Neonatal Varicella is an uncommon disease in the Indian population, due to the presence of antibodies in the mother formed on the exposure to illness in their teenage in majority of population. The acquired varicella in newborn period, born to a non-immune mother shows a disseminated disease pattern with poor prognosis and high risk of mortality due to pneumonia, hepatitis, coagulopathy and secondary severe sepsis. The definite diagnosis is made by virus isolation or amplification of viral DNA from the skin lesions by PCR, but the clinical diagnosis from the pattern of rash hints the diagnosis well and appropriate. The drug of choice is intravenous acyclovir and Varicella Zoster Immune Globulin (VZIG), although the use of VZIG still remains debatable in symptomatic individuals.
Here, we present a case of a 15-day-old newborn with confluent maculo-papular rash preceded by rash in the mother at 10th day post-delivery. The newborn was managed in NICU with standard protocols, but the prognosis became poor due to complications that were pneumonia, hepatitis and secondary sepsis.
Hepatitis, Pneumonia, Sepsis, Varicella zoster immune globulin
Case Report
A 15-day-old baby presented with generalised confluent vesico-papular rash for two days [Table/Fig-1] and increasing respiratory distress since one day. The general condition and active feeding of the baby were deteriorating since last 12 to 14 hours.
Baby with generalised confluent vesico-papular rash.

Antenatal, perinatal and birth history were not significant. The mother had history of fever and rash at 10th day of post-natal period with healed crusted hyper-pigmented lesions on the day of presentation [Table/Fig-2]; clinically, simulating as chickenpox. Mother was never exposed to varicella infection before this ever in her life.
Mother with healed skin lesions of recent chickenpox.

On examination, baby was looking sick with severe respiratory distress. Her pulse rate was 160/min, respiratory rate was 70/min, SPO2 on room air was 80% and rectal temperature of 100°F was recorded. Following this, baby was intubated and put on a ventilator on Spontaneous Intermittent Mandatory Ventilation (SIMV) mode (Peak Inspiratory Pressure-12, Peak End Expiratory Pressure-5, Rate 50/min, FiO2 70%, Inspiratory: Expiratory ratio 1:2.4). A clinical diagnosis of Neonatal varicella with pneumonia and secondary sepsis was made. Investigations were followed and treatment was initiated with IV acyclovir, piperacillin, tazobactam, fluids with adequate sedation was also given. Varicella specific immunoglobulin was demanded but could not be availed due to its immediate shortage and high cost.
On investigations, TLC was 25,900/cumm with no significant differential count, there was significant thrombocytopenia (120,000/mm3) and deranged liver function tests (SGOT: 359 U/L and SGPT: 340 U/L). Radiological investigation of chest radiograph revealed an inhomogeneous opacity in the right upper and middle lobe [Table/Fig-3], which was not very characteristic of varicella pneumonia but that of a supervening bacterial infection as varicella complication. Lumbar puncture was also done with no significant interpretation.
Chest radiographs during the course of illness.
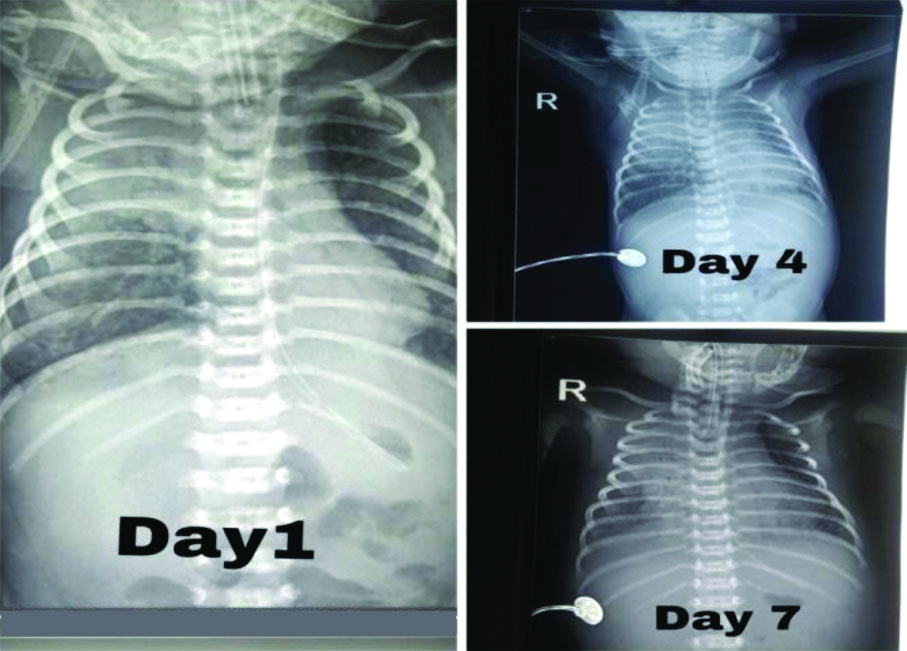
During the hospital stay of seven days; baby showed improvement on same ongoing treatment, following which ventilator settings were decreased but could not be tapered from SIMV mode. The repeat chest radiograph showed increase in the opacity [Table/Fig-3]; also the thrombocytopenia progressed to a count of 35000/mm3. The blood culture showed growth of Staphylococcus species sensitive to vancomycin which was added subsequently on day seven of hospital stay. The CSF culture showed no growth inferring no CNS infection.
On the last day (8th day) of the hospital stay baby developed bleeding diathesis evident in oro-gastric tube and endotracheal tube predicting a poor prognosis following which samples for assessment of bleeding profile (PT/INR, APTT, D-dimers) were withdrawn and a portable ultrasound of Skull and Abdomen was demanded, but the parents decided to leave against medical advice from the NICU care.
Discussion
Varicella is a highly infectious condition and poses extreme conditions to both mother and foetus if acquired during pregnancy. The usual incubation period for varicella is 14 days, with extreme of 10-28 days [1]. The infection has although became rare at the child bearing age in women because of its widespread immunisation during childhood and minimal circulation of wild type virus.
Congenital Varicella vs. Neonatal Varicella
The primary varicella zoster virus infection acquired during 8 to 26 weeks of gestation may lead to foetal varicella infection, of which some percentage of foetus develop congenital varicella syndrome with varied presentation at birth. Neonatal varicella per say can be presented either as a part of maternal infection who has acquired the infection five days prior to two days after delivery (perinatal infection) [2] or it can acquired post-natally by the baby i.e., after 12 days of post-natal life either by mother or any infected household contact. This indexed case is case of acquired neonatal varicella who presented at 13th day of life preceded by clinical diagnosis of Chicken pox in the mother at 10th day post-delivery. The severity of neonatal varicella varies depending on day of presentation i.e., late onset has severe disease than an earlier age which can be explained by the fact of maternal transmission of antibodies via the placenta if it is perinatal varicella infection. For cases, like the indexed one, an acquired neonatal varicella specially of a non-immune mother shows a severe and disseminated disease. The potentially fatal condition can be due to varicella pneumonia and haemorrhagic lesions over the liver and lung; which has been reported on autopsies by researches in late 90’s [3]. Although fatality has been reported around 20% when rash starts at-12 days of post natal life [4]. The typical finding in the varicella pneumonia is diffuse molted bronchopneumonia involving both the lung fields’ evidence on chest radiograph. In this case, the pneumonia was localised, unilateral and showed no improvement on treatment, which may be suggestive of secondary bacterial infection. The hepatic involvement in the disease process was evidenced with deranged liver function tests and bleeding on the last day of hospital stay in the index case. Gershon A also concluded in their literature that infant in whom varicella is fatal have a disseminated infection with pneumonia, extensive haemorrhagic skin vesicles, hepatitis and thrombocytopenia [5]. The platelet count in this case was also seen as a decreasing trend i.e., 1,20,000/cumm at day one to 35,000/cumm at day seven of hospital stay, subjecting to a poor clinical outcome.
A definitive diagnosis is based on serological methods, but is usually clinical based on history of symptomatic varicella infection to mother or any other household contact [6]. The choice of investigation is rapid amplification of viral DNA in skin swabs by PCR (Polymerase Chain Reaction). The sensitivity of this is still found to be low. Enders G et al., were not able to detect virus in skin lesion of congenital varicella syndrome babies, even the varicella specific IgM marker was found only in 25% [7]. The lack of parents’ consent for the serological investigation caused a diagnostic handicap. The drug of choice for treatment of varicella is acyclovir with symptomatic treatment as per condition of the baby with recommended dose of 10 mg/kg/dose 8 hourly [8]. The use of VZIG is still controversial during full blown varicella disease. Its use is effective in newborn for perinatal varicella, when administered as soon the mother develops rash within two days of delivery. IVIG contains high titers of VZV-specific IgG and VZV antibodies have been shown to be equivalent [9]. The severity of disease can be reduced with VZIG and more, if given as soon as possible. In this case its non-availability and also late presentation to the hospital can be one of the reasons for progressive severity of varicella infection in the baby.
Conclusion(s)
Varicella is an infectious disease with grievous outcome in the newborn period when presented with rash after 12 days of postnatal life subjecting to poor outcomes due complications like pneumonia, hepatitis, bleeding diathesis and secondary severe sepsis.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes (from parents)
For any images presented appropriate consent has been obtained from the subjects. Yes (from parents)
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 19, 2019
Manual Googling: Dec 17, 2019
iThenticate Software: Dec 23, 2019 (5%)
[1]. Arvin A, Gershon A, Live attenuated varicella vaccineAnu Rev Microbiol 1996 50:09-100.10.1146/annurev.micro.50.1.598905076 [Google Scholar] [CrossRef] [PubMed]
[2]. Chapman SJ, Varicella in pregnancySemin Perinatal 1998 22:339-46.10.1016/S0146-0005(98)80023-2 [Google Scholar] [CrossRef]
[3]. Luchesi PF, La Bocetta AC, Peale AR, Varicella neonatorumAm J Dis Child 1947 73(1):44-54.10.1001/archpedi.1947.0202036005100420282145 [Google Scholar] [CrossRef] [PubMed]
[4]. Blumental S, Lepage P, Management of varicella in neonates and infantsBMJ Paediatrics Open 2019 3:e00043310.1136/bmjpo-2019-00043331263790 [Google Scholar] [CrossRef] [PubMed]
[5]. Gershon A, Chicken pox, measles and mumps. In: Remington J, Klein J, edsInfections of the fetus and newborn infant 2001 5th edPhiladelphiaSaunders:683-732. [Google Scholar]
[6]. Choudhary P, Singh A, Jain R, Mandal A, Late neonatal varicellaIndian J Paediatr Dermatol 2017 18:254-55.10.4103/2319-7250.206087 [Google Scholar] [CrossRef]
[7]. Enders G, Miller E, Cradock Watson J, Bolley I, Ridehalgh M, Consequences of varicella and herpes zoster in pregnancy: Prospective study of 1739 casesLancet 1994 343:1548-51.10.1016/S0140-6736(94)92943-2 [Google Scholar] [CrossRef]
[8]. Bhardwaj AK, Sharma PD, Sharma A, Neonatal varicella: A rare case reportAustralas Med J 2011 4(6):291-93.10.4066/AMJ.2011.68223386890 [Google Scholar] [CrossRef] [PubMed]
[9]. Paryani SG, Arvin AM, Koropchak CM, Dobkin MB, Wittek AE, Amylon MD, Comparison of varicella zoster antibody titres in patients given intravenous immune serum globulin of VZIGJ Pedatr 1984 105:200-05.10.1016/S0022-3476(84)80113-4 [Google Scholar] [CrossRef]