographic investigations. His troublesome hiccups that resolved after correction of hyponatremia, showed an association between hyponatremia and hiccups. Hyponatremia and hiccups were found to have a dose-response relationship as demonstrated by a case-control study performed by George J et al., which showed that for every 10mEq/L reduction in serum sodium, patients were 17 times at risk of developing hiccups [12].
There is no specific cut-off level of hyponatremia that triggers hiccups. Cronin RE, did an observation on 11 cases of psychogenic polydipsia that had symptomatic hyponatremia. Three out of 11 patients have chronic recurrent intractable hiccups with nausea, vomiting, and lethargy. The serum sodium on admission for symptomatic hyponatremia ranges from 101 to 119 mmol/L. The serum sodium following recovery ranges from 129 to 142 mmol/L [13].
There is no known mechanism on how hyponatremia causes hiccups. However, a 10 year review of anatomy, aetiology, and treatment of hiccup done by Samuels L, revealed that there are contraction differences in hiccup spasm based on a routine repeated fluoroscopic examination of patients with hiccups [14]. Fluoroscopy is the best modality of imaging to visualise contraction or spasm of the diaphragm [15]. In this case, the presence of raised right hemidiaphragm in the chest radiography during admission might be suggestive of a unilateral contraction of the diaphragm with complete or incomplete spasm; as supported by the abdominal ultrasonographic finding of the reduced amplitude of right hemidiaphragm. Unfortunately, the fluoroscopy was only done after the resolution of symptom and noted to be normal.
Conclusion(s)
Hiccups can be a manifestation of hyponatremia. No specific level of serum sodium has been reported for the development or resolution of hiccups. The dose-response relationship between hyponatremia and hiccups vary in different individuals. A fluoroscopic examination can be considered in cases of hiccups or hyponatremia to conclude the association between both. We postulated that severe hyponatremia might cause the raised right hemidiaphragm which then led to persistent hiccups. Further studies are needed to scientifically investigate this possible mechanism.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 13, 2019
Manual Googling: Dec 07, 2019
iThenticate Software: Dec 24, 2019 (11%)
[1]. Hardo PG, Intractable hiccups-an early feature of Addison’s diseasePostgrad Med J 1989 65(770):918-19.10.1136/pgmj.65.770.9182616432 [Google Scholar] [CrossRef] [PubMed]
[2]. Kolodzik PW, Eilers MA, Hiccups (singultus): Review and approach to managementAnn Emerg Med 1991 20(5):565-73.10.1016/S0196-0644(05)81620-8 [Google Scholar] [CrossRef]
[3]. Chang FY, Lu CL, Hiccup: Mystery, nature and treatmentJ Neurogastroenterol Motil 2012 18(2):123-30.10.5056/jnm.2012.18.2.12322523721 [Google Scholar] [CrossRef] [PubMed]
[4]. Friedman NL, Hiccups: A treatment reviewPharmacotherapy 1996 16(6):986-95. [Google Scholar]
[5]. Sahay M, Sahay R, Hyponatremia: A practical approachIndian J Endocrinol Metab 2014 18(6):760-71.10.4103/2230-8210.14132025364669 [Google Scholar] [CrossRef] [PubMed]
[6]. Jones JS, Lloyd T, Cannon L, Persistent hiccups as an unusual manifestation of hyponatremiaJ Emerg Med 1987 5(4):283-87.10.1016/0736-4679(87)90256-3 [Google Scholar] [CrossRef]
[7]. Ramirez FC, Graham DY, Hiccups, compulsive water drinking and hyponatremiaAnn Intern Med 1993 118(8):64910.7326/0003-4819-118-8-199304150-000208452336 [Google Scholar] [CrossRef] [PubMed]
[8]. Lazarevic V, Hagg E, Wahlin A, Hiccups and severe hyponatremia associated with high-dose cyclophosphamide in conditioning regimen for allogenic stem cell transplantationAm J Hematol 2007 82(1):85-88.10.1002/ajh.2070616917917 [Google Scholar] [CrossRef] [PubMed]
[9]. Goyal A, Mehmood S, Mishra S, Bhatnagar S, Persistent hiccups in cancer patient: A presentation of syndrome of inappropriate antidiuretic hormone induced hyponatremiaIndian J Palliat Care 2013 19(2):110-12.10.4103/0973-1075.11671224049353 [Google Scholar] [CrossRef] [PubMed]
[10]. Gardecki J, Espinosa J, Lucerna A, Bernhardt J, Singultus: Avoiding a hiccup in careAm J Emerg Med 2017 35(6):938:e1-938.e3.10.1016/j.ajem.2016.12.05628041755 [Google Scholar] [CrossRef] [PubMed]
[11]. Patni M, Humaney NR, Jeswani J, Deoke SA, Clinico-etiological profile of hyponatremia in patients admitted in intensive care unit of tertiary health care rural centerJournal of Medical Science and Clinical Research 2015 3(8):6975-82.10.18535/jmscr/v3i8.12 [Google Scholar] [CrossRef]
[12]. George J, Thomas K, Jeyaseelan L, Peter JV, Cherian AM, Hyponatremia and hiccupsNatl Med J India 1996 9(3):107-09. [Google Scholar]
[13]. Cronin RE, Psychogenic polydipsia with hyponatremia: Report of eleven casesAm J Kidney Dis 1987 9(5):410-16.10.1016/S0272-6386(87)80144-0 [Google Scholar] [CrossRef]
[14]. Samuels L, Hiccup: A ten year review of anatomy, etiology, and treatmentCan Med Assoc J 1952 67(4):315-22. [Google Scholar]
[15]. Minami T, Manzoor K, McCool FD, Assessing diaphragm function in chest wall and neuromuscular diseasesClin Chest Med 2018 39(2):335-44.10.1016/j.ccm.2018.01.01329779593 [Google Scholar] [CrossRef] [PubMed]