Uterine Artery Embolization: A Boon for a Near Miss Case of Pseudoaneurysm
Anam Khan1, Neema Acharya2, Mahima Koshatwar3, Janhvi Sabnis4, Akshayata Sorte5
1 Junior Resident, Department of Obstetrics and Gynaecology, DMIMSDU, Wardha, Maharashtra, India.
2 Professor and Head, Department of Obstetrics and Gynaecology, DMIMSDU, Wardha, Maharashtra, India.
3 Undergraduate Student, DMIMSDU, Wardha, Maharashtra, India.
4 Undergraduate Student, DMIMSDU, Wardha, Maharashtra, India.
5 Undergraduate Student, DMIMSDU, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Neema Acharya, AF 5, Doctors Quarters, AVBR Hospital Campus, DMIMSDU, Sawangi Meghe, Wardha-442001, Maharashtra, India.
E-mail: neemasacharya@gmail.com
One of the unusual causes of secondary postpartum haemorrhage is Uterine Artery Pseudoaneurysm (UAP) and is associated with high mortality rate. Authors report a case of 26-year-old female who had secondary postpartum haemorrhage due to left UAP after caesarean section. Transcatheter arterial embolization is safe and beneficial for managing postpartum haemorrhage resulting from pseudoaneurysm. Angiographic embolization was done for the pseudoaneurysm in this patient successfully. Hence, reporting this case to highlight the availability of transcatheter arterial embolization as a treatment option in UAP before going for surgery in favourable cases.
Secondary postpartum haemorrhage, Transcatheter arterial embolization, Uterine artery pseudoaneurysm
Case Report
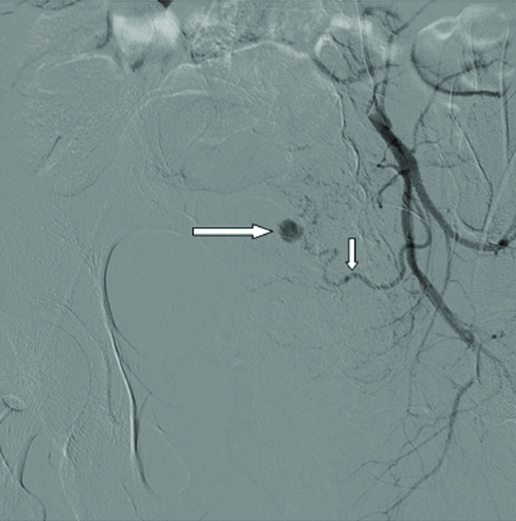
A 26-year-old para 1 living 1 was received in the Emergency Department on postpartum day 28 with symptoms of profuse bleeding per vaginum. She had undergone caesarean section for non-reassuring cardiotocography. The immediate and early postoperative periods were uneventful and patient was discharged home on 7th postoperative day. Patient had two episodes of bleeding per vaginum, one each in 2nd and 3rd week of postpartum period. The pelvic sonography revealed normal findings. This episode could be managed with dilatation and curettage, along with oxytocins and antibiotics. There were no retained products of conception. In the 4th week of postpartum period patient presented with sudden onset of profuse bleeding per vaginum. The bleeding was arrested temporarily by putting uterine balloon (Bakri balloon) for uterine tamponade. Ultrasound of pelvis showed normal sized uterus with 4×4 cm haematoma on the anterior wall of uterus. Magnetic Resonance Imaging (MRI) was done which showed evidence of haematoma posterior to the urinary bladder with cluster of abnormal vascularity seen within. It was suggestive of pseudoaneurysm of uterine artery. Hence, she was referred to our institute for further care. At the time of admission, she was in a state of obstetric haemorrhagic shock having tachycardia and hypotension and looked pale. Her haemoglobin was 6.1 gm%. After initial management of haemorrhagic shock with one unit of blood transfusion and two units of fresh frozen plasma, patient was taken for interventional radiological procedure. Pelvic angiography revealed pseudoaneurysm from left uterine artery as seen in [Table/Fig-1].
It shows pseudoaneurysm of left uterine artery. Long arrow is pointing the pseudoaneurysm, short arrow is pointing the left uterine artery.
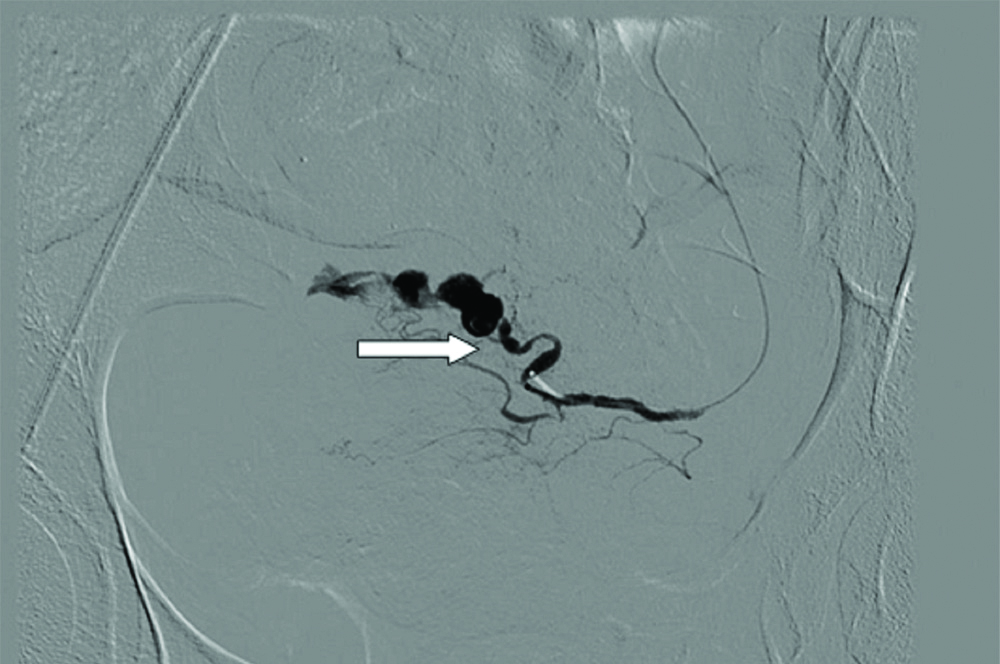
The left uterine artery was selectively embolized by using histocryl glue mixed with lipiodol as seen in [Table/Fig-2]. The bleeding stopped immediately. The right uterine artery showed no abnormal bleeding. Her immediate and early post-procedure periods were uneventful and patient was discharged on 5th post-procedure day. At present six months after treatment, patient is menstruating normally and not having any menstrual or gynaecologic complaint. The ultrasound of the pelvis done during follow-up revealed normal findings. MRI scan was not repeated due to cost issue.
It shows angiographic picture of left uterine artery pseudoaneurysm after embolization. Arrow is showing the block created by the histocryl glue and lipoidol mixture.
Discussion
Postpartum haemorrhage is defined as cumulative blood loss greater than 1000 mL with signs and symptoms of hypovolemia within 24 hours of the birth process, regardless of the route of delivery. The condition can occur up to six weeks following delivery [1]. Postpartum haemorrhage, occurring within first 24 hours of delivery is called as primary or early postpartum haemorrhage, while secondary or delayed postpartum haemorrhage is defined as bleeding occurring after 24 hours post delivery within six weeks, having blood loss of 500 mL or more [2]. Even with proper obstetric care, almost 3% of vaginal deliveries will cause severe postpartum haemorrhage.
Secondary postpartum haemorrhage results due to retained products of conception, endometritis, placental bed sub involution, arteriovenous malformations, choriocarcinoma and pseudoaneurysm of uterine artery [3]. The occurrence of an arterial pseudoaneurysm is rare but not uncommon, as it develops after vascular trauma during common obstetric surgery like caesarean section or after uterine curettage [4]. A pseudoaneurysm results when blood accumulates between the layers of a vessel wall with turbulent flow which is in communication with the parent vessel via an inadequacy in the arterial wall. The reported incidence of UAP aneurysm is 0.2%-0.4% approximately in women of reproductive age group [5].
With advances in radioimaging technology, it is diagnosed easily using both Doppler sonography and arteriography. Hence the incidence of this entity is increasing. With the availability of intervenional radiological procedures as therapeutic modality, postpartum haemorrhage due to psedoaneurysm can be managed conservatively. Thereby, it has added benefit of avoiding surgical intervention and preservation of fertility [3].
UAP is seen as a pulsatile hypoechoic mass attached to an artery. Colour Doppler ultrasound findings are turbulent arterial flow, to and fro, yin and yang sign that occurs due to the flowing blood into the pseudoaneurysm in systole and backward flow during diastole. The findings on Computed Tomography (CT) scan are round pelvic mass showing similar enhancement like arteries in arterial phase. Active extravasation can also be demonstrated on CT scan. Angiography is the gold standard for diagnosis as it also helps in identifying active extravasation [6].
The primary treatment of a ruptured UAP is similar to treatment of any haemorrhagic shock. Resuscitation is done by obtaining large bore intravenous access and by administering crystalloid and blood products. Until we achieve definite treatment, we can do vaginal packing or uterine balloon tamponade. In present case, we used uterine tamponade with Bakri balloon to arrest bleeding temporarily.
Uterine Artery Embolization (UAE), typically the preferred method of management, is a safe and effective way to treat UAP [7]. Mostly in cases of profuse secondary postpartum haemorrhage with undiagnosed cause, surgical intervention is followed, after failure of conservative medical methods used to manage haemorrhage. Conservative surgical methods like step wise devascularisation spare the uterus and fertility but if bleeding persists, emergency total or sub-total hysterectomy becomes lifesaving [8].
With the emergence and expertise in the field of interventional radiology, ‘Transcatheter UAE’ is a promising minimally invasive procedure for management of postpartum haemorrhage [8]. It allows the preservation of fertility and menstrual function and also avoids short and long term effects of surgery or hysterectomy on quality of life of these young women of reproductive age group. With the rising trend of caesarean section in modern obstetrics, UAP is likely to be common and should be kept in mind as a cause of secondary postpartum haemorrhage [3].
The success rate of UAE to arrest postpartum haemorrhage in such cases is 97%. There are several advantages of UAE as enumerated below,
Exact bleeding site is identifiable.
Repetition of embolization if required can be easily done.
It does not preclude any haemorrhage control measures.
General anaesthesia is avoided.
It is a fertility conserving procedure.
Angiography aids in finding out the site of pseudoaneurysm. Unilateral embolization is sufficient but sometimes if bleeding continues, bilateral embolization can be done due to redistribution of blood from opposite side uterine artery [9].
Eriksson LG et al., examined the safety of UAE for patients with postpartum haemorrhage from multiple causes. In their series out of 20 cases, three had UAP and all of them achieved haemostasis without complications [10]. A study by Choi YH et al., showed 90% effectiveness of UAP and 10% complication rate [11]. In the present case, UAE was life saving for a young woman, and a near miss case of secondary postpartum haemorrhage due to UAP.
Conclusion(s)
Pseudoaneurysm is one of the main causes of secondary postpartum haemorrhage which should be kept in mind with history of caesarean section. With the increasing expertise and safety of minimally invasive radiological procedures, such cases can be managed conservatively without the need of surgical exploration or hysterectomy. Timely diagnosis with MRI and UAE along with emergency obstetric care to treat shock is key steps to be followed for management of this condition. Every obstetric tertiary health care center should consider developing interventional radiology unit at their hospital as it is minimally invasive and lifesaving procedure for such near miss cases.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 03, 2019
Manual Googling: Dec 05, 2019
iThenticate Software: Dec 24, 2019 (13%)
[1]. Anderson JM, Etches D, Prevention and management of postpartum hemorrhageAm Fam Physician 2007 75(6):875-82. [Google Scholar]
[2]. Pelage JP, Fohlen A, Le Pennec V, Role of arterial embolization in the management of postpartum hemorrhageJ Gynecol Obstet Biol Reprod. (Paris) 2014 43(10):1063-82. [Google Scholar]
[3]. Subramaniam S, Nadarajan C, Aziz ME, Role of uterine artery embolization in pseudoaneurysm of uterine artery: A rare cause of secondary postpartum HemorrhageCureus 2018 10(2):e222010.7759/cureus.222029692958 [Google Scholar] [CrossRef] [PubMed]
[4]. Nanjundan P, Rohilla M, Raveendran A, Jain V, Khandelwal N, Pseudoaneurysm of uterine artery: A rare cause of secondary postpartum hemorrhage, managed with uterine artery embolisationJ Clin Imaging Sci 2011 1:14 [Google Scholar]
[5]. Baba Y, Matsubara S, Kuwata T, Ohkuchi A, Usui R, Saruyama M, Uterine artery pseudoaneurysm: Not a rare condition occurring after nontraumatic delivery or non-traumatic abortionArch Gynecol Obstet 2014 290(3):435-40.10.1007/s00404-014-3226-424691826 [Google Scholar] [CrossRef] [PubMed]
[6]. Yeniel AO, Ergenoglu AM, Akdemir A, Eminov E, Akercan F, Karadadaş N, Massive secondary postpartum hemorrhage with uterine artery pseudoaneurysm after cesarean sectionCase Rep Obstet Gynecol 2013 2013:28584610.1155/2013/28584623653875 [Google Scholar] [CrossRef] [PubMed]
[7]. Jennings L, Presley B, Krywko D, Uterine artery pseudoaneurysm: A life threatening cause of vaginal bleeding in the emergency departmentJ Emerg Med 2019 56(3):327-31.10.1016/j.jemermed.2018.12.01630685218 [Google Scholar] [CrossRef] [PubMed]
[8]. Ratnam LA, Gibson M, Sandhu C, Torrie P, Chandraharan E, Belli AM, Transcatheter pelvic arterial embolisation for control of obstetric and gynaecological haemorrhageJ Obstet Gynaecol 2008 28(6):573-79.10.1080/0144361080227337419003648 [Google Scholar] [CrossRef] [PubMed]
[9]. Chitra TV, Panicker S, Pseudoaneurysm of uterine artery: A rare cause of secondary postpartum hemorrhageJ Obstet Gynaecol 2011 61(6):641-44.10.1007/s13224-011-0096-623204681 [Google Scholar] [CrossRef] [PubMed]
[10]. Eriksson LG, Mulic-Lutvica A, Jangland L, Nyman R, Massive postpartum hemorrhage treated with transcatheter arterial embolization: Technical aspects and long term effects on fertility and menstrual cycleActa Radiol 2007 48(6):635-42.10.1080/0284185070137068317611871 [Google Scholar] [CrossRef] [PubMed]
[11]. Choi YH, Baba Y, Ikeda S, So YH, Hayashi S, Nakajo M, Efficacy of uterine artery embolization for patients with postpartum hemorrhageOpen J Radiol 2013 3(2):51-55.10.4236/ojrad.2013.32008 [Google Scholar] [CrossRef]