Spinal epidural lipomatosis is a rare condition that occurs due to pathological overgrowth of normal spinal extradural fat with subsequent canal narrowing and cord impingement. The condition may be idiopathic or iatrogenic. A strong aetiological association with prolonged exogenous steroid administration has been described. On the other hand, obesity is known to be a cause of idiopathic spinal epidural lipomatosis. We present the radiological picture that led to the diagnosis of iatrogenic epidural lipomatosis induced by exogenous steroid administration in young child post-meningitis. Present case is unusual because exogenous steroid administration that led to abnormal fat proliferation was one time for a short duration of less than a week, unlike other cases reported in literature where epidural lipomatosis has developed in patients on long term steroid therapy.
Cord compression, Epidural fat deposition, Iatrogenic, Magnetic resonance imaging
Case Report
A three-year-old child presented with bilateral lower limb pain and weakness of three months duration. The patient gave a history of fever with altered consciousness three months preceding this presentation for which he had been hospitalised. A diagnosis of pyogenic meningitis had been arrived based on CSF findings, and for therapeutic management of meningitis, he had received intravenous hydrocortisone along with oral antibiotics (Augmentin 5 mL thrice a day) during his hospital stay. The dose of hydrocortisone had been 2 mg intravenously twice a day for five days. The patient was discharged on the 6th day as the symptoms of meningitis and fever resolved.
He had been advised 1 mg oral prednisolone once a day for four weeks at the time of discharge and called for follow-up after a month, the dose of prednisolone was halved and tapered to 0.5 mg per day for another two weeks and thereafter discontinued. The child developed lower limb weakness three months after the initial illness and was referred by the physician for MRI of the dorsolumbar spine to ascertain the cause of paraparesis. The blood work-up at the current presentation revealed raised ESR (60 mm). The clinical and radiological suspicion was of an infective process, bacterial or viral, causing spinal subarachnoid involvement with cord compression or a malignant intradural mass lesion compressing the cord.
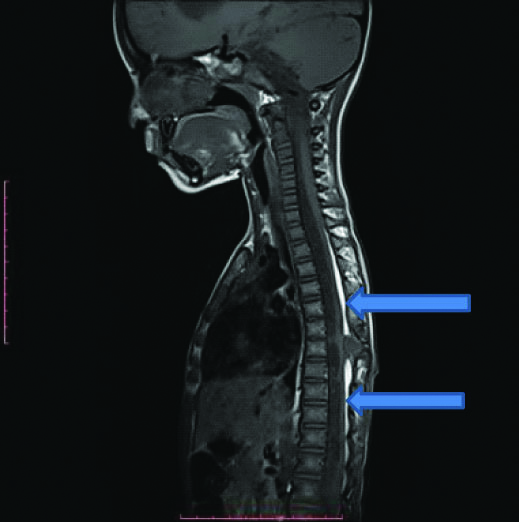
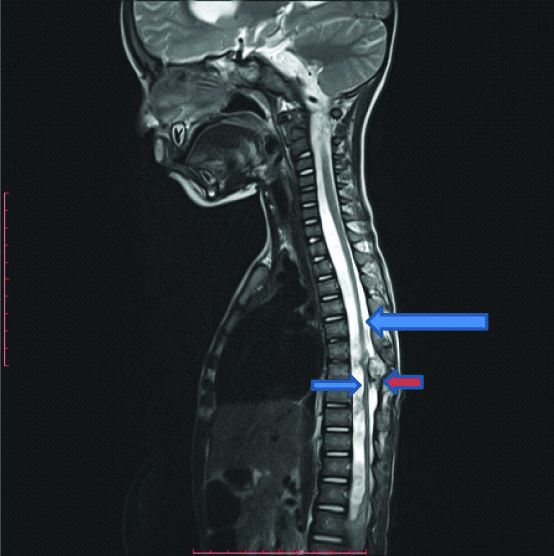
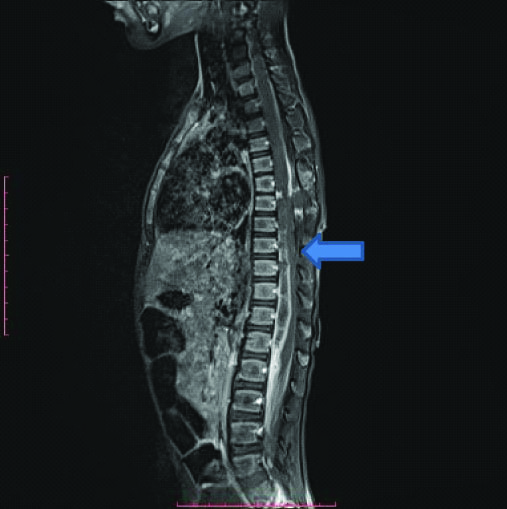
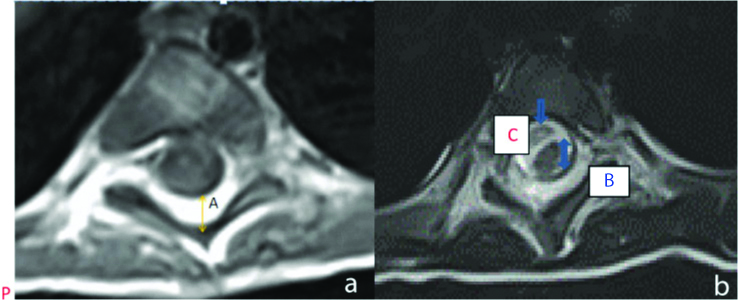
Sagittal MR of the dorsolumbar spine demonstrated un-encapsulated ill-marginated high-signal intensity images in the thoracic epidural space on both T1- and T2-weighted images, extending from D-1 to D-11 vertebral levels [Table/Fig-1a,b]. This abnormal hyper intensity was located in the posterior epidural compartment, occupying 50% of dorsal dural sac space, with displacement of the thoracic cord anteriorly. On fat saturated MR sequences, the abnormal tissue in the posterior epidural space demonstrated signal suppression indicating increased epidural fat content [Table/Fig-1c]. The Dural sac-fat ratio was found to be 1:2, with antero-posterior dimension of the abnormal dorsal epidural fat being 7 mm on axial MR image, and reduction of AP dimension of the Dural sac (3.5 mm) [Table/Fig-2a]. The dural sac appeared stellate in shape on axial images. In addition to the abnormal dorsal epidural fat content, the MR images demonstrated an enhancing epidural collection from D-6 to D-8 level without cord oedema or an osseous lesion [Table/Fig-2b]. MR findings enabled a diagnosis of epidural abscess with thoracic epidural lipomatosis. The epidural abscess was deemed to be the result of extension of meningitis and spread of infection to the spinal subarachnoid space, while the cause of bilateral lower limb weakness was cord compression by epidural fat proliferation.
T1 Weighted sagittal MR image shows abnormal linear continuous hyper intense signal in posterior epidural compartment of thoracic spine from D-1 to D-11 level (blue arrows), diagnostic of fat deposition.
T2 Weighted sagittal MR image shows hyper intense signal of fat in the posterior epidural thoracic region obscured by the CSF signal (blue arrows). A small heterogeneous epidural collection is also seen at D-9 level (red arrow).
Fat suppressed T1 Weighted sagittal image shows suppression of the T1 hyper intense signal (blue arrow) that was seen in dorsal epidural spine in [Table/Fig-1a], confirming presence of abnormal fat in the epidural thoracic posterior compartment.
Axial T2 and T1 Weighted MR Image shows fat percentage within thoracic spinal canal. The posterior epidural fat thickness in AP dimension, marked A in the figure, is 6mm while AP dimension of dural sac, marked B in the image, is 3.5 mm (dural sac/epidural fat ratio is 50%-1:2). The cord in the thecal sac is also seen indented by a small epidural collection marked C.
Discussion
Spinal epidural lipomatosis is an uncommon condition characterised by excessive proliferation and deposition of unencapsulated adipose tissue within the epidural space, which can cause compression of the spinal cord, nerve roots, or both. The condition is most common with long-term use of oral steroids or prolonged inhalation of steroids; however it has also been reported following a single epidural injection of corticosteroid [1]. It was first described in 1975 in a renal graft recipient who had been receiving exogenous steroids [2]. The mean dosage of oral steroids that can lead to abnormal fat deposition in unusual locations with development of clinical symptoms is stated to be 30-100 mg/day over 5-11 years [3]. Moreover, few cases have described marked epidural lipomatosis subsequent to intravenous administration of steroid for short duration. In this patient, methylprednisolone 1g/d i.v was given for three days followed by oral prednisone 1 mg/kg/day for a week and continued for one month at the dose of 30 mg/day (amounting to dose of >15 mg/day for body weight of 11 kg); along with methotrexate (0.5 mg/kg s.c. once weekly) and etanercept (25 mg s.c. once weekly). Due to the inability to taper the corticosteroids below 15 mg/day, at the end of this month, the patient developed swelling and increasing pain of the lower back, gained 11.5 kg, her Body Mass Index (BMI) increased from 20.7 (79th percentile) to 23.6 (95th percentile), and imaging demonstrated thoracic epidural lipomatosis [4].
Spinal epidural lipomatosis is known to result from excessive endogenous glucocorticoid production associated with endocrinopathies such as Cushing’s syndrome. Obesity has been found to be another aetiological factor, with endocrine dysfunction, deranged metabolism and abnormal fat deposition being interlinked. Epidural lipomatosis may be idiopathic with most patients of idiopathic epidural lipomatosis being obese males with a body mass index greater than 28 kg/m2 [5]. Thoracic spine is most commonly involved followed by the lumbosacral region. Presence of excessive fat in the thecal sac causes direct compression of the cord with paresis and progressive lower limb weakness [6]. Often chronic backache is the clinical presentation, the culprit factors being steroid induced osteoporosis compounded by osteoporotic vertebral collapse. Sensory loss, incontinence and ataxia may occur in advanced lipomatosis.
MRI is quintessential to make a diagnosis of spinal epidural lipomatosis since the neurologic examination in these patients is inconclusive [7]. Excessive un-encapsulated epidural fat shows the homogeneous high signal intensity typical of fat on T1 as well as T2-weighted images; and this signal is seen suppressed on STIR MR images [7]. Epidural lipomatosis is considered as a diagnosis when epidural fat thickness measures greater than 6 mm (range 7-16 mm). Epidural fat thickness measurement is obtained in sagittal MR images.
The normal mean thickness of epidural fat at the mid-thoracic level is 4.6 mm {range 3-6 mm); while in the cervical epidural compartment, normally no fat exists [8]. A small amount of unencapsulated fat normally surrounds the nerve roots, vessels and ligaments traversing the thoracic, lumbar and sacral epidural space, creating a cushioning effect.
Altered shape of the dural sac with reduced AP sac diameter is another MR feature that enables a diagnosis of epidural lipomatosis. Excessive fat proliferation alters the normal round shape of thecal sac which becomes polygonal, stellate, Y or V shaped. Three linear projections emanating from the central part of thecal sac like an inverted triangle on axial MR images (described as the Y sign) giving the thecal sac a stellate appearance, is considered a characteristic imaging finding of epidural lipomatosis [9]. This appearance is caused by the meningo-vertebral ligaments that anchor the outer dura to the vertebral body or to posterior longitudinal ligament anteriorly and to pedicles and laminae postero-laterally and is particularly seen in the lumbo-sacral region. In the thoracic spine, the shape of dural sac remains ovoid, and abnormal fat proliferation causes an antero-posterior flattening of the cord with effacement of subarachnoid space.
MRI enables assessment of extent of canal compromise by this unencapsulated abnormal quantity epidural fat. A system for grading epidural lipomatosis has been reported wherein the antero-posterior diameter of spinal canal, thecal sac and epidural fat are measured on axial MR scans. Epidural fat occupying less than 50% of the AP diameter of spinal canal is mild lipomatosis (Grade I), between 50- 75% is moderate (Grade II), while in severe (Grade III) lipomatosis, epidural fat occupies greater than 75% of the thecal sac [10]. The ratio of epidural sac diameter to amount of epidural fat in mild epidural fat proliferation is 1.0-1.5; ratio in moderate proliferation lies between 0.34-1.0; and is 0.33 or less in severe lipomatosis [11].
Included in the differential diagnosis are epidural lipomas, angiolipomas, extra adrenal spinal myelolipoma or methemoglobin containing haematomas, all of which appear as encapsulated masses, unlike the unencapsulated fat in epidural lipomatosis. Spinal liposarcoma is aggressive and tends to demonstrate muscle and bone invasion. The case reported is unique as epidural lipomatosis has developed even with short term administration of steroids given for meningitis.
Treatment of this unusual condition depends on the severity of neurologic manifestations. Decompressive debulking laminectomy with excision of the epidural fat is required in patients who have symptoms of cord compression, while conservative treatment options include weaning of steroids and weight reduction in obese persons [12]. However recovery may be immediate or slow.
Epidural lipomatosis can emerge as the unlikely aetiology of cord compression during MRI spine. MRI of spine enabled diagnosis of Grade 1 epidural lipomatosis as the cause of clinical symptoms of paraparesis in this patient. MRI is the modality of choice for evaluation of patients of compressive myelopathy. Older reports have suggested iatrogenic aetiology of this condition with prolonged corticosteroid administration resulting in fat accumulation in the spinal epidural space. However, even a single epidural injection of steroids, has been reported to be the rare trigger for abnormal fat deposition in epidural location [13].
The case being reported is unusual because although epidural lipomatosis has been reported to be a potentially serious untoward effect of chronic oral corticosteroid treatment more so in the paediatric population. We found a single case series where intravenous mode of steroid administration was found and development of epidural lipomatosis following shorter duration of steroid administration was reported with a mean 1.3 (±1.5) years (SD) (median, 0.8 years) of therapeutic steroids; within three weeks of corticosteroid treatment in patients of nephrotic syndrome, and within the first 18 months of treatment in (17/20) patients receiving steroids for various indications like organ transplantation, juvenile idiopathic arthritis, systemic lupus erythematosus, Crohn disease, Sjögren syndrome, Henoch-Schönlein purpura, pineoblastoma, and relapsing polychondritis [4]. Few reports are available where intravenous hydrocortisone administered in excessive dose over a shorter duration, resulted in epidural fat deposition and we found only one such case series [4].
It is therefore to be remembered that abnormal accumulation of fat in epidural compartment can be an unusual complication of any mode of steroid administration, oral, intravenous, transnasal or epidural, leading to clinical features of cord compression. The present case also shows that dose as well as duration of administration of exogenous steroid is equally important for intraspinal fat deposition to develop. In this patient, intravenous steroids had been administered for a short duration of five days, but the dose of hydrocortisone administered was definitely greater than that acceptable for the body weight, leading to development of epidural lipomatosis as a complication and cord compression was compounded by the epidural collection.
We want to highlight that the human body can respond adversely to exogenous steroids even with a single dose and dose regulation and management is extremely important; as is the awareness that rare aetiologies of spinal compression can be diagnosed effectively by MRI.
Conclusion(s)
Spinal epidural lipomatosis though rare per se, can develop in obese individuals and is an unusual complication of prolonged therapeutic steroid administration. Epidural lipomatosis is an unusual cause of canal stenosis and compressive myelopathy. The condition should be suspected when patients on long term steroids or those with excessive body mass and fat percentage present with features of cord compression. Abnormal fat in the epidural compartment had led to the clinical presentation of lower limb weakness in present patient. The diagnosis is based purely on imaging and MRI alone can detect this condition. Knowledge of this unusual condition is necessary for both radiologists and clinicians to make an accurate diagnosis and plan an adequate management of compressive myelopathy.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 28, 2019
Manual Googling: Dec 06, 2019
iThenticate Software: Dec 24, 2019 (11%)
[1]. Fogel GR, Cunningham PY, Esses SI, Spinal epidural lipomatosis: Case reports, literature review and meta-analysisSpine J 2005 5(2):202-11.10.1016/j.spinee.2004.05.25215795966 [Google Scholar] [CrossRef] [PubMed]
[2]. Lee M, Lekias J, Gubbay SS, Hurst PE, Spinal cord compression by extradural fat after renal transplantationMed J Aust 1975 1:201-03.10.5694/j.1326-5377.1975.tb111328.x1092979 [Google Scholar] [CrossRef] [PubMed]
[3]. Karageorgos A, Petsanas A, Gelalis I, Gkantaifis N, Aretha D, Idiopathic thoracic spinal epidural lipomatosis with relapsing and remitting symptomsThe Internet Journal of Orthopedic Surgery 2009 18(1):01-06.10.5580/2657 [Google Scholar] [CrossRef]
[4]. Möller JC, Cron RQ, Young DW, Girschick HJ, Levy DM, Sherry DD, Corticosteroid-induced spinal epidural lipomatosis in the pediatric age group: Report of a new case and updated analysis of the literaturePediatr Rheumatol Online J 2011 9:510.1186/1546-0096-9-521284882 [Google Scholar] [CrossRef] [PubMed]
[5]. Maillot F, Mulleman D, Mammou S, Goupille P, Valat JP, Is epidural lipomatosis associated with abnormality of body fat distribution? A case reportEur Spine J 2006 15:105-08.10.1007/s00586-005-0955-x16007467 [Google Scholar] [CrossRef] [PubMed]
[6]. Bushkar JB, MenkinSmith LP, Krywko DM, Idiopathic spinal epidural lipomatosis causing cauda equina syndromeClin Pract Cases Emerg Med 2017 1(4):305-08.10.5811/cpcem.2017.6.3477829849325 [Google Scholar] [CrossRef] [PubMed]
[7]. Pinkhardt EH, Sperfeld AD, Bretschneider V, Unrath A, Ludolph AC, Kassubek J, Is spinal epidural lipomatosis an MRI-based diagnosis with clinical implications?Acta Neurol Scand 2008 117(6):409-14.10.1111/j.1600-0404.2007.00964.x18081912 [Google Scholar] [CrossRef] [PubMed]
[8]. Kumar V, Singhora M, Agarwal AK, Spinal epidural lipomatosis-an enigmatic cause of back painSaudi J Med 2016 1(2):37-39. [Google Scholar]
[9]. Geers C, Lecouvet FE, Behets C, Malghem J, Cosnard G, Lengelé BG, Polygonal deformation of the dural sac in lumbar epidural lipomatosis: Anatomic explanation by the presence of meningovertebral ligamentsAm J Neuroradiology 2003 24(7):1276-82. [Google Scholar]
[10]. Borré DG, Borré GE, Aude F, Palmieri GN, Lumbosacral epidural lipomatosis: MRI gradingEur Radiol 2003 13(7):1709-21.10.1007/s00330-002-1716-412835988 [Google Scholar] [CrossRef] [PubMed]
[11]. Venkatanarasimha N, Parrish RW, Case 148: Thoracic epidural lipomatosisRadiology 2009 252(2):618-22.10.1148/radiol.252208036519703892 [Google Scholar] [CrossRef] [PubMed]
[12]. Beckworth WJ, McCarthy EJ, Garcia Corrada JE, Holbrook JF, Epidural lipomatosis and associated spinal stenosis-the impact of weight loss: A case reportAm J Lifestyle Med 2017 11(6):511-14.10.1177/155982761668676430202377 [Google Scholar] [CrossRef] [PubMed]
[13]. Choi KC, Kang BU, Lee CD, Lee SH, Rapid progression of spinal epidural lipomatosisEur Spine J 2012 21(4):408-12.10.1007/s00586-011-1855-x21667131 [Google Scholar] [CrossRef] [PubMed]